Epidemiology and risk factors for premature physeal closure in distal femur fractures
Sini-Tuuli KOIVISTO 2,4, Topi LAAKSONEN 1,4, Ilkka HELENIUS 1,3,4, Henri VASARA 3,4, and Antti STENROOS 1,4
1 Department of Pediatric Orthopaedics and Traumatology, University of Helsinki and Helsinki New Children’s Hospital, Helsinki; 2 University of Helsinki, Faculty of Medicine, Helsinki; 3 Department of Orthopaedics and Traumatology, University of Helsinki and Helsinki University Hospital, Helsinki; 4 Finnish Pediatric Orthopaedics Research Group (FIPO), Helsinki, Finland
Background and purpose — Premature physeal closure (PPC) is a common and concerning complication to distal femoral fractures as the distal growth plate accounts for 70% of the growth of the femur. The literature is not unanimous in determining the risk factors of PPC, and the epidemiological characterization of these fractures is limited. Our aim was to calculate the population-based incidence and investigate risk factors for PPC in these fractures.
Patients and methods — In this register-based study, between 2014 and 2021, 70 children with distal femoral physeal fractures presented to our hospital. Demographic data, and fracture- and treatment-related details were collected using the Kids’ Fracture Tool. A directed acyclic graph (DAG) was constructed to determine confounding factors used in the risk analysis.
Results — Physeal fractures of the distal femur occurred with an annual incidence of 6/105 children, and a resulting PPC occurred in 16/70 (23%) with an annual incidence of 1.3/105 children. In multivariable analysis, dislocation exceeding 10 mm was a risk factor for PPC (OR 6.3, CI 1.4-22).
Conclusion — One-fourth of distal femoral physeal fractures developed PPC. Greater dislocation and higher injury energy were significant risk factors, whereas choice of fracture treatment was not an independent risk factor. All patients with PPC belonged in the age group 11–16 years.
Citation: Acta Orthopaedica 2023; 94: 348–353. DOI: https://doi.org/10.2340/17453674.2023.13654.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-15. Accepted: 2023-05-29. Published: 2023-07-12.
Correspondence: ilkka.helenius@hus.fi
S-TK: study design, data acquisition, manuscript preparation. TL: study design, data acquisition, manuscript preparation. HV: study design, manuscript preparation. IH: study design, manuscript preparation. AS: study design, data acquisition, manuscript preparation.
Handling co-editors: Ivan Hvid and Robin Christensen
Acta thanks Torsten Backteman, David Little, and Søren Kold for help with peer review of this manuscript.
Physeal fractures of the distal femur are infrequent fractures in children, accounting for 0.3–1.4% of all physeal fractures in children [1-3]. Mechanism of injury often involves high-energy trauma, with the most common injury mechanisms being motor vehicle accidents (MVA), sports-related accidents, and falls [4-6]. The fractures exhibit exceptionally high complication rates, most commonly premature physeal closure (PPC), which has been reported to occur in up to 21–35% of patients [4-8].
A number of predictive factors have been assessed for the development of PPC, and predictive factors that have shown statistical significance in some studies include Salter-Harris classification, age, dislocation, surgical fixation techniques, and treatment strategy (surgical vs. conservative) [4,6,9-11].
Being rare, the epidemiological data on these fractures is limited, and the literature is not unanimous in determining predictive factors for PPC of the distal femur [5,7,8,11,12]. We aimed to estimate the population-based incidence, characterize the epidemiology, and evaluate predictive factors of PPC in distal femur fractures in children. We hypothesized that physeal fracture classification, primary dislocation, and choice of treatment would be risk factors for PPC.
