CT-based radiostereometric analysis for assessing midfoot kinematics: precision compared with marker-based radiostereometry
Magnus POULSEN 1,2, Are H STØDLE 1, Lars NORDSLETTEN 1,2, and Stephan M RÖHRL 1,2
1 Division of Orthopaedic Surgery, Oslo University Hospital Ullevål, Oslo; 2 Institute of Clinical Medicine, University of Oslo, Norway
Background and purpose — 3-dimensional midfoot motion is hard to evaluate in clinical practice. We present a new computed tomography (CT)-based radiostereometric analysis (CT-RSA) technique to examine in vivo midfoot kinematics during single-leg stance and compare it with marker-based radiostereometry (RSA).
Patients and methods — 8 patients were examined with bilateral non- and full-weight-bearing CT images of the midfoot. 1st tarsometatarsal motion was analyzed using a surface-registration technique (CT-RSA). As all patients had unilateral tantalum markers in the 1st cuneiform (C1) and 1st metatarsal (M1), comparison of precision with markerbased RSA was performed. CT-RSA precision was evaluated with surface registration of both C1–M1 bone and C1–M1 tantalum markers, while RSA precision was determined with C1–M1 markers only. Additionally, to remove motion bias, we evaluated intrasegmental CT-RSA precision by comparing proximal with distal part of M1.
Results — Under physical load, the primary movement for the 1st tarsometatarsal joint was M1 dorsiflexion (mean 1.4°), adduction (mean 1.4°), and dorsal translation (mean 1.1 mm). CT-RSA precision, using surface bone or markers, was in the range of 0.3–0.7 mm for translation and 0.6–1.6° for rotation. In comparison, RSA precision was in the range of 0.4–0.9 mm for translation and 1.0–1.7° for rotation. Finally, intrasegmental CT-RSA precision was in the range of 0.1–0.2 mm for translation and 0.4–0.5° for rotation.
Conclusion — CT-RSA is a valid and precise, non-invasive method to measure midfoot kinematics when compared with conventional RSA.
Citation: Acta Orthopaedica 2023; 94: 366–372. DOI: https://doi.org/10.2340/17453674.2023.16905.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-03-29. Accepted: 2023-06-16. Published: 2023-07-20.
Correspondence: japoul@ous-hf.no
MP, AHS, and SMR were responsible for the study concept, design, and acquisition of data. AHS recruited the patients. MP and SMR had full access to all data in the study and take responsibility for data integrity and the accuracy of data analysis. MP wrote the manuscript, and AHS, LN, and SMR contributed critical revisions and approved the final version.
The authors thank Oslo Metropolitan University, Faculty of Health Sciences, represented by Kari Gerhardsen Vikestad and Linn Bjerknes, for their assistance with the Cone-Beam CT examinations. Also, they thank the CIRRO radiographers Alexis Hinojosa and Mona Risdal, as well as research coordinator Marte Traae Magnusson, for their vital contribution to this study.
Handling co-editor: Bart Swierstra
Acta thanks Cyrus Brodén and Bart Kaptein for help with peer review of this manuscript.
Traditionally, foot kinematics have been studied using external skin markers on bony landmarks for optical detection [1,2]. With mobile articulations, such as the ankle and subtalar region, extensive research has been done, and their functional kinetics have been documented in detail [3,4]. However, for joints with little native movement, like the tarsometatarsal (TMT) joints, skin markers are inadequate to detect individual joint characteristics, and their articulations are generally combined in segments [5].
With well-established accuracy and precision, radiostereometric analysis (RSA) is considered the gold standard for in vivo implant migration analysis [6]. Additionally, comparable RSA precision has been documented for in vitro kinematic studies in joints with limited mobility [7,8]. However, for clinical kinematic studies, this high-level precision is generally not reproduced due to the natural segmental motion present in the examined joint [9-11]. Furthermore, RSA requires several unique entities, including surgically placed tantalum markers and specially trained staff. Computed tomography (CT) offers direct 3-dimensional data that can serve as a substitute for traditional markers [12]. Preliminary arthroplasty studies with CT-based surface registration have shown comparable results to marker-based RSA without significant loss of accuracy or precision [13-16]. With respect to arthrokinematic studies, CTbased radiostereometry (CT-RSA) is not dependent on tantalum markers and, with surface detection, it could offer an alternative method for precision evaluation. If CT-RSA proves to be a precise noninvasive method for joint motion assessment, it will be possible to perform this wherever a CT scanner is available.
