Factors influencing functioning after volar locking plate fixation of distal radius fractures: a scoping review of 148 studies
Susanne BOEL 1–3, Anders VINTHER 1,4, Alice Ø HANSEN 2,5, Carsten B JUHL 1,6, Marcus LANDGREN 7,8, Nicolaj S JACOBSEN 5, Camilla P PAULSEN 9, Claus T JØRGENSEN, and Hanne Kaae KRISTENSEN 2,3,10
1 Department of Physiotherapy and Occupational Therapy, Copenhagen University Hospital, Herlev and Gentofte; 2 Department of Clinical Research, University of Southern Denmark, Odense; 3 Centre for Innovative Medical Technology, Odense University Hospital, Odense; 4 Hospital Secretariat and Communications, Research, Herlev and Gentofte, Copenhagen University Hospital; 5 Department of Orthopedic Surgery and Traumatology, Odense University Hospital, Odense; 6 Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense; 7 Department of Orthopedic Surgery, Hand Surgery Unit, Herlev and Gentofte, Copenhagen University Hospital; 8 Department of Evidence-Based Medicine (EBM), Danish Health Authority, Copenhagen; 9 Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen; 10 Health Sciences Research Centre, UCL University College, Odense, Denmark
Abstract
Background and purpose — A better understanding of factors that influence functioning may improve the identification of patients with distal radius fractures (DRFs) who need hand therapy. The purpose of this scoping review was to provide a comprehensive overview of factors that have been evaluated for their influence on hand functioning following volar plate fixation of DRFs.
Material and methods — 6 databases were searched from 2005 to 2021 for publications regarding surgical treatment for a DRF with a volar locking plate. Included studies evaluated demographic, perioperative, and postoperative factors within the 6 weeks post-surgery for their influence on functioning at least 3 months post-surgery. Functioning was assessed with patient-reported outcome measures. The factors were categorized into themes and mapped to the International Classification of Functioning, Disability and Health (ICF).
Results — 148 studies were included. 708 factors were categorized into 39 themes (e.g. pain) and mapped to the ICF components. The themes were primarily mapped to “body functions and structures” (n = 26) and rarely to “activities and participation” (n = 5). Fracture type (n = 40), age (n = 38), and sex (n = 22) were the most frequently evaluated factors.
Conclusion — This scoping review identified an extensive number of factors evaluated within 6 weeks after surgery for their influence on functioning at least 3 months after volar plate fixa tion of a DRF and the existing research has primarily evaluated factors related to “body functions and structures,” with limited focus on factors related to “activities and participation.”
Citation: Acta Orthopaedica 2023; 94: 280–286. DOI https://doi.org/10.2340/17453674.2023.13431.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-28. Accepted: 2023-04-23. Published: 2023-06-07.
Correspondence: Susanne.boel.01@regionh.dk
SB, AV, CBJ, HHK, AØH, ML: authored the protocol (9). SB: performed database searches. SB, AV, NSJ, CPP, CTJ: conducted the study selection process. SB, NSJ, CPP, CTJ: performed data extraction. AV, AØH, ML: acted as 3rd reviewers. SB, AØH: categorized factors into themes and mapped factors to ICF components. HHK, AV, CBJ: resolved disagreements and verified the factor mapping. SB: wrote and edited the manuscript. All authors: reviewed and accepted the final version of the manuscript.
Handling co-editor: Taco Gosens
Acta thanks Johannes Mayr and Anne Vochteloo for help with peer review of this manuscript.
The rehabilitation approach offered to patients with a surgically treated distal radius fracture (DRF) relies on the healthcare professionals’ clinical experience and assessment of range of motion, edema, and pain (1). However, these clinical findings do not encapsulate all aspects of a patient’s functioning (2). Factors such as age, osteoporosis, associated ligament injuries, and personal preferences may provide additional information that enhances clinicians’ identification of patients who might benefit from treatments such as hand therapy.