Patients and methods
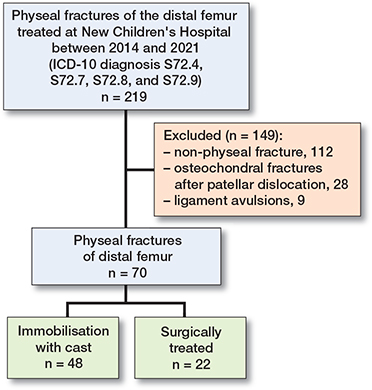
New Children’s Hospital is the only tertiary level hospital in the Helsinki capital area and the only hospital providing oncall pediatric orthopedic treatment in Finland. We performed a register-based study including all children (< 16 years old) who presented with a physeal fracture of the distal femur. Patients were identified using the Kids’ Fracture Tool, which is an electronic pediatric fracture register (New Children’s Hospital, Helsinki, Finland, and BCB Medical, Turku, Finland) where all children’s fractures have been collected and evaluated prospectively in Helsinki area since 2014. The patient’s data is entered into the registry when the patient is admitted to the emergency room, and additional data on treatment and recovery is added at all phases of treatment. The information added to the registry is futhermore revised by a pediatric orthopaedic surgeon and a radiologist. 70 consecutive distal femoral physeal fractures treated at New Children’s Hospital between 2014 and 2021 were identified (Figure 1). Physeal fractures were classified according to Peterson [13] (Figure 2), and all patients had a minimum of 6 months of radiographic follow-up.
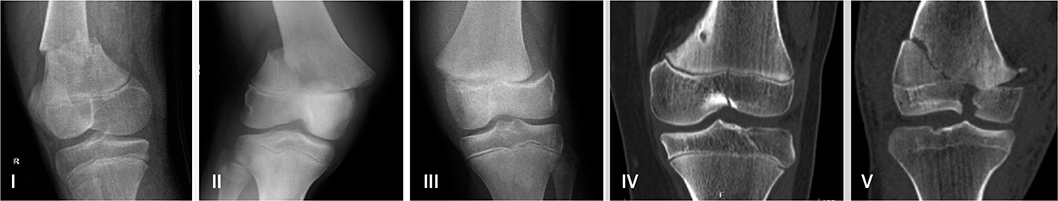
Figure 2. Demonstrative radiographs describing the Peterson fracture classification.
Demographic data including age, sex, mechanism of injury, site of the fracture, and associated injuries was registered from the Kids’ Fracture Tool and patient medical records [14]. Fracture morphology and degree of dislocation in anteroposterior (AP) and sagittal planes were recorded from primary radiographs. Both the proportional size in relation to physeal width (%) and absolute (mm) size of the Thurstan–Holland fragment were registered. Fracture energy was registered in 3 categories: low-energy, moderate energy, and high-energy fractures. Fractures estimated to have injury energy equivalent to falling at ground-level were classified as low-energy fractures, while those estimated to have injury energy equivalent to a motor vehicle accident (MVA) of under 30 km/hour, bike accident, or falling from a moderately elevated setpoint were classified as moderate energy fractures. High-energy fractures were estimated to have injury energy equivalent to an MVA of over 30 km/hour or falling from a substantial height (> 3 m).
Method of treatment, number of procedures, surgical methods (closed vs. open reduction; type of osteosynthesis), hospitalization period, and immobilization type and length were registered from the Kids’ Fracture Tool and patient medical records. Fracture- and treatment-related complications were also recorded. Development of PPC was evaluated from follow-up radiographs and CT images. PPC was defined as the presence of a physeal bar/bony bridge on CT in patients with no signs of normal physiological physiodesis. Patients undergoing lateral plate fixation over the physeal line were not included in the premature physeal closure group as all these patients were reaching skeletal maturity at the time of initial fracture treatment.