In this study, we first describe the stepwise application of a new, CT-based surface registration technique (CT-RSA) for detecting in vivo midfoot kinematics under natural weightbearing conditions. Second, we evaluate the precision of different methods of CT-RSA and compare the results with precision from conventional marker-based RSA.
Patients and methods
Patient selection
8 patients, 4 women and 4 men (mean age 33 years, range 24–53), were enrolled from a previously published RSA study [10]. All patients had been treated for a unilateral Lisfranc injury with a temporary, motion-preserving osteosynthesis [17]. Tantalum markers (0.8 mm diameter) were perioperatively inserted into the medial cuneiform and the proximal part of the 1st metatarsal. Minimum post-surgical time before inclusion in the current study was 5 years. On the contralateral, healthy foot, none of the patients had any midfoot deformities, prior to foot surgery, or sequelae after a previous foot injury. This study was reported in accordance with the STARD guideline.
Marker-based RSA setup
RSA arrangement consisted of a uniplanar technique with 2 mobile X-ray tubes (GE Proteus XR/A system, Piscataway, NJ, USA) and exposure parameters of 150 kV and 6 mAs. We used a vertical sett calibration cage (Cage43, RSA Biomedical, Umeå, Sweden). Following the standardized RSA guidelines [18], quality control parameters were applied. An upper limit of 0.35 mm for the mean error of rigid body fitting was used to indicate tantalum marker stability. Likewise, to indicate good marker spread, each rigid body needed a condition number below the limit of 150. All marker-based RSA analyses were performed using the RSAcore software (Leiden, The Netherlands) (Figure 1).
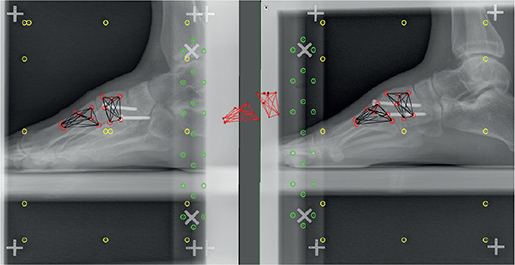
Figure 1. Radiostereometric analysis setup with tantalum markers in 1st cuneiform and 1st metatarsal.
CT setup
Cone-beam CT (CBCT) was used to acquire the CT images. CBCT utilizes a cone-shaped beam that captures the total volume of an image in 1 single rotation [19]. This offers high spatial resolution combined with rapid scanning, which is suitable for studying joint mobility [20]. In addition, CBCT technology facilitates low-dose radiation exposures with a maximum effective dosage of 6 μSv per scan when imaging the ankle region [21]. Each patient was examined using a portable CBCT unit (Verity, Planmed Oy, Helsinki, Finland) equipped with a 193 x 242 mm² flat panel detector. The CT scanner had a tube voltage of 96 kV, tube current of 9 mA, and CTDIvol 5.2 mGy. Metal artifact reduction was applied, and slices were reconstructed at 0.2 mm thickness at 1 mm increments.
Radiographic examinations
The RSA and the CT-RSA radiographs were performed in an identical manner. In this study, RSA was utilized as a precision measurement and not for motion detection. Single-leg stance was applied with non-weight-bearing and full-weightbearing settings. Each radiological series was performed with the patients standing upright and the examined foot placed flat in a forward-facing position (Figure 2). To facilitate natural weight-bearing conditions, patients were instructed to stand on a straight leg with evenly distributed weight on the entire examined foot. The contralateral leg was raised by 90-degree flexing of the knee while the hip remained outstretched. For the non-weight-bearing images, patients were instructed to lean back and place all body weight on the non-examined leg. Only the healthy, non-operated foot was used for motion analysis.

