A comparison of uncemented short versus standard stem length in total hip arthroplasty: results from the Dutch Arthroplasty Register
Mirthe H W VAN VEGHEL 1, Gerjon HANNINK 2, Jakob VAN OLDENRIJK 3, Liza N VAN STEENBERGEN 4, and B Willem SCHREURS 1,4
1 Department of Orthopedics, Radboud University Medical Center, Nijmegen; 2 Department of Medical Imaging, Radboud University Medical Center, Nijmegen; 3 Erasmus University Medical Center, Department of Orthopedics and Sport Medicine, Rotterdam; 4 Dutch Arthroplasty Register (Landelijke Registratie Orthopedische Interventies), ‘s-Hertogenbosch, the Netherlands
Background and purpose — We aimed to compare revision rates between uncemented short and standard stems in total hip arthroplasties (THAs) and the corresponding patient-reported outcome measures (PROMs).
Patients and methods — We included all short (C.F.P., Fitmore, GTS, Metha, Nanos, Optimys, Pulchra, and Taperloc Microplasty) and standard stems in uncemented THAs registered between 2009 and 2021 in the Dutch Arthroplasty Register. Kaplan–Meier survival and multivariable Cox regression analyses were performed with overall and femoral stem revision as endpoints.
Results — Short stems were used in 3,352 and standard stems in 228,917 hips. 10-year overall revision rates (4.8%, 95% confidence interval [CI] 3.7–6.3 vs. 4.5%, CI 4.4–4.6) and femoral stem revision rates (3.0%, CI 2.2–4.2 vs. 2.3%, CI 2.2–2.4) were comparable for short- and standard-stem THAs. Today’s predominant short stems (Fitmore and Optimys) showed short-term revision rates similar to that of standard-stem THAs. Other, less frequently used short stems had higher 10-year overall (6.3%, CI 4.7–8.5) and femoral stem (4.5%, CI 3.1–6.3) revision rates. Multivariable Cox regression also showed a higher risk for overall (HR 1.7, CI 1.0–2.9) and femoral stem revision (HR 2.0, CI 1.1–3.5) using the latter short stems compared with standard stems. An exploratory analysis of PROMs showed no difference.
Conclusion — There was no overall difference in revision rates but a tendency toward increased revision of short stems both for the whole THA and for the stem itself. The less frequently used short stems had increased revision risk. No difference in PROMs was shown.
Citation: Acta Orthopaedica 2023; 94: 330–335. DOI: https://doi.org/10.2340/17453674.2023.13652.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-14. Accepted: 2023-05-23. Published: 2023-07-07.
Correspondence: Mirthe.vanVeghel@radboudumc.nl
GH, JvO, LNvS, BWS: concept and design. MHWvV, GH: data analysis and interpretation. MHWvV: manuscript preparation. MHWvV, GH, LNvS, BWS: manuscript editing. MHWvV, GH, JvO, LNvS, BWS: manuscript review. MHWvV, GH, JvO, LNvS, BWS: final approval of the version submitted.
Handling co-editors: Keijo Mäkelä and Philippe Wagner
Acta thanks Christian Delaunay and John Tucker for help with peer review of this manuscript.
In recent decades, there has been an increase in total hip arthroplasties (THAs), particularly in young patients [1,2]. Bone-saving implants such as short femoral components may be important in these patients to facilitate future revisions, although little evidence for this exists [3].
Uncemented short-stem THAs have become more prevalent in recent years in some countries [4]. Although a clear definition is lacking, these short stems are characterized as small cementless femoral components that preserve more femoral neck and achieve metaphyseal fixation [5,6]. 3 main advantages of short stems may be preservation of proximal bone stock for future revisions, improvement of biomechanical reconstruction, and the possibility for less invasive approaches [4,7-9].
Short stems have shown revision rates and improvements in functional outcome similar to standard stems at short- and mid-term follow-up [4,8,10]. However, only limited population-based registry studies on short-stem THAs are available [8,10,11]. Due to their increased popularity, particularly in younger and fitter patient groups, more population-based registry studies on incidence of short-stem THAs, revision rates, and patient-reported outcome measures (PROMs) are needed to show the average results in contrast to randomized controlled trials.