Statistics
The number of under 16-year-old children during the study period was collected from the statistical yearbooks of Helsinki [15] to calculate a population-based annual incidence of physeal fractures. Patients with missing data were excluded from analysis. Categorical variables were presented in counts and percentages. For risk factor analysis, we first performed univariate binary logistic regression analysis, after which potential variables were selected for the multivariate logistic regression analysis. Odds ratios with 95% confidence intervals (CI) were calculated for each risk factors. A directed acyclic graph (DAG) was created to demonstrate causal pathways and to reduce bias in covariate selection, for which we used DAGitty 3.0 software (available at https://dagitty.net. Released January 9, 2019). We selected covariates according to a method proposed by Shrier and Platt [16], and separate multivariable models were performed for each tested variable based on the DAG. SPSS 27.0.1 (IBM Corp, Armonk, NY, USA; released November 3, 2020) was used for the statistical analysis, and p-values of less than 0.05 were considered statistically significant. This article was reported in accordance with the STROBE guidelines.
Ethics, funding, and disclosures
The study protocol was approved by the Helsinki University Hospital Review Board (Dnr 365/13/03/03/2015). The authors declare no conflicts of interest and received no funding for the research and/or publication of this article. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.13654
Results
During the study period, 70 children with physeal distal femoral fractures presented to our clinic, with a median age of 11.0 years (range 0.4–15.8), resulting in a population-based annual incidence of 6/105 (CI 5.6–6.8) children. 50/70 (71%) of fractures were sustained in boys, yielding a ratio of 2.5:1.
Most fractures resulted from traffic accidents 17/70 (24%), followed by falls on the same level 14/70 (20%), and trampolines 12/70 (17%). 9/70 (13%) fractures were sustained by children with an illness affecting normal musculoskeletal integrity, and the injury mechanism was unknown in 3 of them (Table 1). Patients were transported to the hospital by ambulance in 42/70 (60%) cases (Table 1). 11/70 (16%) patients suffered other fractures at the time of injury.
| Fractures | n | % | Median age (range) | Mechanism of injury | Injury energy | Associated injuries | |||||||
| Fall from | Traffic | Trampoline | Sport | Other | |||||||||
| same | height | Low | Moderate | Severe | |||||||||
| Peterson I | 11+2 a | 19 | 5.1 (0.4–13.6) | 5 | 1 | 4 | 3 | 10 | 2 | 1 | |||
| Peterson II | 33+7 a | 57 | 10.3 (0.7–15.8) | 7 | 3 | 5 | 7 | 11 | 4+3 b | 25 | 12 | 3 | 2 |
| Peterson III | 4 | 6 | 15.0 (11.9–15.2) | 3 | 1 | 1 | 3 | 1 | |||||
| Peterson IV | 4 | 6 | 12.2 (9.8–14.8) | 1 | 3 | 1 | 3 | 3 | |||||
| Peterson V | 9 | 13 | 15.1 (12.4–15.7) | 1 | 2 | 5 | 1 | 1 | 3 | 5 | 5 | ||
| Total | 70 | 100 | 10.8 (0.4–15.8) | 14 | 5 | 17 | 12 | 12 | 7+3 b | 38 | 17 | 15 | 11 |
| a 9 children had an illness affecting normal musculoskeletal integrity. b Exact injury mechanism could not be expressed by parents in 3 children and were presumably sustained in a low-energy injury setting, as all 3 patients were either infants or in a wheelchair. |
|||||||||||||
Peterson II (40/70) was the most common fracture type (Table 1). There was an increasing trend in the children’s age according to Peterson classification (P < 0.001). Peterson I and II fractures were more likely to be sustained in low to moderate injury energy settings, while Peterson fractures III–V occurred only in older children and had more severe injury energy (P < 0.001).
5/70 (7.1%) had fracture reduction done before the first radiographic examination. In the primary radiographs, 42/70 (60%) fractures were minimally displaced (≤ 2 mm). 28/70 (40%) fractures were displaced (> 2 mm): 15/28 in both coronal and sagittal planes, 6/28 in the coronal plane only, and 7/28 in the sagittal plane only. Posterior displacement was most common (n = 17), followed by valgus (n = 14), varus (n = 7), and anterior displacement (n = 5). The median coronal displacement was 15 mm (range 3–91), and the median sagittal displacement was 5 mm (range 3–57). The median size of the Thurstan–Holland fragment was 16 mm (range 4–55), representing 29% (range 7–74) of the physeal width in the coronal view.