Figure 2. Single-leg stance, non-weight-bearing (A), and weight-bearing (B) images obtained on a portable cone-beam computed tomography machine.
Measuring joint motion with CT-RSA
To measure motion, acquired CT images were analyzed using a surface registration technique (CT-based Micromotion Analysis—CTMA, SECTRA, Linköping, Sweden). By mimicking RSA, it combines 2 low-dose CT scans separated by a provocation and quantifies the in vivo joint movement. Here we present the stepwise way in which our CT-RSA motion analyses of the 1st TMT joint was performed.
- CBCT images were uploaded to the CT-RSA server. The Hounsfield unit threshold of 150 was selected based on optimal bone registration and remained the same for all examinations.
- Using the non-weight-bearing images as primary (orange) and the weight-bearing images as secondary (blue), the anatomical segment of interest was registered manually (Figure 3). We marked the entire available area for each bone, whereas the software then produced 50,000 marker points on the surface for migration evaluation. The proximal 1st cuneiform (C1) was registered as the stationary object, and the distal 1st metatarsal (M1) was registered as the moving object.
- The software then calculated migration from the center-of-mass of M1 relative to the spatially aligned C1 from the non-weight-bearing images to the weight-bearing images. The degree of alignment was visualized with a 3-dimensional color-coded model with green, yellow, red, and blue indicating a shift of position of < 0.1 mm, 0.2 mm, 0.35 mm, and > 0.35 mm, respectively (Figure 3).
- Vectorial migration was expressed in 6 degrees of freedom representing translation (millimeters) and rotation (degrees) along the x, y, and z axis in a CT-based coordinate system (Figure 4). The interpretation of migration represents the inducible motion in the 1st TMT joint under physiological loading.
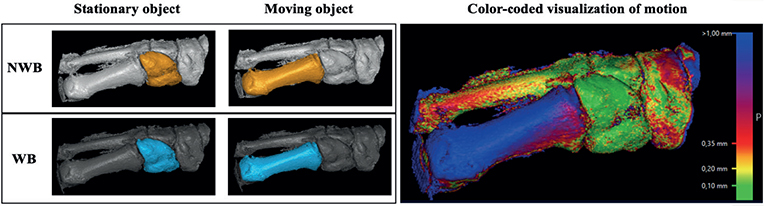
Figure 3. Measuring 1st TMT joint movement with CT-RSA using the CTMA software from Sectra. Depicting the 1st cuneiform as the stationary object and the 1st metatarsal as the moving object. Color-coded, overlapping images show the relative motion of the 1st metatarsal with the spatially aligned 1st cuneiform. Abbreviations: NWB: non-weight-bearing, WB: weight-bearing.
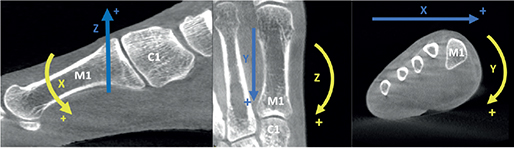
Figure 4. Movement vectors for the 1st metatarsal (M1) related to the 1st cuneiform (C1) on cone-beam CT images. The blue arrow represents translational migration, while the yellow arrow represents rotational migration.
Validating CT-RSA precision
First, we started by assessing RSA test precision, and sequential double examinations were performed. Here, precision is synonymous with repeatability and was defined as “the degree to which repeated measurements under unchanged conditions show the same results” [22]. For precision evaluation, paired double examinations of both non-weight-bearing and weight-bearing images were used (n = 16). Again, it should be noted that in this study, marker-based RSA was used only for precision comparison. The RSA coordinate system for migration was altered to match that of CT-RSA for comparison.
