6 compared with 12 weeks treatment in the von Rosen splint is sufficient for Barlow and Ortolani positive hips: a comparative study of 237 neonates
Adam SAND, Carl Johan TIDERIUS, Henrik DÜPPE, and Daniel WENGER
Department of Orthopaedics, Lund University, Skåne University Hospital, Sweden
Background and purpose — At our institution, newborns with Barlow or Ortolani positive hips have been treated for 12 weeks with the von Rosen abduction splint until 2012 when the treatment length was halved. We investigate whether acetabular development at 12 months of age and complications differ between hips treated with the von Rosen splint for 6 compared with 12 weeks.
Patients and methods — 99 patients were included in the 6-week program and 138 patients in the 12-week program. We measured the acetabular index (AI) on standard anteroposterior pelvic radiographs taken at 12 months of age. Medical records were reviewed for complications and additional treatments until age 12 months. We used non-inferiority testing with an equivalence margin of 1° with a 95% confidence interval (CI) to compare the 2 groups.
Results — The mean AI at 12 months in the 6-week group was 25° (CI 24–26) compared with 25° (CI 25–26) in the 12-week group. Non-inferiority was demonstrated for the 6-week program: –0.2° (CI –1.1 to 0.7). In the 6-week group, 8 patients received additional treatment, including 1 hip dislocation that occurred between 6 weeks and 3 months. There were no additional treatments or complications in the 12-week group.
Conclusion — AI was equal at 12 months of age for patients treated for 6 compared with 12 weeks in the von Rosen splint. The hip dislocation which occurred indicates that follow-up around 3 months of age is indicated.
Citation: Acta Orthopaedica 2023; 94: 295–299. DOI: https://doi.org/10.2340/17453674.2023.13649.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-01-26. Accepted: 2023-05-13. Published: 2023-06-19.
Correspondence: adam.sand@med.lu.se
All authors contributed to analysis and interpretation of the data.
Handling co-editor: Ilkka Helenius
Acta thanks Nanni Allington and Darko Anticevic for help with peer review of this manuscript.
Early diagnosis and initiation of treatment are the most important factors to avoid a troublesome outcome for patients with developmental dysplasia of the hip (DDH). Abduction splinting is regarded as the optimal treatment of unstable hips in infants, but there is no consensus regarding the choice of abduction splint or treatment length. Several different types of splints and criteria for initiation of treatment have been described.
At our institution, screening for DDH in newborns was initiated in 1952, and a treatment program with the von Rosen abduction splint started in 1956 [1,2]. Treatment length has varied over the years. Previously, infants with Barlow positive (dislocatable) or Ortolani positive (dislocated) hips [3,4] were treated for 12 weeks, and infants with unstable hips (as judged by dynamic sonography during a Barlow test) were treated for 6 weeks.
Since 2012, all infants with neonatal hip instability have been treated for 6 weeks, no matter the degree of instability or dislocation. This change in treatment protocol was supported by a retrospective study of 247 newborns stating that 6 weeks of treatment with the von Rosen splint is sufficient to treat DDH [5]. As 6 of those 247 patients needed additional treatment, including 2 percutaneous tenotomies, and because there was no control group or quantification of radiographic hip development, a comparison of the 2 treatment protocols is indicated.
We aimed to compare the 2 treatment lengths with regards to radiographic outcome at 12 months, and the rates of additional treatments and complications. Our hypothesis was that 6 weeks treatment would yield similar outcome as 12 weeks treatment.
Patients and methods
Study setting
The study group included patients who were born at the 2 maternity units, Malmö and Lund, which are part of Skåne University Hospital, and diagnosed with neonatal hip instability. Patients treated for 12 weeks were treated in Malmö between January 2003 and December 2010, and patients treated for 6 weeks were treated in Lund between September 2013 and December 2019. The study is reported according to STROBE guidelines.
Screening and inclusion
The primary screening for hip instability in newborns in Sweden is done by pediatricians who perform clinical examinations before the children leave the maternity ward. This practice is stipulated by the Swedish National Board of Health and Welfare. The screening program is universal, i.e., clinical examinations are performed on all newborns, regardless of whether risk factors for DDH have been identified or not.