All patients were treated within 24 hours from the injury. 48/70 (69%) were treated conservatively with a cast: 42 cast in situ, 4 with reduction and cast, and 2 with manipulation under anesthesia. These patients had a median coronal and sagittal displacement of 1 mm (ranges 0–11 and 0–10) in relation to the physis. The surgically treated group had a median coronal displacement of 14 mm (range 0–91) and sagittal displacement of 5 mm (range 0–57). Peterson classification reflected treatment strategy as well as injury energy (Figure 3).
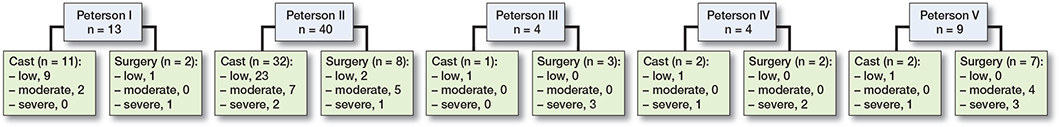
Figure 3. Peterson fractures’ treatment distribution and reported injury energies in each treatment class.
During the follow-up, physeal closure was noted in 24/70 (34%) patients. 16/70 (23%) were diagnosed with PPC, while in 8 children, the physeal closure was deemed physiological. Of the 16 children diagnosed with PPC, 8 had a surgical intervention to impede either angular deformity or leg length. The median age of these 16 patients at the time of the fracture was 14 years (range 11.7–15.3). The population-based incidence of distal femur PPC was 1.3/105 children (Table 2, see Appendix).
Only 1 patient developed a clinically significant leg length discrepancy and was surgically treated with limb-lengthening surgery 42 months after the injury (Patient 8, Table 2, see Appendix)). 6 patients were treated with contralateral epiphysiodesis and 1 with epiphysiodesolysis (Patients 1–7, Table 2, see Appendix)). No corrective osteotomies were done. The remaining 8 children with PPC had too little growth left to develop a clinically significant deformity (Patients 9–16, Table 2, see Appendix)).
A directed acyclic graph was constructed to demonstrate the causal pathways and to identify confounders and reduce bias in covariate selection (Figure 4). The results of the univariable analysis are presented in Table 3. In the multivariable analysis, dislocation in the primary radiographs (> 10 mm) was a significant risk factor for PPC (OR 6.3, CI 1.4–22). There were no neurovascular injuries or compartment syndromes in this cohort.
| Factor | PPC a | Odds ratio (CI) | P value |
| Age at time of injury | |||
| 0–5 | 0/18 (0) | Reference | |
| 6–10 | 0/12 (0) | 1 | |
| 11–16 | 16/24 (40) | 1.07e+9 | |
| Injury energy: | |||
| Low | 2/36 (5.3) | Reference | |
| Moderate | 7/10 (41) | 13 ( 2.5–70) | 0.004 |
| High | 7/8 (47) | 16 (2.7–90) | 0.002 |
| Primary treatment | |||
| New Children’s’ Hospital | 9/33 (21) | Reference | |
| Secondary care clinics | 7/19 (27) | 1.3 (0.4–4.2) | 0.01 |
| Private clinics | 0/2 (0) | 0 | |
| Peterson fracture class | |||
| I | 0/13 (0) | Reference | |
| II | 9/31 (23) | 3.4 (0.3–30) | 0.2 |
| III | 3/1 (75) | 36 (1.7–757) | 0.02 |
| IV | 0/4 (0) | 0 | |
| V | 4/5 (44) | 9.6 (0.8–108) | 0.06 |
| Dislocation b | |||
| 0–2 mm | 3/46 (6.1) | Reference | |
| 2–10 mm | 2/5 (29) | 6.1 (0.8–45) | 0.07 |
| >10 mm | 11/3 (79) | 26 (9.9–117) | < 0.001 |
| Number of reduction attempts | |||
| 1 | 9/49 (16) | Reference | |
| 2 | 7/3 (70) | 13 (2.7–58) | 0.001 |
| 3 | 1/1 (50) | 5.4 (0.3–95) | 0.2 |
| Treatment method | |||
| Cast in situ | 2/40 (4.8) | Reference | |
| Closed reduction and cast | 0/6 (0) | 0 | |
| Osteosynthesis | 14/8 (64) | 35 (6.6–184) | < 0.001 |
| Surgeon status | |||
| Resident | 1/29 (3.3) | Reference | |