Thereafter, in a stepwise manner as with our RSA analysis, CT-RSA precision was evaluated through double examinations. Here we tested 3 different methods of surface registration. First, we surface-mapped the entire bone surface of C1 and compared it with the entire M1 surface. Both feet for each patient were used for this analysis (n = 32) (Figure 5A). Because the CT-RSA software allows for surface detection of metal objects, we changed the HU units to metal window registration (HU 2200) and also surface-mapped the tantalum markers in C1 and compared them with the markers in M1. Only the foot with surgically placed markers was used for this analysis (n = 16) (Figure 5B). CT offers direct 3-dimensional data, and the CT-RSA software is not restricted to specific markers for data tracking. Therefore, subsequent measurements within a bone segment without motion, for any movement above zero, will represent a measurement error. Thus, for our 3rd test of precision, surface detection of the proximal one-third of M1 was compared with the distal one-third of the same metatarsal bone (intrasegmental). A defined area between mapping segments was left unregistered to prevent overlapping surface detection. Intrasegmental precision was evaluated on both feet (n = 32) (Figure 5C).
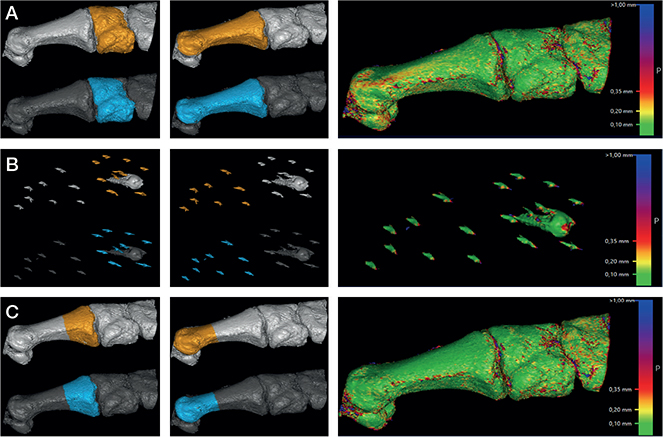
Figure 5. Different surface mapping methods for CT-RSA precision analysis. A: Bone surface of C1 vs. M1. B: Tantalum markers of C1 vs. M1. C: Proximal part of 1st MT vs. distal part of 1st MT (intrasegmental).
Statistics
RSA parameters were given with mean values, standard deviation (SD), and total range. To determine RSA and CT-RSA precision, double examination results were expressed as 1.96 x SD. All methods of precision showed a bell-shaped curve when visualized in a histogram, meaning normal distribution was assumed. Given the small sample size, no statistical tests were used to compare precision modalities. Motion analysis of the 1st TMT joint is presented for each patient with mean values and SD. All statistical data analyses were performed using STATA (version 17.0, StataCorp, College Station, TX, USA).
Ethics, funding, and disclosures
The National Ethical Board (REK) approved the study (Dnr 2011/1582), and all patients signed an informed consent form before enrollment. The study was supported by Oslo University Hospital. However, the supporting organization had no role in the design and conduct of the study. All authors declare no competing interests. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.16905
Results
Marker-based RSA analysis
The mean number of tantalum markers in C1 was 6.5 (SD 0.7, range 6–8) and 7.1 (SD 1.5, range 5–9) in M1. Using the RSA control parameters, none of the examinations were excluded from the study based on high condition number or mean error exceeding the recommendations by the RSA guidelines [18]. The mean condition number in C1 was 86 (SD 17, range 55–129) and 80 (SD 18, range 53–110) for M1. Furthermore, the mean error of rigid body fitting for C1 was 0.13 (SD 0.08, range 0.02–0.34) and 0.12 (SD 0.08, range 0.03–0.34) for M1. Precision for RSA in this cohort measured in the range of 0.39–0.94 mm for translation and 1.0–1.7° for rotation (Table 1).
CT-RSA analysis
3 different methods of CT-RSA precision analysis were performed (Table 1). Methods 1 and 2 rely on segmental surface registration of bone and markers in C1 and M1, respectively. Here precision for translation was in the range of 0.33–0.70 mm for surface bone and 0.37–0.64 mm for tantalum markers. Likewise, the precision for rotation was 0.70–1.5° for bone and 0.62–1.7° for markers. The intrasegmental precision measured in the range of 0.19–0.23 mm for translation and 0.39–0.56° for rotation.