Included in the study were patients who had Barlow positive or Ortolani positive hips where treatment with the splint was initiated within 2 weeks postpartum based on the indication by the orthopedic surgeon. Standard pelvic anteroposterior (AP) radiographs and clinical examinations were performed at 3 months and at 12 months. Medical records were examined for complications and additional treatments occurring before 12 months of age. Patients with a diagnosed syndrome were excluded from the study.
Treatment and group allocation
The findings of the pediatricians were graded into 5 groups: normal, suspected instability, unstable (not dislocatable), dislocatable (Barlow positive), and dislocated (Ortolani positive). All except those graded as normal were referred for examination by a pediatric orthopedic surgeon.
Treatment was initiated immediately after examination for those who had Barlow or Ortolani positive hips. For those who were considered to have an unstable or potentially unstable hip, a dynamic sonographic investigation was performed [6]. If more than 25% of the femoral head could be dislocated using this technique, the hip was considered unstable and treatment with the von Rosen splint was initiated. The splint was worn day and night and parents were informed not to take it off. All patients were bathed and examined by a nurse weekly at our outpatient clinic. The only difference in treatment between the comparison group and the study group was that the comparison group had been treated in the von Rosen splint for 12 weeks instead of 6.
Outcome measurements
The acetabular index (AI) was measured according to Tönnis on the 12-month follow-up radiograph as the roof angle (Figure 1) [7]. The inter- and intra-observer error is low when measuring AI [8]. Avascular necrosis of the femoral head (AVN) was assessed according to the Kalamchi–MacEwen classification [9]. Additional treatments, such as prolonged treatment in the von Rosen splint or treatment with the CAMP abduction orthosis, and complications, such as dislocations or AVN, were documented from patients’ medical records.
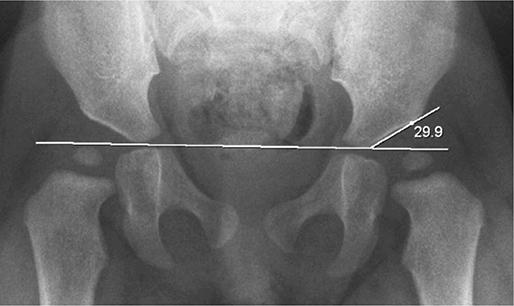
Figure 1. Left-sided AI measurement of a 12-month old girl who had bilaterally Barlow positive hips at birth [8]. AI is measured by drawing a line between the 2 triradiate cartilages (Hilgenreiner line) and measuring the angle with a second line drawn through the lateral acetabular roof.
Statistics
Non-inferiority testing was used by calculating the 95% confidence interval (CI) and using 1 as the equivalence margin to calculate if there was a difference in AI between the 2 groups [10]. The estimated mean AI with CI is presented. We estimated that with a standard deviation (SD) of 4 we needed 258 hips to attain 80% power to show non-inferiority between the 2 groups’ AI. Data analysis was performed using IBM SPSS Statistics version 27 (IBM Corp, Armonk, NY, USA).
Ethics, data sharing, funding, and disclosures
The Swedish ethical review authority approved the present study (2020-04747). Parents gave verbal informed consent upon entry in the registry. The study was supported by a grant from the Kockska Foundation and Stiftelsen för medicinsk vetenskaplig forskning inom ortopedi vid Malmö Allmänna Sjukhus. Pseudonymized study data can be obtained upon request, including ethical board approval, to the corresponding author. All authors declare that they have no conflict of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.13649
Results
Of 259 patients in the prospective registry, 26 patients were excluded. 99 patients (129 pathological hips) were treated for 6 weeks, and 134 patients (183 pathological hips) were treated for 12 weeks (Table, Figure 2).