Functioning is defined in the International Classification of Functioning, Disability and Health (ICF) as an interaction between a patient’s health condition, and the components “body functions and structures,” “activities and participation,” “environmental factors,” and “personal factors” (3). An understanding of functioning is important for framing patients’ health status (3) and should be considered in patients with DRFs (4). The evaluation of patients’ level of functioning with patient-reported outcomes measures (PROMs) may improve clinicians’ understanding of their needs and facilitate the planning of targeted rehabilitation approaches for patients at risk of insufficient functioning (5).
While systematic reviews have been published evaluating the effect of specific factors, such as pronator quadratus repair (6) and duration of immobilization (7) on functioning, we found no systematic reviews that provided an overview of all factors that may influence functioning after volar locking plate fixation. A variety of heterogeneous factors have been investigated for their influence on functioning. We therefore performed a scoping review with the purpose of providing a comprehensive overview of factors that have been evaluated for their influence on functioning following volar plate fixation of DRFs.
Methods
We conducted a scoping review using a replicable, transparent, and rigorous process and included a wide range of study designs consistent with scoping review methodology and guidelines (8). The review was performed based on the a priori published protocol (9), and deviations from the protocol are presented in Section 1 (see Supplementary data). The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (10).
Review question
Which demographic, perioperative, and postoperative factors within 6 weeks after surgery have been evaluated for their influence on functioning at least 3 months after volar plate fixation of a DRF?
Eligibility criteria
At least 75% of the study’s participants had to fulfill the following criteria to be included in the review: ≥ 18 years of age, had surgery within 3 weeks after trauma, and were treated with a volar locking plate (Table 1). If a volar plate was inserted in 2005 or later, we assumed that a locking plate was used. Functioning needed to be evaluated at least 3 months after surgery, based on the systematic review by Stinton et al. (11).
| Patient | Adults (≥ 18 years) treated with volar locking plate fixation within 3 weeks after a distal radius fracture |
| Concept | Factors: Demographic, perioperative, and postoperative factors evaluated within 6 weeks after surgery Functioning: Evaluated at least 3 months after surgery either qualitatively or with the following patient-reported outcome measures of functioning and their variations commonly used in distal radius fractures (43): Patient-Rated Wrist Evaluation (PRWE), Patient-Rated Wrist/Hand Evaluation (PRWHE), Disabilities of the Arm, Shoulder and Hand (DASH), QuickDASH, Michigan Hand Outcomes Questionnaire (MHQ), and BriefMHQ |
| Context | Any context regardless of country or healthcare setting |
Types of sources and search strategy
We considered peer-reviewed full-text studies in English, Danish, Norwegian, or Swedish with any study design. Systematic reviews published within the last 5 years were initially included to allow their reference lists to be checked for relevant studies.
The MEDLINE, CINAHL, Embase, Cochrane Library, PsycINFO, and SPORTdiscus databases were searched for studies published from 2005 until November 23, 2021, which reflected the time frame of volar locking plate fixation becoming common practice (12). The search strategy for MEDLINE is shown in Section 2 (see Supplementary data). The same search strategy was adapted and employed in the other database searches.
Study selection and data extraction
All identified citations were uploaded into the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia), and duplicates were removed. The screening of titles and abstracts (SB, AV), assessment of full-text studies against the inclusion criteria (SB, AV/CPP/NSJ/CTJ), and extraction of data (SB, CPP/NSJ) were performed by 2 reviewers independently. Any disagreements were resolved through discussion between the reviewers or by arbitration with a 3rd reviewer (AV/AØH). The following data was extracted: source (first author, country, year published), study design, study aim, postoperative rehabilitation, sample characteristics, DRF classification, plate type, factors evaluated, PROM used to evaluate functioning, and time points employed to assess functioning. Section 3 (see Supplementary data) outlines the operationalization of the data-extraction process.
Data analysis and presentation
The factors were categorized into themes by 2 reviewers (SB, AØH). For example, the theme “pain” contained the factors pain medication (13), pain at rest (14), and pain measured with the Pain Catastrophizing Scale (15). Likewise, depression (14,15), comorbidities (16,17), polytrauma (18), and diabetes (19,20) were factors included in the theme “comorbidities.” Factors that were evaluated from multiple perspectives or at multiple time points in the same study were only reported once.