TMT motion
For comparison purposes, left foot results were altered to match that of a right foot alignment. Using our intrasegmental precision as an indicator for minimum detectable change, all patients had some degree of observed midfoot motion. Under physical load, the primary movement for the 1st TMT joint was observed through M1 dorsiflexion (mean 1.4°), adduction (mean 1.4°), and dorsal translation (mean 1.1 mm) (Table 2).
| Patient | Translation (mm) | Rotation (°) | ||||
| X | Y | Z | X | Y | Z | |
| 1 | 0.2 (0.1) | −1.0 (0.2) | 2.0 (0.3) | −1.7 (0.2) | −3.0 (0.4) | 0.8 (0.4) |
| 2 | 2.7 (0.2) | 0.6 (0.1) | 1.0 (0.3) | −2.5 (0.1) | 1.1 (0.5) | 5.1 (0.1) |
| 3 | 1.0 (0.0) | 0.2 (0.0) | 0.2 (0.0) | −0.9 (0.1) | 1.4 (0.1) | 2.0 (0.2) |
| 4 | 0.4 (0.1) | −0.6 (0.0) | 1.1 (0.1) | −0.7 (0.1) | −1.0 (0.2) | −0.1 (0.0) |
| 5 | 1.9 (0.1) | −0.7 (0.2) | 1.8 (0.1) | −2.1 (0.2) | −2.7 (0.2) | 2.1 (0.3) |
| 6 | 0.5 (0.3) | −0.3 (0.2) | 1.2 (0.4) | −1.4 (0.3) | 0.1 (0.4) | 0.1 (0.5) |
| 7 | 0.4 (0.2) | −0.5 (0.1) | 1.0 (0.2) | −1.0 (0.2) | −0.8 (0.1) | 0.6 (0.4) |
| 8 | 0.7 (0.2) | −0.3 (0.1) | 0.8 (0.0) | −1.0 (0.0) | −0.7 (0.2) | 0.8 (0.2) |
| Mean | 1.0 (0.8) | −0.3 (0.5) | 1.1 (0.5) | −1.4 (0.6) | 0.7 (1.5) | 1.4 (1.6) |
| For direction of migration (+/−), see Table 1. | ||||||
Discussion
We describe a CT-based surface registration technique to evaluate in vivo midfoot motion. The 1st TMT joint moved primarily in dorsiflexion, adduction, and dorsal translation under natural weight-bearing conditions. We showed that the precision of our CT-RSA measurements was directly comparable to marker-based RSA, thus being the first to investigate method agreement between the 2 techniques in a kinematic study.
Precision is a benchmark indicator for method validation. Not only does it signify variability in repeated examinations, but it also evaluates the random error present in your measurements [23]. Factually, marker-based RSA is considered the most accurate and precise method available to measure orthopedic implant migration [6,18]. When using double examination measurements in experimental phantom settings, RSA test precision shows remarkably good values [24]. However, precision tends to vary when the same repeated approach is used in a clinical setting, with values ranging between 0.15–0.60 mm for translation and 0.3–2.0° for rotation being considered acceptable [6]. Furthermore, when one evaluates precision in a kinematic-based RSA study, with tantalum markers present on both sides of a joint, precision can show even greater variability. This is the inevitable result of micromotion occurring between the 2 jointed segments in between double examinations. The RSA precision values in the present study ranged from 0.39–0.94 mm for translation and 1.0–1.7° for rotation. These results are fitting for the study setup and in accordance with previously published equivalent studies [9,10,25]. To further substantiate our results, the RSA control parameters indicate stable and consistent tantalum markers valid for reliable precision measurements.