Also, the bone-preserving features of short stems during future revisions have yet to be confirmed. Bone preservation may allow for the use of standard-length stems during component exchange, rather than larger revision stems to compensate for proximal bone loss. It may be valuable to know more about the types of femoral implants used during revision of these short stems.
Therefore, we aimed to compare patients, procedure and prosthesis characteristics, revision rates, patient-reported quality of life, pain, and physical functioning in patients with primary uncemented short-stem THAs and standard-stem THAs, using data from the Dutch Arthroplasty Register (LROI).
Patients and methods
Data was obtained from the LROI. The LROI is a national population-based arthroplasty register, established by the Netherlands Orthopaedic Association (NOV) in 2007. In 2012, 100% coverage of Dutch hospitals was achieved with a completeness of more than 95% of primary THAs [12]. Nowadays, 99% completeness of primary THAs and 98% of revision arthroplasties have been reached [13]. The LROI contains data on patient, prosthesis, and procedure characteristics of primary and revision arthroplasties and PROMs. Prosthesis characteristics are obtained from an implant library, which is based on article numbers of prosthesis components, and consists among others of data on type, brand, name, and material of the prosthesis component provided by the manufacturer. Revision arthroplasty is defined as a replacement, removal or addition of 1 or more components of the implant [12]. PROMs registered in the LROI are the EuroQol 5 Dimensions index score (EQ-5D), the EuroQol Visual Analog Scale (EQ VAS), the Hip disability and Osteoarthritis Outcome Score – Physical function Short form (HOOS-PS), the Oxford Hip Score (OHS), and the Numeric Rating Scale during activity (NRS activity) and at rest (NRS rest). PROMs are measured preoperative and at 3 months and 12 months postoperatively.
We included all primary THAs with an uncemented short or standard femoral component in the period 2009–2021 (Figure 1). THAs with a metal-on-metal articulation (n = 3,619) and procedures with the diagnosis tumor (n = 20) were excluded. Short-stem THAs were defined based on the definition of the LROI and previous literature [4-6,8,14-16]. The LROI defines a short stem as a small cementless femoral component with special design features where fixation is intended to be metaphyseal [17]. Short stems identified in the LROI were C.F.P. (Waldemar Link, Hamburg, Germany), Fitmore (Zimmer Biomet, Warsaw, IN, USA), GTS (Zimmer Biomet, Warsaw, IN, USA), Metha (B. Braun Aesculap, Tuttlingen, Germany), Nanos (Smith & Nephew, London, UK), Optimys (Mathys, Bettlach, Switzerland), Pulchra (Adler Orthro, Cormano, Italy) and Taperloc Microplasty (Zimmer Biomet, Warsaw, IN, USA) (Figure 1).
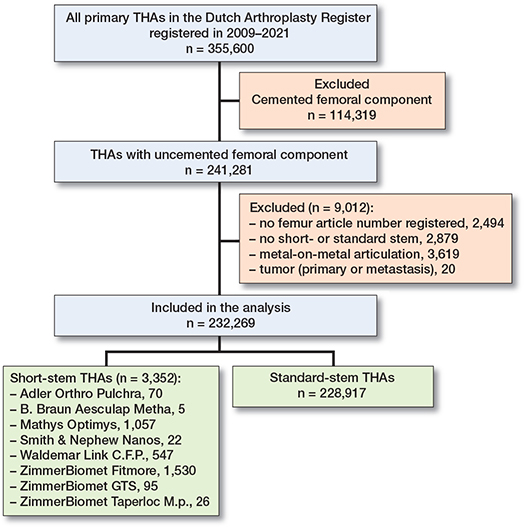
Figure 1. Flowchart of included hips.