Data was analyzed through content analysis (21). We identified the content of the factors based on the purpose of the assessments conducted in the original research and the manner in which the factors related to the ICF components (3). The content of each factor (22) was analyzed by 2 reviewers (SB, AØH) independently, and a 3rd reviewer was consulted if the determination of a factor’s content required discussion (ML). Each factor was mapped to 1 to 4 components of the ICF (3) that were most consistent with the factor’s content using the ICF linking rules (22,23) and the supplementary criteria developed for our review (Section 4, see Supplementary data; SB, AØH). The ICF components are defined in Table 2 and examples of factor mapping using the ICF framework is provided in Table 3. Disagreements during content analysis and factor mapping were resolved through arbitration with 3 additional reviewers, who also verified the factor mapping (AV, CBJ, HHK).
| Body functions and structures |
| “Body functions are the physiological functions of body systems including psychological functions” (3) “Body structures are anatomical parts of the body such as organs, limbs and their components” (3) |
| Activities and participation |
| “Activity is the execution of a task or action by an individual” (3) “Participation is involvement in a life situation” (3) |
| Environmental factors |
| “Environmental factors make up the physical, social, and attitudinal environment in which people live and conduct their lives” (3) |
| Personal factors |
| “Personal factors are the particular background of an individual’s life and living, and comprise features of the individual that are not part of a health condition or health status. These factors may include sex, race, age, other health conditions, fitness, lifestyle, habits, upbringing, coping styles, social background, education, profession…, all of which may play a role in disability at any level” (3) |
| First author | Factor evaluated in the original research | Content analysis | ICF category | ICF component |
| Uchiyama (44) | ||||
| Alendronate | Administration of alendronate | E1101 (drug handling) | Environmental factors | |
| Effect on bone healing and consequent influence on functioning | S73010 (structure of bones of forearm) | Body functions and structures | ||
| Choi (26) | ||||
| Osteoporosis | Osteoporosis | Comorbidity | Personal factors | |
| Effect of reduced density in the bone structure on functioning | S73010 (structure of bones of forearm) | Body functions and structures | ||
The 2 reviewers who carried out the content analysis and factor mapping (SB, AØH) are experienced occupational therapists with specialized knowledge of hand therapy and the use of the ICF framework in research. The content analysis was based on a biopsychosocial pre-understanding that a dynamic variety of factors influence patients’ functioning (2,3).
The factor mapping to the ICF classification was presented as frequency counts of studies assessing factors within each theme.
Results
Study selection
After the study selection process, 147 studies met the inclusion criteria and were included. An additional study was included after checking the reference lists of the included studies; thus, 148 studies were included in the scoping review (Figure 1).
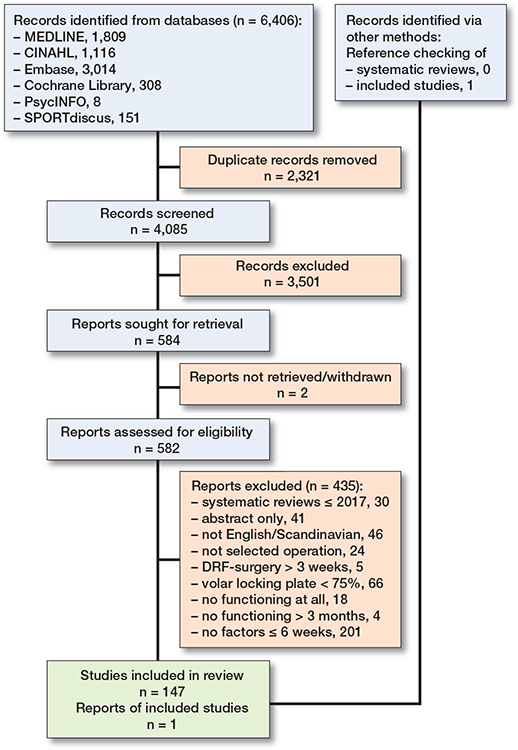
Figure 1. PRISMA-ScR flow diagram. DRF: distal radius fracture.