Consequently, new migration techniques should be compared for validation, with RSA being the current gold standard [18]. Therefore, to evaluate the relative precision of the new CT-RSA method, an identical experimental setup was performed. First, because CT-RSA offers surface registration of both bone and tantalum markers, the 2 intersegmental methods were matched and showed an excellent level of agreement. In this study, using surface anatomy of bone or markers did not influence the outcome. Second, the results were compared with marker-based RSA findings and likewise indicated similar results between the 2 modalities. Additionally, by applying an intrasegmental approach to measure CT-RSA precision, one removes the inevitable bias caused by involuntary joint motion and can assume that there is zero motion present between the double examinations. By doing so, our intrasegmental precision yielded results in the same range as previously published arthroplasty studies [13-16], e.g., Brodén et al., who compared CT-RSA with RSA precision in cemented acetabular cups [13]. Here, CT-RSA precision was reported as below 0.16 mm for translation and below 0.37° for rotation and was directly comparable with their matching RSA results. Likewise, these authors also found similar results when measuring migration in shoulder arthroplasty with the same study setup [15]. However, no previous kinematic studies have compared the precision of CT-RSA with marker-based RSA. In addition, this is the first CT-RSA study to use intrasegmental precision evaluation. We would advocate that this should be the preferred method to evaluate test precision in future kinematic CT-RSA studies. Furthermore, for studies relying on provocation, our intrasegmental approach can be applied to the before and after scans enabling precision to be analyzed without the obligation of double examinations, consequently halving the effective radiation dosage for our patients.
Combining low-dose, weight-bearing CT images with surface registration software is a noninvasive method for examining joint kinematics. Other similar noninvasive methods include fast-phase contrast MRI imaging and the Dual Fluoroscopic Imaging System (DFIS), which utilize specialized radiological equipment and are generally limited to a research approach [26,27]. Furthermore, as is the case with external skin markers, these methods are inappropriate for clinical decisionmaking for patients with foot impairments. In our study, the induced 1st TMT joint movement is analyzed under natural weight-bearing conditions. Nonetheless, the technique is applicable to all joints in the human body, whether it be to measure normal motion or to provoke a joint to evaluate ligamentous pathology. Studies on midfoot kinematics generally depict sagittal motion as the main directional movement [1,28]. We also observed largest motion in the sagittal plane. However, an almost equal motion was observed in 1st metatarsal adduction, as well as sagittal translation. This result indicates the complexity of the 1st TMT joint and its tri-planar characteristics during weight-bearing. The average degree of total dorsiflexion in the 1st TMT joint has been described in the literature as approximately 5° [28,29]. With our test subjects, the mean dorsiflexion was 1.4°, indicating that our single-leg stance might have been a poor method to elicit midfoot motion.
In contrast to the specially designed equipment and skilled personnel that conventional RSA requires, CT-RSA introduces a substitutional method of motion detection that necessities only a CT scanner, commonly present in most clinics and hospitals. It has the advantage of observing subtle movements under natural conditions and, if preferred, can be applied to multiple joints within the CT scan field of view. Having a validated joint motion tool is especially important in a clinical setting, where altered kinematics, which may indicate stabilizing ligament injury, can be directly compared with the corresponding healthy foot. Furthermore, radiological studies that measure pathological differences often rely on independent assessments of the examiners by comparing inter- and intraobserver reliability. Having a validated, precise motion tool present, CT-RSA can serve as a reference template for evaluating manual motion measurements on radiological images.
Limitations
This is an exploratory study with a small sample size; therefore the results should be viewed with precaution. Normally when determining RSA precision, it is assumed that there is no movement present between the objects. In a kinematic-based study with 2 movable segments, this assumption is not valid, and the true test precision cannot be ascertained. However, our intrasegmental precision method with CT-RSA resolves this issue. CT-RSA uses surface anatomy on a 3-dimensional model for motion detection. This means that target areas must be registered manually, a process that is both time-consuming and relies on user experience. The method also uses static images to evaluate the shift in position of a target bone relative to a spatially aligned bone. It does not depict the complete range of movement of that given joint during a dynamic activity, such as walking, running, or jumping. Furthermore, if used in clinical practice for foot and ankle pathology, one preferably needs a CT machine that allows for weight-bearing imaging. And if comparing bilateral images, an additional CT scan must be taken on a healthy extremity, which inflicts additional radiation dosage on the patient.
Conclusion
The use of weight-bearing, cone-beam CT imaging combined with a surface registration technique (CT-RSA) is applicable to motion analysis of the midfoot. It offers an encouraging method to detect both normal and pathological joint motion in clinical practice. In addition, for future kinematic CT-RSA studies, an intrasegmental approach to determine test precision should be considered.