| Fellow | 9/17 (35) | 15 (1.7–132) | 0.1 |
| Consultant | 6/8 (43) | 22 (2.2–207) | 0.007 |
| a Number of adverse events/predisposed (% adverse events of total) b Maximum dislocation on either the AP or lateral primary radiographs. |
|||
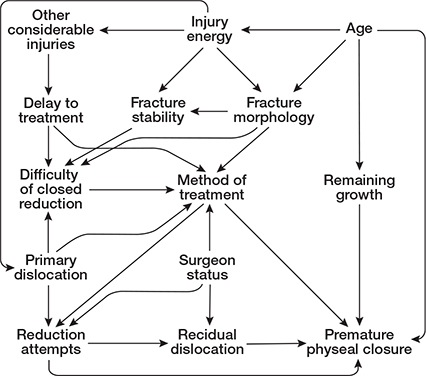
Figure 4. Demonstration of causal pathways behind PPC.
Discussion
Aim of this study
We found an annual incidence of 6/105 children, which to the best of our knowledge has not been previously reported. One-fourth of these children developed PPC despite treatment within 24 hours, giving an estimated annual incidence of 1.3/105 children. Lower trauma energy was associated with lower Peterson classification. Those treated surgically were older, had more likely sustained higher energy injuries, and had larger dislocation. Primary dislocation (> 10 mm) and higher injury energy were statistically significant risk factors for PPC, and all patients with PPC were in the age group 11–16 years.
Comparisons
Consistent with earlier reports, PPC following physeal fracture was not uncommon, occurring in 23% of cases (16/70), compared with the most recent reports of 21–35% [4-8]. In support of our findings, Bellamy et al. and Garret et al. found higher fracture energies to be associated with physeal bar formation [7,8]. The degree of dislocation in the predicament of complications is also supported by other authors [9,11,12]. Fracture energy and dislocation are closely related and seem intuitive as predictive factors for PPC, as high-energetic and dislocated fractures are more likely to cause more extensive physeal injury and disruption of physeal vasculature, which could contribute to the development of PPC.
The number of reduction attempts has been suggested as a risk factor for PPC. The number of patients with multiple attempts was low and statistical conclusions could not be made. Of note, consultant surgeon status statistically correlated with the development of PPC. However, this could be attributable to selection bias as the more experienced surgeons are more likely to operate on the more challenging trauma patients with higher injury energy and more dislocation, and who probably have an increased risk of PPC to begin with.
The number of fractures with Peterson III–V morphologies was too limited to draw reliable statistical conclusions, but it seems that Peterson classification correlates with PPC risk. Arkader et al. found Salter-Harris classification to be a significant predictor for both outcome and complications and findings by Garrett et al. were also in support of this [4,8]. However, several authors have failed to show this association [5-7].
The majority of our patients (42/70) were treated non-surgically. Treatment of unstable, dislocated Peterson II and III fractures is likely the most controversial, as the management without internal fixation is highly prone to re-displacement, whereas internal fixation requires a physeal-crossing technique in Peterson III fractures and those Peterson II fractures with a too small Thurstan–Holland fragment for fixation [17]. 4 of our patients were treated with physeal crossing pins, 3 of whom developed PPC (Table 2). Arkader et al. found a higher incidence rate of complications occurring when the physis was violated by hardware, while some authors argue that usage of smooth pins would be unlikely to cause the PPC [8,17].