Study characteristics
The largest number of included studies originated from Europe (n = 57) and Asia (n = 57), followed by North America (n = 29), South America (n = 4), and Oceania (n = 1). Studies with the following designs were included: randomized controlled trials with data extracted from 2 or 3 treatment groups (n = 32), randomized controlled trials with data extracted from only 1 treatment group (n = 4), non-randomized controlled trials (n = 14), prospective cohort studies (n = 41), retrospective cohort studies (n = 48), case-control studies (n = 5), and case series studies (n = 4). The distributions of study publication year and employed PROMs are shown in Figures 2 and 3 (see Supplementary data). In 27 of the 148 studies, 2 different PROMs were employed: Disabilities of the Arm, Shoulder and Hand (DASH) and Patient-Rated Wrist Evaluation (PRWE) (n = 15) or QuickDASH and PRWE (n = 12; Table 5, see Supplementary data).
The 148 studies evaluated a total of 708 factors (Table 5, see Supplementary data). The factors were categorized into 39 themes, of which 23 themes were evaluated in more than 2 studies.
Factors mapped to components of the ICF classification
Of the 148 included studies, 138 studies evaluated 1 or more factors in “body functions and structures,” 43 studies evaluated 1 or more “personal factors,” 85 studies evaluated 1 or more “environmental factors,” 14 studies evaluated 1 or more factors in “activities and participation,” and 3 studies evaluated factors not covered or defined in the ICF classification. 42 studies evaluated only factors in 1 ICF component, while 7 studies evaluated factors in all 4 ICF components.
The themes and the frequency of studies reporting factors within the themes mapped to the ICF components are depicted in Figure 4. The factor mapping revealed most themes related to “body functions and structures” (n = 26), followed by “environmental factors” (n = 17) and “personal factors” (n = 11), while themes were least often mapped in “activities and participation” (n = 3; Figure 4).
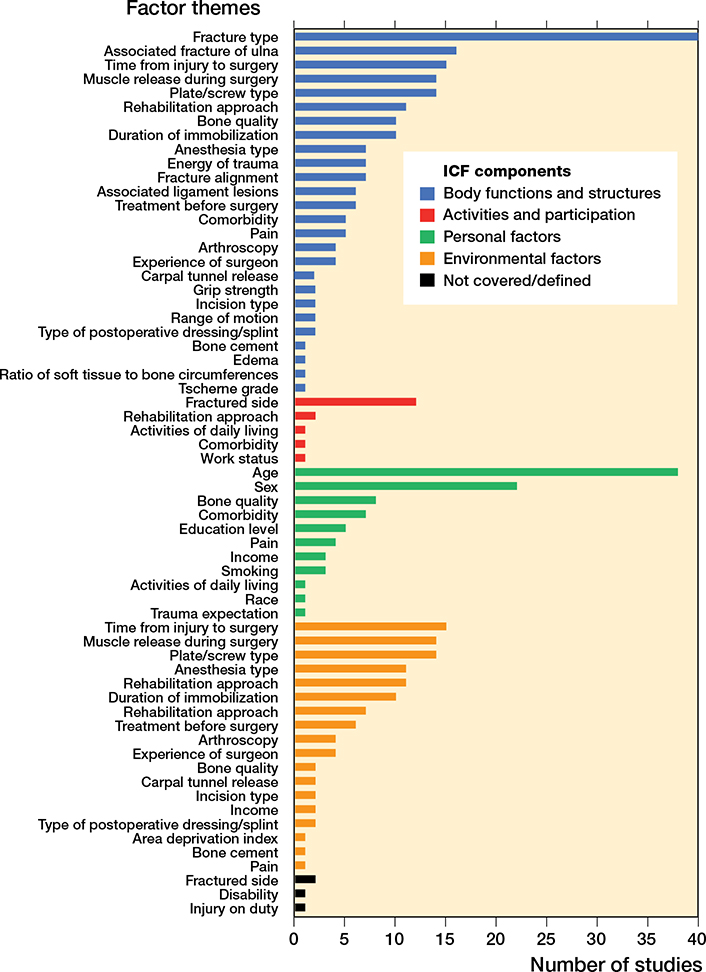
Figure 4. Factor themes and frequency of studies reporting factors within each ICF component. ICF = International Classification of Functioning, Disability and Health.