- Nester C J, Jarvis H L, Jones R K, Bowden P D, Liu A. Movement of the human foot in 100 pain free individuals aged 18–45: implications for understanding normal foot function. J Foot Ankle Res 2014; 7: 51. doi: 10.1186/s13047-014-0051-8.
- Deschamps K, Staes F, Roosen P, Nobels F, Desloovere K, Bruyninckx H, et al. Body of evidence supporting the clinical use of 3D multisegment foot models: a systematic review. Gait Posture 2011; 33: 338-49. doi: 10.1016/j.gaitpost.2010.12.018.
- Kitaoka H B, Crevoisier X M, Hansen D, Katajarvi B, Harbst K, Kaufman K R. Foot and ankle kinematics and ground reaction forces during ambulation. Foot Ankle Int 2006; 27: 808-13. doi: 10.1177/107110070602701010.
- Jastifer J R, Gustafson P A. The subtalar joint: biomechanics and functional representations in the literature. Foot 2014; 24: 203-9. doi: 10.1016/j.foot.2014.06.003.
- Schallig W, van den Noort J C, McCahill J, Stebbins J, Leardini A, Maas M, et al. Comparing the kinematic output of the Oxford and Rizzoli Foot Models during normal gait and voluntary pathological gait in healthy adults. Gait Posture 2020; 82: 126-32. doi: 10.1016/j.gaitpost.2020.08.126.
- Kärrholm J. Roentgen stereophotogrammetry: review of orthopedic applications. Acta Orthop Scand 1989; 60: 491-503. doi: 10.3109/17453678909149328.
- Kibsgård T J, Røise O, Stuge B, Röhrl S M. Precision and accuracy measurement of radiostereometric analysis applied to movement of the sacroiliac joint. Clin Orthop Relat Res 2012; 470(11): 3187-94. doi: 10.1007/s11999-012-2413-5.
- Beumer A, Valstar E, Garling E, Niesing R, Ranstam J, Löfvenberg R, et al. Kinematics of the distal tibiofibular syndesmosis. Acta Orthop Scand 2003; 74: 337-43. doi: 10.1080/00016470310014283.
- Martinkevich P, Rahbek O, Møller-Madsen B, Stilling M. Calcaneal cuboid joint motion and osteotomy stability in children one year after calcaneal lengthening osteotomy. J Orthop 2020; 22: 565-70. doi: 10.1016/j.jor.2020.11.001.
- Poulsen M, Stødle A H, Nordsletten L, Röhrl S M. Does temporary bridge plate fixation preserve joint motion after an unstable Lisfranc injury? Foot Ankle Surg 2023; 29: 151-7. doi: 10.1016/j.fas.2022.12.007.
- Humadi A, Dawood S, Halldin K, Freeman B. RSA in spine: a review. Global Spine J 2017; 7: 811-20. doi: 10.1177/2192568217701722.
- Eriksson T, Maguire G Q, Noz M E, Zeleznik M P, Olivecrona H, Shalabi A, et al. Are low-dose CT scans a satisfactory substitute for stereoradiographs for migration studies? A preclinical test of low-dose CT scanning protocols and their application in a pilot patient. Acta Radiol 2019; 60: 1643-52. doi: 10.1177/0284185119844166.
- Brodén C, Sandberg O, Olivecrona H, Emery R, Sköldenberg O. Precision of CT-based micromotion analysis is comparable to radiostereometry for early migration measurements in cemented acetabular cups. Acta Orthop 2021; 92: 419-23. doi: 10.1080/17453674.2021.1906082.
- Brodén C, Sandberg O, Sköldenberg O, Stigbrand H, Hänni M, Giles J W, et al. Low-dose CT-based implant motion analysis is a precise tool for early migration measurements of hip cups: a clinical study of 24 patients. Acta Orthop 2020; 91: 260-5. doi: 10.1080/17453674.2020.1725345.