The surgical treatment approach displayed statistical significance in risk of PPC compared with non-surgical treatment. However, selection bias is again likely to affect the findings as the surgically treated patients were more likely to sustain high-energy fractures with greater dislocation. Previous studies have displayed essentially unchanged complication rates despite different treatment approaches [4-6,8]. Thus, it seems that the etiological factors such as injury energy and dislocation have more significance in the development of PPC than the treatment strategy itself. It is challenging to evaluate the effect of treatment strategy on the risk of PPC. This is due to insufficient number of patients for multivariate analysis in the current and previous studies, and because fracture energy and dislocation seem to both predict the PPC risk and to guide treatment strategy.
The physis of the distal femur accounts for 70% of the growth of the femur and 37% of the total growth of the lower extremity, making these fractures susceptible to clinically significant growth disturbances, especially if sustained at a young age [18]. Fortunately, only 1 patient with PPC suffered from a clinically significant growth disturbance, as all our patients who sustained PPC were older children (> 11 years) approaching skeletal maturity.
In addition to PPC, other complications that have been reported regarding physeal fractures of the distal femur include stiffness, ligamentous injuries, and, rarely, compartment syndrome and peroneal nerve neuropraxia [4-6,10]. None of our patients suffered from neurovascular complications or compartment syndrome.
We have decided to use the Peterson classification instead of the Salter-Harris at our clinic as it is more comprehensive, considering how frequently Peterson I fractures occur. Although we could not draw statistical conclusions concerning the predicament of PPC according to the Peterson classification, many of our findings supported Peterson’s aim to create a classification that reflected the severity of the physeal injury: Peterson III–IV patients sustained injury in more high-energy settings, had more associated injuries and were more likely to be surgically treated compared with patients with Peterson I and II fractures (Table 1). Moreover, the classification reflects the age of the patients as young children are more prone to sustain injuries in the metaphysis, in contrast to older children who tend to have more intra-articular involvement.
Strengths and limitations
This is a register-based study with limitations. First, a few children might have been treated elsewhere in the Helsinki area, which may affect the incidence. However, physeal fractures of the distal femur are almost invariably treated at our tertiary level university hospital. Even though the primary care would have been done elsewhere, the follow-up visits are also included in our register. Thus, the basis for an approximation of the population-based incidence is solid. Second, the reliability of statistical conclusions that can be made is inherently limited by the small number of patients in our study, even if it represents one of the largest patient series on this fracture type. Third, initial dislocations are prone to error as we can only assess them from primary radiographs. Fourth, assessment of injury energies is based on subjective judgment, and it is challenging to categorize patients reliably in injury energy groups and to compare injury energies between studies. Finally, the children suffering from lower-extremity physeal fractures are evaluated for physeal growth disturbances after 6 months at our clinic.
The strengths of our study include the prospective data collection using the Kids’ Fracture Tool, which has been shown to collect comprehensive data accurately during the entire treatment [14]. We considered the use of relative risk instead of odds ratio (OR) but, taking into consideration that we decided to use the DAG methodology, logistic regression was used. Furthermore, this is a retrospective (case-control) study, where OR was used as a measure of the strength of association between the exposure and outcome. Our outcome is binary, which is easier to interpret in odds-ratio terms: the effect of an explanatory variable is multiplicative on the odds and thus leads to an odds ratio. However, it should be noted that relative risk has been used in similar study designs [19].
Conclusions
Physeal fractures of the distal femur occurred with an estimated annual incidence of 6/105 children, and a resulting PPC occurred in 23% of these fractures with an estimated annual incidence of 1.3/105 children. Etiological factors such as dislocation exceeding 10 mm and higher fracture energy were found to be significant risk factors and seem to have more significance in the development of PPC than the treatment strategy itself.