| Factor | Patients | Hips | Day of treatment start a | Additional treatment before 12 months b | AI > 30° at 12 months c | AI at 12 months mean (CI) |
| 6 weeks | 99 | 129 | 5 (1–12) | 8 (8) | 11/127 (9) | 25° (24–26) |
| 12 weeks | 134 | 183 | 2 (1–7) | 0 | 16/183 (9) | 25° (25–26) |
| Total | 233 | 312 | 3 (1–12) | 8 (3) | 27/310 (9) | 25° (25–26) |
| a mean (range); b n (% of patients); c n/N (% of hips) | ||||||
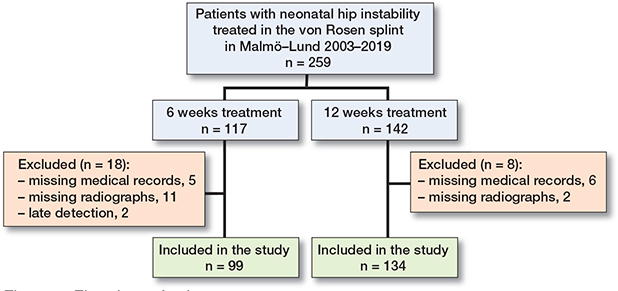
Figure 2. Flowchart of cohort.
There was no difference in sex or age between groups (Table 1). 1 patient with a left-sided hip dislocation was excluded from the AI calculations, diagnosed at the 3-month check-up.
The mean AI at 12 months in the 6-week group was 25° (CI 24–26) compared with 25° (CI 25–26) in the 12-week group (Figure 3, Table). Non-inferiority was demonstrated for the 6-week treatment group: –0.2° (CI –1.1 to 0.7) (Figure 4). In both groups 9% of patients had an AI > 30° at the 12-month follow-up.
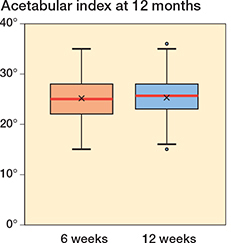
Figure 3. Acetabular index at 12 months ±1 month, patients with additional treatment included (except 1 patient with a dislocation). Box = interquartile range, whiskers = 1.5 x IQR values, red line = median, X = average, dot = outlier.
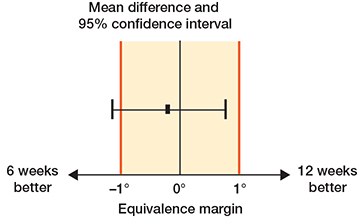
Figure 4. Non-inferiority within a 95% CI and 1° equivalence margin.
There was no case with additional treatment during the first year in the 12-week group and no patient with AVN in either group. In the 6-week group we found additional treatments during the first year in 8 cases:
- – 2 patients with clinically unstable hips at the 6-week follow up were treated for an extra 2 weeks in the von Rosen splint.
- – 5 patients with radiological dysplasia at the 3-month follow-up, of whom 4 had additional treatment with the CAMP abduction splint nightly for 3–6 months, and 1 patient until the 12-month follow-up.
- – 1 patient had a left-sided hip dislocation at the 3-month follow-up that required surgical treatment and was excluded from AI calculations. At inclusion, that child had bilateral Barlow positive hips.
If we exclude the 7 cases that were given additional treatment, the mean AI in the 6-week group changes minimally from 25° (CI 24–26) to 25° (CI 24–26) and the non-inferiority result from –0.2° (CI –1.1 to 0.7) to –0.5° (CI –1.4 to 0.4).