The themes fracture type (n = 40), age (n = 38), and sex (n = 22) were extensively evaluated, while factors representing patients’ perceptions of their health status were evaluated in only 5 studies that assessed trauma expectation, depression, pain, performance of activities of daily living, and disability.
Discussion
The study aimed to provide a comprehensive overview of factors that have been evaluated for their influence on hand functioning following volar plate fixation of DRFs. We found factors in all ICF components encompassing the perspective of functioning in patients with DRFs. This is in line with the 2009 ICF Core Set for Hand Conditions, which acknowledged the importance of reporting factors from all ICF components to measure functioning in patients with hand conditions (24). However, in our scoping review, we observed a tendency in the research to primarily evaluate factors related to “body functions and structures.” Interestingly, only 7 studies (14,15,25-29) evaluated factors in all 4 ICF components. The predominant evaluation of factors in “body functions and structures” is also evident in the hand therapy literature up to 2010 (30) and in the American Academy of Orthopedic Surgeons’ Clinical Practice Guideline for DRFs (31). The hand therapy literature has emphasized “body function and structures” and to a lesser extent “activities and participation,” and “environmental factors” (30) and “activities and participation” were not addressed in the Clinical Practice Guideline (31).
A patient’s rehabilitation approach (e.g., hand therapy or home-based exercises), often relies on the healthcare professional’s clinical experience, available resources, and interpretation of impairment measures of range of motion, edema, or pain (1). These factors were used as inclusion criteria for patients determined to not need supervised rehabilitation in a study by Boel and Juhl (32), which found that 42% of patients experienced insufficient functioning at 6 months after volar plate fixation of DRF, implying that these factors alone do not identify all patients in need of a rehabilitation approach that exceeds generic home exercises (32). Furthermore, the American Academy of Orthopedic Surgeons found that no established prognostic criteria enable the identification of the appropriate rehabilitation approach for all patients (33). As highlighted in the ICF framework, impairment-based factors alone do not provide a complete picture of the patient’s health status, and a dynamic variety of factors must be considered to identify patients at risk of experiencing insufficient postoperative functioning (2).
Our scoping review identified several factors that were evaluated in multiple studies and can thus serve as a future resource for researchers. For instance, future systematic reviews and meta-analyses can investigate how these factors affect functioning. The results of such systematic reviews would importantly strengthen the evidence base and aid in the development of guidelines to identify patients requiring individualized and specific rehabilitation approaches. Furthermore, they may inform the development of a decision aid that can be used to prepare and facilitate consultations between patients and healthcare professionals to promote shared and individualized decision-making regarding the rehabilitation approach that is compatible with the patient’s values (34).
Patients with DRFs have described having activity limitations, participation restrictions, and dependence on help from others in various life activities during the first 4 weeks following surgery (35). Patients with a variety of hand conditions have reported valuing several factors in the component of “activities and participation” as important aspects of functioning (24). In our scoping review, factors mapped to “activities and participation” were synthesized into 5 themes (“fractured side,” “rehabilitation approach,” “activities of daily living,” “comorbidities,” “work status”). With the exception of “fractured side,” these themes were evaluated in only a limited number of studies (14-16,32,36). As pointed out by patients with both DRFs and other hand conditions (24,35) and the ICF framework (3), performing activities and participating in everyday life situations are essential components of functioning, which highlights the need for further evaluation of factors related to “activities and participation” in future research.
Hall et al. argued that patient-reported factors impact the outcomes of patients with DRFs (37), and Hansen et al. found that “the level of sense of coherence” was associated with functioning in patients with hand-related disorders (38). These findings emphasize the importance of taking patients’ perceptions of their health status into consideration. Our scoping review included studies exploring patients’ perceptions through PROMs using predefined items (14,15,32,39,40). However, predefined items might only partially capture patients’ perspectives, as they may not reflect the factors of value for all patients (41). We found no qualitative studies that comprehensively captured patients’ perspectives. Future research with a qualitative design is thus warranted.