Statistics
Descriptive statistics were used to present patients, prosthesis, and procedure characteristics as well as the incidence of short-stem THAs by type of hospital (i.e., general hospital, private clinic, or academic medical center). Crude Kaplan–Meier survival analyses were performed to determine 10-year overall and femoral stem revision rates including 95% confidence intervals (CI) according to type of stem. Survival was defined as the time between primary THA to first revision, death of the patient, or end of follow-up (January 1, 2022). Multivariable Cox regression analyses were used to account for differences in confounders between the short-stem and standard-stem groups. We used log–log plots and testing of scaled Schoenfeld residuals to assess the proportional hazards assumption, which appeared to be violated. Therefore, Schemper’s weighted Cox models were used [18]. Age, sex, American Society of Anesthesiologists (ASA) score, diagnosis (osteoarthritis [OA] vs. non-OA), and surgical approach were considered confounders. Body mass index (BMI) and smoking status were not included as confounders, as these variables have been registered in the LROI since 2014. Missing data in confounders was imputed, using multiple imputation by chained equations using predictive mean matching in which 15 datasets were created. Less than 1% was missing for each confounder. There was no missing data in outcome variables. Effect estimates were pooled according to Rubin’s Rules. For CIs, we assumed that the number of observed cases followed a Poisson distribution. Reasons for overall and femoral stem revision were described according to stem type. Linear mixed models were performed to analyze PROM scores. Time (i.e., preoperative, 3 months, and 12 months postoperatively) and group (i.e., short stem vs. standard stem) were included as fixed factors, and patient as a random factor. Possible interaction between time and group was included as fixed factor if model fit improved. Residual plots as well as Q–Q plots were used to visually examine the distributions of both random effects and residuals, which were approximately normally distributed. PROM analyses were performed on patients with a short-stem or standard-stem THA for primary OA since 2014, as PROM scores are available for these patients since 2014 in the LROI. PROM data were not imputed, as a complete PROM score (preoperative as well as 3-month and 12-month postoperative response) was available in less than 30%. Only patients with complete PROM scores were included in the PROM analyses. Therefore, the PROM analyses should be considered an exploratory analysis.
Incidence analyses, Kaplan–Meier survival analyses, and multivariable Schemper’s weighted Cox regression analyses were also performed separately for short-stem THAs with Fitmore, and Optimys versus other short stems, as Fitmore and Optimys are currently widely used in the Netherlands, while the other short stems have mainly been used in the past.
This study was reported in accordance with the STROBE guidelines. R (version 4.0.4, R Foundation for Statistical Computing, Vienna, Austria) was used to perform all analyses.
Ethics, data sharing, funding, and disclosures
Data was received completely anonymously. Data was available from the LROI, but restrictions apply to the availability of this data, which was used under license for the current study. This study is funded by the Dutch Arthroplasty Register. No conflicts of interest were declared. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.13652
Results
232,269 THAs were included in the period 2009–2021, of which 3,352 (1.4%) were short-stem THAs. Fitmore (n = 1,530) and Optimys (n = 1,057) were the 2 most implanted short stems (Figure 1). Median follow-up was 5.1 (interquartile range [IQR] 2.5–8.1) years. Short-stem THA patients were younger (63, SD 10 vs. 67, SD 10 years) and had a lower ASA score (ASA-I 36% vs. 22%) than standard-stem THA patients. More short-stem THA patients were of normal weight than standard-stem THA patients (36% vs. 23%). The anterior approach was most often used in short-stem THAs (67%), while the posterolateral approach was commonly used in standard-stem THAs (53%). In both groups, a ceramic-on-polyethylene articulation and a 32 mm femoral head were most frequently used. Short-stem THAs were more often performed in a private clinic than standard-stem THAs (59% vs. 9.0%) (Table 1).