- Brodén C, Giles J W, Popat R, Fetherston S, Olivecrona H, Sandberg O, et al. Accuracy and precision of a CT method for assessing migration in shoulder arthroplasty: an experimental study. Acta Radiol 2020; 61: 776-82. doi: 10.1177/0284185119882659.
- Angelomenos V, Mohaddes M, Itayem R, Shareghi B. Precision of low-dose CT-based micromotion analysis technique for the assessment of early acetabular cup migration compared with gold standard RSA: a prospective study of 30 patients up to 1 year. Acta Orthop 2022; 93: 459-65. doi: 10.2340/17453674.2022.2528.
- Stødle A H, Nilsen F, Molund M, Ellingsen Husebye E, Hvaal K. Open reduction and internal fixation of acute Lisfranc fracture-dislocation with use of dorsal bridging plates. JBJS Essent Surg Tech 2019; 9: e39. doi: 10.2106/jbjs.st.19.00009.
- Valstar E R, Gill R, Ryd L, Flivik G, Börlin N, Kärrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76: 563-72. doi: 10.1080/17453670510041574.
- Posadzy M, Desimpel J, Vanhoenacker F. Cone beam CT of the musculoskeletal system: clinical applications. Insights Imaging 2018; 9: 35-45. doi: 10.1007/s13244-017-0582-1.
- Tuominen E K J, Kankare J, Koskinen S K, Mattila K T. Weight-bearing CT imaging of the lower extremity. AJR Am J Roentgenol 2013; 200: 146-8. doi: 10.2214/AJR.12.8481.
- Koivisto J, Kiljunen T, Kadesjö N, Shi X-Q, Wolff J. Effective radiation dose of a MSCT, two CBCT and one conventional radiography device in the ankle region. J Foot Ankle Res 2015; 8: 8. doi: 10.1186/s13047-015-0067-8.
- Sköldenberg O, Eisler T, Stark A, Muren O, Martinez-Carranza N, Ryd L. Measurement of the migration of a focal knee resurfacing implant with radiostereometry. Acta Orthop 2014; 85: 79-83. doi: 10.3109/17453674.2013.869654.
- Niesen A E, Hull M L. Measurement error versus repeated measurements: a guide describing two methods for computing bias and precision of migration measurements from double examinations using radiostereometric analysis. J Biomech Eng 2022; 144(6): 061011 doi: 10.1115/1.4054375.
- Bragdon C R, Malchau H, Yuan X, Perinchief R, Kärrholm J, Börlin N, et al. Experimental assessment of precision and accuracy of radiostereometric analysis for the determination of polyethylene wear in a total hip replacement model. J Orthop Res 2002; 20: 688-95. doi: 10.1016/S0736-0266(01)00171-1.
- Martinkevich P, Rahbek O, Møller-Madsen B, Søballe K, Stilling M. Precise and feasible measurements of lateral calcaneal lengthening osteotomies by radiostereometric analysis in cadaver feet. Bone Joint Res 2015; 4(5): 78-83. doi: 10.1302/2046-3758.45.2000292.
- Ye D, Sun X, Zhang C, Zhang S, Zhang X, Wang S, et al. In vivo foot and ankle kinematics during activities measured by using a dual fluoroscopic imaging system: a narrative review. Front Bioeng Biotechnol 2021; 9: 693806. doi: 10.3389/fbioe.2021.693806.
- Sheehan F T, Seisler A R, Siegel K L. In vivo talocrural and subtalar kinematics: a non-invasive 3D dynamic MRI study. Foot Ankle Int 2007; 28: 323-35. doi: 10.3113/FAI.2007.0323.
- Lundgren P, Nester C, Liu A, Arndt A, Jones R, Stacoff A, et al. Invasive in vivo measurement of rear-, mid- and forefoot motion during walking. Gait Posture 2008; 28: 93-100. doi: 10.1016/j.gaitpost.2007.10.009.
- Whittaker E C, Aubin P M, Ledoux W R. Foot bone kinematics as measured in a cadaveric robotic gait simulator. Gait Posture 2011; 33: 645-50. doi: 10.1016/j.gaitpost.2011.02.011.