Discussion
The aim of the study was to establish whether a shortened treatment length from 12 to 6 weeks with the von Rosen splint would reduce the efficacy of our neonatal DDH treatment. This appears not to be the case as AI was similar in the 2 groups, but more additional treatments and complications occurred. Our finding that the shortened treatment length yields similar results has implications for health economics, as well as for minimizing discomfort in patients and their parents, where anxiety related to treatment with abduction splints is common. The finding of a therapy-resistant dislocation at 3 months indicates the need for standardized follow-up. This is further supported by the finding that 7 cases in the 6-week group were judged to have either persistent instability or radiographic dysplasia at the 3-month visit. It is impossible to say whether the therapy-resistant dislocation could have been prevented with 12 weeks of treatment as it is such a rare complication and it is unknown when the dislocation occurred. This is further supported by the finding that 7 cases in the 6-week group were judged to have either persistent instability or radiographic dysplasia at the 3-month visit. However, it is also possible that the change in treatment protocol per se contributed to the additional treatments in the 6-week group. Since 2012 (i.e., the 6-week group), calculation of AI at the 12-month radiographic examination is mandatory at our department, and patients with AI 28–30 are given an additional radiographic examination at 18 months of age. Patients with an AI > 30 are given nightly abduction orthosis treatment for 3 months. Until 2012 (i.e., the 12-week group), the radiographs were merely “eye-balled” to exclude dislocation or obvious dysplasia, such as lateralization or a broken Shenton’s line. The more thorough examination of radiographs since 2012 may have lowered the threshold for additional treatment at the 3-month visit. At 10–12 months of age an AI above 27–29° is often considered as “severe dysplasia” (based on 2 SD above the mean in a cohort study published in 1976) [7]. We find it reassuring not only that the mean AI was non-inferior after 6 weeks treatment, but also that outliers with high AI values were not more common after the shortened treatment.
Results with the von Rosen splint have been reported to be superior to other splints in treatment of newborns [11], and the treatment is safe with regards to AVN, which is why we have continued to use this method for more than 60 years [12]. In 2006 Lauge-Pedersen et al. [5] published a retrospective study concluding that 6 weeks of treatment with the von Rosen splint is sufficient to treat DDH in newborns. They included all patients with hip instability found through primary clinical screening and made no distinction between unstable and dislocated hips. In that study, 6 of 247 patients needed additional treatment, including 2 percutaneous tenotomies. Previously, Sahlstrand et al. reported that treatment for 8 weeks is sufficient [13]. Our study confirms that 6 weeks of treatment appears to be sufficient in Barlow and Ortolani positive hips, and in contrast to the previous publications we have quantified radiographic hip development and compared the results with a control group with 12 weeks treatment. In Sweden, late diagnosed DDH is defined as older than 2 weeks of age. Since the clinical screening program was instituted, the incidence of late diagnosed hip dislocations has decreased from at least 0.9 per 1,000 to 0.12 per 1,000 live births [14]. This is almost a 10-fold decrease over 50 years.
The concept of overtreatment is a problem that must be discussed in this context. A number of hips that are unstable neonatally will stabilize without treatment, some already during the first week of life [15]. As the outcome is dependent on early treatment start, at least well documented for slightly older children, and as treatment in newborns is safe, we accept some overtreatment [12,16]. An alternative method is to follow patients clinically, and by later sonographic examinations of hip morphology determine which need treatment. We believe this to be a sound policy in settings where clinical screening of newborns is ill organized (i.e., left to junior physicians). It is important to understand that both clinical hip examination and sonography are user-dependent tests. Nationwide studies on hip screening programs relying on sonographic examinations have reported improvements compared with pre-screening times, but slightly inferior results compared with the Swedish nationwide registry [14,17,18]. One thing that seems fairly clear is that selective sonographic screening based on risk factors is ineffective, probably as risk factors such as breech position in utero are present in only a minority of patients with hip dislocation [14,19].
Limitations
One limitation of this study is that clinicians performed AI measurements more thoroughly during the later study period, which may have affected the frequency of additional treatments. One aspect of this study that could be debated is whether AI is a good measurement to grade the progress of DDH or not. The acetabular notch, an anatomical feature that can be visible on radiographs and may affect the measurement of AI values, was not taken into account in our measurements [20]. It is, however, unlikely that this would affect our conclusions as it introduces a systematic error that would be the same for both groups.
Conclusion
Hip development, evaluated by the AI, was equal at 12 months of age following treatment in the von Rosen splint for 6 weeks compared with 12 weeks. 6 weeks of treatment with the von Rosen splint seems sufficient for Barlow and Ortolani positive hips. One case of hip dislocation detected at age 3 months indicates a need for standardized follow-ups irrespective of treatment length.
- Düppe H, Danielsson L G. Screening of neonatal instability and of developmental dislocation of the hip: a survey of 132,601 living newborn infants between 1956 and 1999. J Bone Joint Surg Br 2002; 84(6): 878-85. doi: 10.1302/0301-620x.84b6.12326.