| Factor | Standard stem n = 228,917 | Short stem n = 3,352 |
| Age, mean (SD) | 67 (10) | 63 (10) |
| Missing | 169 (0.1) | 1 (0.0) |
| Male sex | 85,633 (37) | 1,323 (40) |
| Missing | 300 (0.1) | 1 (0.0) |
| Diagnosis | ||
| Osteoarthritis | 202,126 (88) | 3,059 (91) |
| Dysplasia | 4,785 (2.1) | 117 (3.5) |
| Fracture | 7,654 (3.3) | 1 (0.0) |
| Other | 13,339 (5.8) | 163 (4.9) |
| Missing | 1,013 (0.4) | 12 (0.4) |
| ASA score | ||
| I | 51,070 (22) | 1,198 (36) |
| II | 143,788 (63) | 2,000 (60) |
| III–IV | 32,516 (14) | 125 (3.7) |
| Missing | 1,543 (0.7) | 29 (0.9) |
| Charnley classification a | ||
| A | 72,261 (32) | 1,342 (40) |
| B1 | 47,381 (21) | 858 (26) |
| B2 | 33,962 (15) | 539 (16) |
| C | 3,844 (1.7) | 59 (1.8) |
| Missing | 71,469 (31) | 554 (17) |
| Smoking a | 18,365 (8.0) | 243 (7.2) |
| Missing | 72,065 (32) | 550 (16) |
| Body mass index a | ||
| Underweight (≤ 18.5) | 1,171 (0.5) | 11 (0.3) |
| Normal weight (>18.5–25) | 53,265 (23) | 1,195 (36) |
| Overweight (>25–30) | 68,739 (30) | 1,141 (34) |
| Obesity (>30–40) | 37,379 (16) | 449 (13) |
| Morbid obesity (>40) | 1,849 (0.8) | 5 (0.1) |
| Missing | 66,514 (29) | 551 (16) |
| Previous surgery at affected hip | 9,157 (4.0) | 139 (4.1) |
| Missing | 6,008 (2.6) | 31 (0.9) |
| Fixation | ||
| Cementless | 215,573 (94) | 3,252 (97) |
| Acetabulum cemented | 13,158 (5.7) | 99 (3.0) |
| Missing | 186 (0.1) | 1 (0.0) |
| Surgical approach | ||
| Anterior | 58,654 (26) | 2,249 (67) |
| Anterolateral | 12,795 (5.6) | 89 (2.7) |
| Posterolateral | 121,353 (53) | 368 (11) |
| Straight lateral | 33,350 (15) | 601 (18) |
| Other | 2,040 (0.9) | 38 (1.1) |
| Missing | 725 (0.3) | 7 (0.2) |
| Articulation | ||
| Ceramic-on-ceramic | 20,081 (8.8) | 145 (4.3) |
| Ceramic-on-metal | 66 (0.0) | 0 (0.0) |
| Ceramic-on-polyethylene | 137,586 (60) | 2,878 (86) |
| Metal-on-ceramic | 5 (0.0) | 0 (0.0) |
| Metal-on-polyethylene | 44,699 (20) | 193 (5.8) |
| Oxidized zirconium-on-polyethylene | 18,707 (8.2) | 19 (0.6) |
| Missing | 7,773 (3.4) | 117 (3.5) |
| Femoral head size | ||
| 22–28 mm | 38,854 (17) | 231 (6.9) |
| 32 mm | 126,521 (55) | 2,388 (71) |
| 36 mm | 60,242 (26) | 662 (20) |
| ≥ 38 mm | 1,253 (0.5) | 13 (0.4) |
| Missing | 2,047 (0.9) | 58 (1.7) |
| Type of hospital | ||
| General hospital | 204,420 (89) | 1,322 (39) |
| Private clinic | 20,664 (9.0) | 1,982 (59) |
| Academic medical center | 3,832 (1.7) | 48 (1.4) |
| Missing | 1 (0.1) | 0 (0.0) |
| a Registered since 2014. | ||
In general hospitals, the annual number of short-stem THAs varied between 40 and 180 in the period 2009–2021, whereas in private clinics it increased from 1 in 2015 to 1,124 in 2021. In both general hospitals and private clinics, the Fitmore and Optimys stem were used most often in recent years, while the use of the other short stems decreased in this period. In academic medical centers, the annual number of short-stem THAs ranged between 0 and 10 in the period 2009–2021.
Revision
Crude 10-year overall and femoral stem revision rates were comparable for short-stem and standard-stem THAs (Figure 2). The crude 10-year overall revision rate was 4.8% (CI 3.7–6.3) for short-stem THAs and 4.5% (CI 4.4–4.6) for standard-stem THAs. The crude 10-year femoral stem revision rate was 3.0% (CI 2.2–4.2) for short-stem THAs and 2.3% (CI 2.2–2.4) for standard-stem THAs. Short-stem THAs with a Fitmore or Optimys stem showed comparable short-term overall and femoral stem revision rates to standard-stem THAs. THAs with other short stems had higher 10-year overall (6.3%, CI 4.7–8.5) and femoral stem (4.5%, CI 3.1–6.3) revision rates than standard-stem THAs.