- Peterson H A, Madhok R, Benson J T, Ilstrup D M, Melton L J 3rd. Physeal fractures, Part 1: Epidemiology in Olmsted County, Minnesota, 1979–1988. J Pediatr Orthop 1994; 14: 423-30. doi: 10.1097/01241398-199407000-00002.
- Kawamoto K, Kim W C, Tsuchida Y, Tsuji Y, Fujioka M, Horii M, et al. Incidence of physeal injuries in Japanese children. J Pediatr Orthop B 2006; 15: 126-30. doi: 10.1097/01.bpb.0000191874.69258.0b.
- Mizuta T, Benson W M, Foster B K, Paterson D C, Morris L L. Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop 1987; 7: 518523. doi: 10.1097/01241398-198709000-00003.
- Arkader A, Warner W C Jr, Horn B D, Shaw R N, Wells L. Predicting the outcome of physeal fractures of the distal femur. J Pediatr Orthop 2007; 27: 703-8. doi: 10.1097/BPO.0b013e3180dca0e5.
- Adams A J, Mahmoud M A H, Wells L, Flynn J M, Arkader A. Physeal fractures of the distal femur: does a lower threshold for surgery lead to better outcomes? J Pediatr Orthop B 2020; 29: 40-6. doi: 10.1097/BPB.0000000000000664.
- Eid A M, Hafez M A. Traumatic injuries of the distal femoral physis: retrospective study on 151 cases. Injury 2002; 33: 251-5. doi: 10.1016/s0020-1383(01)00109-7.
- Bellamy J T, Ward L A, Fletcher N D. Evaluation of pediatric distal femoral physeal fractures and the factors impacting poor outcome requiring further corrective surgery. J Pediatr Orthop B 2021; 30: 6-12. doi: 10.1097/BPB.0000000000000733.
- Garrett B R, Hoffman E B, Carrara H. The effect of percutaneous pin fixation in the treatment of distal femoral physeal fractures. J Bone Joint Surg Br 2011; 93: 689-94. doi: 10.1302/0301-620X.93B5.25422.
- Riseborough E J, Barrett I R, Shapiro F. Growth disturbances following distal femoral physeal fracture-separations. J Bone Joint Surg Am 1983; 65: 885-93. PMID: 6885868.
- Ilharreborde B, Raquillet C, Morel E, Fitoussi F, Bensahel H, Pennecot G F, et al. Long-term prognosis of Salter-Harris type 2 injuries of the distal femoral physis. J Pediatr Orthop B 2006; 15: 433-8. doi: 10.1097/01.bpb.0000228384.01690.aa.
- Thomson J D, Stricker S J, Williams M M. Fractures of the distal femoral epiphyseal plate. J Pediatr Orthop 1995; 15: 474-8. doi: 10.1097/01241398-199507000-00013.
- Lombardo S J, Harvey J P Jr. Fractures of the distal femoral epiphyses: factors influencing prognosis: a review of thirty-four cases. J Bone Joint Surg Am 1977; 59: 742-51. PMID: 908697
- Peterson H A. Physeal fractures, Part 3: Classification. J Pediatr Orthop 1994; 14: 439-48. doi: 10.1097/01241398-199407000-00004.
- Laaksonen T, Kosola J, Nietosvaara N, Puhakka J, Nietosvaara Y, Stenroos A. Epidemiology, treatment, and treatment quality of over-riding distal metaphyseal radial fractures in children and adolescents. J Bone Joint Surg Am 2022; 104: 207-14. doi: 10.2106/JBJS.21.00850.
- City of Helsinki Executive Office, Urban Research and Statistics. Statistical Yearbook of Helsinki 2019. (Accessed 2021 Oct 12.) Available from: https://www.hel.fi/hel2/tietokeskus/julkaisut/pdf/20_03_10_Vuosikirjaenglanti2019.pdf [Context Link].2014-2021.