- von Rosen S. Early diagnosis and treatment of congenital dislocation of the hip joint. Acta Orthop Scand 1956; 26(2): 136-55.
- Ortolani M. Congenital hip dysplasia in the light of early and very early diagnosis. Clin Orthop Relat Res 1976; (119): 6-10.
- Barlow T G. Congenital dislocation of the hip in the newborn. Proc R Soc Med 1966; 59(11 Part 1): 1103-6.
- Lauge-Pedersen H, Gustafsson J, Hägglund G. 6 weeks with the von Rosen splint is sufficient for treatment of neonatal hip instability. Acta Orthop 2006; 77(2): 257-61. doi: 10.1080/17453670610045993.
- Dahlström H, Oberg L, Friberg S. Sonography in congenital dislocation of the hip. Acta Orthop Scand 1986; 57(5): 402-6. doi: 10.3109/17453678609014757.
- Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res 1976; (119): 39-47.
- Wenger D, Düppe H, Tiderius C J. Acetabular dysplasia at the age of 1 year in children with neonatal instability of the hip. Acta Orthop 2013; 84(5): 483-8. doi: 10.3109/17453674.2013.850009.
- Kalamchi A, MacEwen G D. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am 1980; 62(6): 876-88.
- Hahn S. Understanding noninferiority trials. Korean J Pediatr 2012; 55(11): 403-7. doi: 10.3345/kjp.2012.55.11.403.
- Wilkinson A G, Sherlock D A, Murray G D. The efficacy of the Pavlik harness, the Craig splint and the von Rosen splint in the management of neonatal dysplasia of the hip: a comparative study. J Bone Joint Surg Br 2002; 84(5): 716-9. doi: 10.1302/0301-620x.84b5.12571.
- Wenger D, Samuelsson H, Düppe H, Tiderius C J. Early treatment with the von Rosen splint for neonatal instability of the hip is safe regarding avascular necrosis of the femoral head: 229 consecutive children observed for 6.5 years. Acta Orthop 2016; 87(2): 169-75. doi: 10.3109/17453674.2015.1126158.
- Sahlstrand T, Malmgren N, Ahlgren S A, Helgason H, Nilsson J. Management of neonatal hip instability: an analysis of the efficiency in a consistent treatment program. J Pediatr Orthop 1985; 5(5): 540-5.
- Wenger D, Düppe H, Nilsson J-Å, Tiderius C J. Incidence of late-diagnosed hip dislocation after universal clinical screening in Sweden. JAMA Network Open 2019; 2(11): e1914779-e1914779. doi: 10.1001/jamanetworkopen.2019.14779.
- Barlow T G. Early diagnosis and treatment of congenital dislocation of the hip. J Bone Joint Surg Br 1962; 44-B(2): 292-301.
- Albinana J, Dolan L A, Spratt K F, Morcuende J, Meyer M D, Weinstein S L. Acetabular dysplasia after treatment for developmental dysplasia of the hip: implications for secondary procedures. J Bone Joint Surg Br 2004; 86(6): 876-86. doi: 10.1302/0301-620x.86b6.14441
- von Kries R, Ihme N, Oberle D, Lorani A, Stark R, Altenhofen L, et al. Effect of ultrasound screening on the rate of first operative procedures for developmental hip dysplasia in Germany. Lancet 2003; 362(9399): 1883-7.
- Thallinger C, Pospischill R, Ganger R, Radler C, Krall C, Grill F. Long-term results of a nationwide general ultrasound screening system for developmental disorders of the hip: the Austrian hip screening program. J Child Orthop 2014; 8(1): 3-10.
- Broadhurst C, Rhodes A M L, Harper P, Perry D C, Clarke N M P, Aarvold A. What is the incidence of late detection of developmental dysplasia of the hip in England?: a 26-year national study of children diagnosed after the age of one. Bone Joint J 2019; 101-b(3): 281-7.
- Boniforti F G, Fujii G, Angliss R D, Benson M K. The reliability of measurements of pelvic radiographs in infants. J Bone Joint Surg Br 1997; 79(4): 570-5.