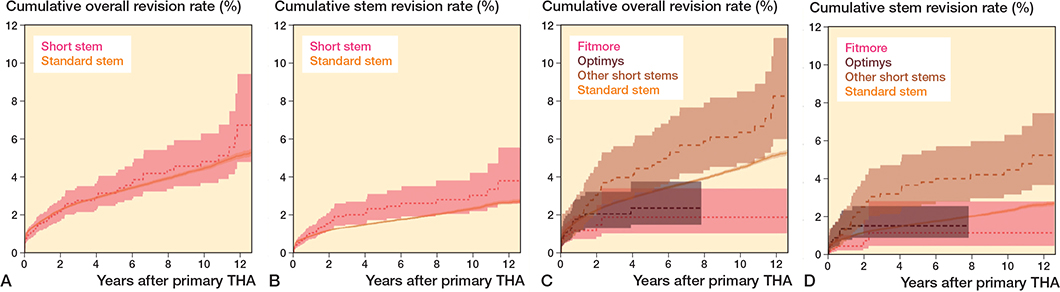
Figure 2. Cumulative overall (A) and femoral stem (B) revision rates of primary THAs according to type of stem and according to type of short stem (C and D respectively).
Multivariable Schemper’s weighted Cox regression analyses adjusted for age, sex, ASA score, diagnosis, and surgical approach showed a comparable risk of overall revision (HR 1.4, CI 0.9–2.1), but a higher risk of femoral stem revision (HR 1.5, CI 1.0–2.4) for short-stem THAs compared with standard-stem THAs (Table 2). No statistically significant differences in risk of overall and femoral stem revision were found between THAs with a Fitmore, Optimys, or standard stem, adjusted for age, sex, ASA score, diagnosis, and surgical approach. The other short-stem group was associated with a higher adjusted risk for overall (HR 1.7, CI 1.0–2.9) and femoral stem (HR 2.0, CI 1.1–3.5) revision compared with the standard stem.
| Type of stem | Overall revision | Femoral stem revision | ||
| Crude HR (CI) | Adjusted a HR (CI) | Crude HR (CI) | Adjusted a HR (CI) | |
| Standard stems | 1.0 (ref.) | 1.0 (ref.) | 1.0 (ref.) | 1.0 (ref.) |
| All short stems | 1.3 (0.9–2.0) | 1.4 (0.9–2.1) | 1.4 (0.9–2.2) | 1.5 (1.0–2.4) |
| Fitmore | 0.6 (0.4–1.0) | 0.9 (0.5–1.4) | 0.6 (0.3–1.1) | 0.7 (0.4–1.5) |
| Optimys | 0.8 (0.5–1.2) | 0.9 (0.6–1.4) | 1.0 (0.6–1.8) | 1.1 (0.7–1.9) |
| Other short stems | 1.8 (1.0–3.0) | 1.7 (1.0–2.9) | 1.9 (1.1–3.4) | 2.0 (1.1–3.5) |
| a Adjusted for age, sex, ASA score, diagnosis, and surgical approach. | ||||
Reasons for revision
The most common reason for overall and femoral stem revision of short-stem THAs was aseptic femoral loosening (27% and 42% respectively), followed by infection (25% and 20% respectively) (Table 3). In short-stem THAs, dislocation was less frequently registered as reason for overall revision compared with standard-stem THAs (8.2% vs. 22%). Femoral stem revisions due to periprosthetic fractures were less prevalent in short-stem THAs compared with standard-stem THAs (13% vs. 24%).