- Shrier I, Platt R W. Reducing bias through directed acyclic graphs. BMC Med Res Methodol 2008; 8: 70. doi: 10.1186/1471-2288-8-70.
- Rockwood C A, Beaty J H, Kasser J R. Rockwood and Wilkins’ fractures in children. 7th ed. Philadelphia: Wolters Kluwer/Lippincott, Williams & Wilkins; 2010.
- Pritchett J W. Longitudinal growth and growth-plate activity in the lower extremity. Clin Orthop Relat Res 1992; (275): 274-9. PMID: 1735225.
- Frost M W, Rahbek O, Iobst C, Bafor A, Duncan M, Kold S. Complications and risk factors of intramedullary bone lengthening nails: a retrospective multicenter cohort study of 314 FITBONE and PRECICE nails. Acta Orthop 2023; 94: 51-9. doi: 10.2340/17453674.2023.8479.
Appendix
| Case | Sex | Age | Peterson fracture class | Mechanism of injury | Dislocation (mm) | Thurstan–Holland fragment (% of physeal width) | Treatment method | Procedure due to PPC | Growth disturbance a | |
| AP | Sag. | |||||||||
| 1 | Girl | 12.5 | II | Fall on same level | 23 | 3 | 10 mm (11) | Physeal crossing pins | Physiodesis distal femur, contralateral | Insignificant |
| 2 | Boy | 14.2 | II | Moped | 2 | 2 | 26 mm (29) | Cast | Physiodesis distal femur, contralateral | Insignificant |
| 3 | Girl | 11.7 | II | Trampoline | 17 | 57 | 8 mm (10) | Physeal crossing pins | Physiodesis distal femur, bilateral | LLD 7 mm |
| 4 | Boy | 14.7 | V | Soccer | 91 | 29 | Physeal crossing pins | Physiodesis distal femur, contralateral | LLD 7 mm | |
| 5 | Boy | 15.2 | V | Motor sled | 15 | 22 | Physeal crossing pins | Physiodesis distal femur, contralateral | LLD 10 mm | |
| 6 | Boy | 12.6 | II | Downhill skiing | 44 | 38 | 55 mm (62) | Screws | Physiodesolysis distal femur, ipsilateral | LLD 10 mm Valgus 5° |
| 7 | Boy | 13.9 | II | Soccer | 1 | 0 | 12 mm (13) | Cast | Physiodesis distal femur, contralateral | LLD 20 mm |
| 8 | Boy | 13.8 | V | Fall | 44 | 2 | K-wires | Limb lengthening | LLD 38 mm | |
| 9 | Girl | 12.5 | II | Bike | 3 | 0 | 34 mm (39) | Screws | Insignificant | |
| 10 | Boy | 15.2 | II | Ice hockey | 37 | 29 | 44 mm (52) | Screws | Insignificant | |
| 11 | Boy | 14.7 | II | Ice hockey | 29 | 5 | 42 mm (50) | Screws | Insignificant | |
| 12 | Boy | 15.3 | II | Moped | 20 | 2 | 40 mm (44) | Physeal crossing pins | Insignificant | |
| 13 | Boy | 15.2 | III | Moped | 22 | 30 | Physeal crossing pins | Insignificant | ||
| 14 | Boy | 15.4 | III | Run over | 13 | 3 | Physeal crossing pins | Insignificant | ||
| 15 | Boy | 14.8 | III | Motocross | 0 | 6 | Physeal crossing pins | LLD 10 mm | ||
| 16 | Girl | 12.4 | V | Car collision | 4 | 2 | Physeal crossing pins | LLD 20 mm | ||
| a The LLD (leg length discrepancy.) and angular measurements represent the discrepancy before any additional surgical procedures. | ||||||||||