PROMs
There were 142,314 THAs for primary OA since 2014, of which 2,589 (1.8%) had a short stem. Depending on the type of PROM, 8–11% of short-stem THA patients and 22–24% of standard-stem THA patients completed the preoperative as well as the 3-months and 12-months postoperative PROMs. All PROM scores improved at 3 months and 12 months postoperatively in both the short-stem and standard-stem groups (Figure 3). No clinically relevant differences were found between short-stem and standard-stem patients in EQ-5D (0.0, CI 0.0–0.0), EQ VAS (0.8, CI –0.8 to 2.4), HOOS-PS (0.8, CI –0.5 to 2.2), OHS (0.0, CI –0.8 to 0.7), NRS during activity (0.2, CI 0.0–0.4), and NRS at rest (0.1, CI 0.0–0.3) scores.
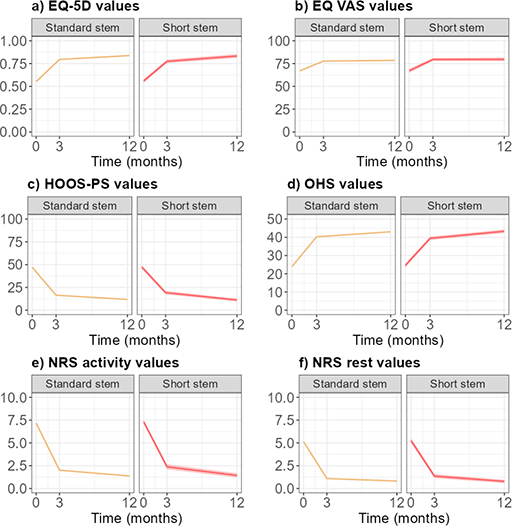
Figure 3. (a) EQ-5D (n = 33,642), (b) EQ VAS (n = 34,214), (c) HOOS-PS (n = 30,485), (d) OHS (n = 30,654), (e) NRS during activity (n = 34,453), and (f) NRS at rest (n = 34,460) mean scores with 95%CI of primary THAs for OA since 2014 according to type of stem.
Discussion
We aimed to compare patients, procedure and prosthesis characteristics, revision rates, patient-reported quality of life, pain, and physical functioning in patients with primary uncemented short versus standard stems in THA. We showed no difference in overall or femoral stem revision rates of THAs with a Fitmore, Optimys, or standard stem, whereas less frequent short stems had higher revision rates. However, it is uncertain whether Fitmore, Optimys, and standard stems have comparable short-term overall and femoral stem revision rates in the general patient population as the number of short stems was small and thus the confidence intervals were wide in our study.
Comparing our study with other registry studies on short-stem THAs is complex, as each study included different short stems. A recent study from Steinbrück et al. [19] demonstrated similar 5-year overall revision rates between matched cohorts of short-stem THAs (2.9%, CI 2.4–3.5, including Optimys, Metha, A2-Kurzschaft, and Nanos) and standard-stem THAs (3.1%, CI 2.7–3.4), using data from the German Arthroplasty Registry (EPRD [Endoprothesenregister Deutschland]). The 5-year overall revision rate for THAs with an Optimys stem was 1.8% (CI 1.5–2.2), which is comparable to our results. The Registry of Prosthetic Orthopedic Implants (RIPO, Italy) found somewhat higher 10-year overall revision rates of 6.1–6.6% for both short-stem THAs (including C.F.P., Nanos, Parva, Fitmore, MiniMax, and Amistem-H) and standard-stem THAs [11]. No prosthesis-specific results for short stems were described. None of these registries have reported results on femoral stem revision or PROMs of short-stem THAs.
The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) reported a 10-year overall revision rate of 2.9% (CI 2.4–3.6) for short-stem THAs in their annual report [20]. This revision rate is lower than for standard-stem THAs performed in Australia (4.4%, CI 4.3–4.5) and our 10-year overall revision rate of short-stem THAs. However, the AOANJRR restricted its analyses to prostheses currently in use, including Collo-Mis, Metha, MiniHip, MiniMax, Nanos, Optimys, and Taperloc Microplasty, whereas we included all commercially available short stems. THAs with an Optimys stem had a 5-year overall revision rate of 1.6% (CI 0.8–3.2), which is in line with our results.
In our study, patients with short stems may have a higher risk for femoral stem revision compared with standard-stem THA patients. However, this higher risk can be explained by short stems that are hardly used in the Netherlands anymore, including Pulchra, Metha, Nanos, C.F.P., GTS, and Taperloc Microplasty. Our study showed a comparable risk for femoral stem revision for Fitmore, Optimys, and standard stems.
Dislocation is less frequently reported as the reason for overall revision of short-stem THAs compared with standard-stem THAs in our study. This may be explained by the more frequent use of the anterior approach in short-stem THAs [21]. In short-stem THAs, periprosthetic fractures are less frequently registered as reason for femoral stem revision than in standard-stem THAs. Advanced age is associated with an increased risk of periprosthetic fractures [22]. In our study, short-stem THA patients were younger than standard-stem THA patients, which may explain the smaller proportion of femoral stem revisions due to periprosthetic fractures in the short-stem THA group. An alternative explanation is that these short stems have their fixation mainly in the metaphyseal area and hence generate less stress in the diaphyseal area.
No differences are found in patient-reported quality of life, pain, and physical functioning between short-stem and standard-stem THA patients. However, PROM response was low in both groups. Hutchings et al. [23] found a pattern of lower postoperative PROM response in patients with worse preoperative EQ-5D and OHS scores. Consequently, PROM scores could be overestimated in this study. In addition, floor and ceiling effects as well as regression to the mean may have played a role in the PROM scores. The proportion of PROMs of patients with a Fitmore stem was relatively low in this study. More than half of the Fitmore stems were implanted in 2021. Therefore, 12 months of follow-up is not yet available for these stems. As a result, there were relatively fewer PROM scores from private clinics. There were no differences in age and sex between PROM responders and non-responders.
This study has some limitations. Confounding may occur by indication as short-stem THA patients are younger and may have better health. Short stems may have been used in few hospitals or by few surgeons, resulting in less generalizable results. Multivariable Cox regression analyses were restricted to patient and procedure characteristics recorded in the LROI. Therefore, possible confounders such as physical activity could not be included. Furthermore, BMI and smoking status could not be included as covariates, as these variables have been registered only since 2014 in the LROI. However, sensitivity analyses with data from the period 2014–2021 showed our results to be robust. Lastly, in the absence of a clear definition of short stem, we based our definition on that of the LROI and previous literature. However, other national arthroplasty registers such as the AOANJRR and the EPRD use a similar definition of a short stem [20,24].
In conclusion, there was no overall difference in revision rates but a tendency toward increased revision of short stems both for the whole THA and for the stem itself. The less frequently used short stems had increased revision risk. No difference in PROMs was shown. As the follow-up of patients with short stems is still limited in the Netherlands, it is recommended to continue following these patients.
- Mei X Y, Gong Y J, Safir O, Gross A, Kuzyk P. Long-term outcomes of total hip arthroplasty in patients younger than 55 years: a systematic review of the contemporary literature. Can J Surg 2019; 62: 249-58. doi: 10.1503/cjs.013118.
- Pivec R, Johnson A J, Mears S C, Mont M A. Hip arthroplasty. Lancet 2012; 380: 1768-77. doi: 10.1016/S0140-6736(12)60607-2.
- Bayliss L E, Culliford D, Monk A P, Glyn-Jones S, Prieto-Alhambra D, Judge A, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet 2017; 389: 1424-30. doi: 10.1016/S0140-6736(17)30059-4.
- Lidder S, Epstein D J, Scott G. A systematic review of short metaphyseal loading cementless stems in hip arthroplasty. Bone Joint J 2019; 101-B: 502-11. doi: 10.1302/0301-620X.101B5.BJJ-2018-1199.R1.
- Falez F, Casella F, Papalia M. Current concepts, classification, and results in short stem hip arthroplasty. Orthopedics 2015; 38: S6-13. doi: 10.3928/01477447-20150215-50.
- Khanuja H S, Banerjee S, Jain D, Pivec R, Mont M A. Short bone-conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am 2014; 96: 1742-52. doi: 10.2106/JBJS.M.00780.
- Gustke K. Short stems for total hip arthroplasty: initial experience with the Fitmore stem. J Bone Joint Surg Br 2012; 94: 47-51. doi: 10.1302/0301-620X.94B11.30677.
- van Oldenrijk J, Molleman J, Klaver M, Poolman R W, Haverkamp D. Revision rate after short-stem total hip arthroplasty: a systematic review of 49 studies. Acta Orthop 2014; 85: 250-8. doi: 10.3109/17453674.2014.908343.
- Patel R M, Stulberg S D. The rationale for short uncemented stems in total hip arthroplasty. Orthop Clin North Am 2014; 45: 19-31. doi: 10.1016/j.ocl.2013.08.007.
- Hauer G, Vielgut I, Amerstorfer F, Maurer-Ertl W, Leithner A, Sadoghi P. Survival rate of short-stem hip prostheses: a comparative analysis of clinical studies and national arthroplasty registers. J Arthroplasty 2018; 33: 1800-5. doi: 10.1016/j.arth.2018.01.017.
- Giardina F, Castagnini F, Stea S, Bordini B, Montalti M, Toni A. Short stems versus conventional stems in cementless total hip arthroplasty: a long-term registry study. J Arthroplasty 2018; 33: 1794-9. doi: 10.1016/j.arth.2018.01.005.
- van Steenbergen L N, Denissen G A, Spooren A, van Rooden S M, van Oosterhout F J, Morrenhof J W, et al. More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86: 498-505. doi: 10.3109/17453674.2015.1028307.
- LROI. Annual report 2022. Landelijke Registratie Orthopedische Interventies; 2022. Available from: https://www.lroi-report.nl/.
- Feyen H, Shimmin A J. Is the length of the femoral component important in primary total hip replacement? Bone Joint J 2014; 96-B: 442-8. doi: 10.1302/0301-620X.96B4.33036.
- Pardo F, Bordini B, Castagnini F, Giardina F, Faldini C, Traina F. Are powder-technology-built stems safe? A midterm follow-up registry study. J Mater Sci Mater Med 2021; 32: 10. doi: 10.1007/s10856-020-06481-8.
- Erivan R, Villatte G, Dartus J, Mertl P, Piriou P, Tracol P, et al. French Hip & Knee Society classification of short-stem hip prostheses: inter- and intra-observer reproducibility. Orthop Traumatol Surg Res 2022; 108: 103126. doi: 10.1016/j.otsr.2021.103126.
- LROI. LROI Implant Library — Hip. Landelijke Registratie Orthopedische Interventies; 2022. Available from: https://golive3.gopublic.nl/media/www.lroi.nl/2022/04/625522c726f17.lroi-implant-library-hip.pdf.
- Schemper M, Wakounig S, Heinze G. The estimation of average hazard ratios by weighted Cox regression. Stat Med 2009; 28: 2473-89. doi: 10.1002/sim.3623.
- Steinbrück A, Grimberg A W, Elliott J, Melsheimer O, Jansson V. Short versus conventional stem in cementless total hip arthroplasty: an evidence-based approach with registry data of mid-term survival. Orthopade 2021; 50: 296-305. doi: 10.1007/s00132-021-04083-y.
- AOANJRR. Hip, knee & shoulder arthroplasty: 2021 annual report. Australian Orthopaedic Association National Joint Replacement Registry; 2021. Available from: https://aoanjrr.sahmri.com/annual-reports-2021.
- Zijlstra W P, De Hartog B, Van Steenbergen L N, Scheurs B W, Nelissen R. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop 2017; 88: 395-401. doi: 10.1080/17453674.2017.1317515.
- Zhu Y, Zhang F, Chen W, Liu S, Zhang Q, Zhang Y. Risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. J Hosp Infect 2015; 89: 82-9. doi: 10.1016/j.jhin.2014.10.008.
- Hutchings A, Neuburger J, Grosse Frie K, Black N, van der Meulen J. Factors associated with non-response in routine use of patient reported outcome measures after elective surgery in England. Health Qual Life Outcomes 2012; 10: 34. doi: 10.1186/1477-7525-10-34.
- EPRD. Annual Report 2021. The German Arthroplasty Registry (EPRD); 2021. Available from: https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/AnnualReport2021-Web_2022-05-19_F.pdf.