Strengths and limitations
A strength of this scoping review is the methodology of checking the included studies’ reference lists, as the core concept “factor” was difficult to capture in the keywords of the initial searches. We found only 1 additional study through the review of reference lists, implying that the search strategy was comprehensive. In addition, the extensive process of screening and extracting evidence was conducted by 6 reviewers, with the 1st author participating in all stages, which guaranteed a uniform approach throughout the review. Furthermore, the use of the linking rules developed by Cieza et al. (22,23) and the supplementary criteria developed for our review (Section 4, see Supplementary data) increased the reliability and transparency of the mapping process.
The primary limitation of our scoping review is the lack of citation tracking employed to identify studies citing the included studies. However, our review provides a comprehensive overview. We therefore believe that studies not identified in our search would be unlikely to contribute novel information to our review. Moreover, 10 studies did not report whether a locking plate was used. Volar locking plates were introduced in 2000 (42) and became the method of choice for displaced and non-reducible DRFs a few years later. Therefore, by selecting publications from 2005 onwards, we assumed that the risk of including patients treated with volar non-locking plates was minimal.
Conclusion
This scoping review identified an extensive number of factors evaluated within 6 weeks after surgery for their influence on functioning at least 3 months after volar plate fixation of a DRF. Our scoping review provides an overview of factors across the multifaceted perspective of functioning. Most factors were mapped to “body functions and structures,” while very few factors were mapped to “activities and participation.”
Supplementary data
Figures 2 and 3, Tables 4 and 5, Sections 1–4, and the complete list of references are available as Supplementary data on the article home page, DOI: 10.2340/17453674.2023.13431
List of abbreviations
BriefMHQ: Michigan Hand Questionnaire.
DASH: Disabilities of the Arm, Shoulder and Hand.
DRF: distal radius fracture.
ICF: International Classification of Functioning, Disability and Health.
MHQ: Michigan Hand Questionnaire.
PROMs: patient-reported outcome measures.
PRWE: Patient-Rated Wrist Evaluation.
PRWHE: Patient-Rated Wrist Hand Evaluation. QuickDASH: Quick Disabilities of the Arm, Shoulder and Hand.
- Handoll H H, Elliott J. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev 2015(9): Cd003324. doi: 10.1002/14651858.CD003324.pub3.
- Ustün T B, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: a new tool for understanding disability and health. Disabil Rehabil 2003; 25(11-12): 565-71. doi: 10.1080/0963828031000137063.
- World Health Organization (WHO). International Classification of Functioning, Disability and Health: ICF. Geneva: World Health Organization (WHO); 2001.
- Harris J E, MacDermid J C , Roth J. The International Classification of Functioning as an explanatory model of health after distal radius fracture: a cohort study. Health Qual Life Outcomes 2005; 3: 73. doi: 10.1186/1477-7525-3-73.
- Rehabilitation International Denmark [Internet]. Aarhus: Welcome to Rehabilitation International Denmark: Rehabilitation International Denmark; 2022 [cited 2023 Mar 24]. Available from: www.rehabiliteringsforum.dk/in-english/.
- Lu C-K, Liu W-C, Chang C-C, Shih C-L, Fu Y-C, Jupiter J B. A systematic review and meta-analysis of the pronator quadratus repair following volar plating of distal radius fractures. J Orthop Surg Res 2020; 15(1): 419. doi: 10.1186/s13018-020-01942-w.
- Gutierrez-Espinoza H, Araya-Quintanilla F, Olguin-Huerta C, Gutierrez-Monclus R, Jorquera-Aguilera R, Mathoulin C. Effectiveness of early versus delayed motion in patients with distal radius fracture treated with volar locking plate: a systematic review and meta-analysis. Hand Surg Rehabil 2021; 40(1): 6-16. doi: 10.1016/j.hansur.2020.10.007.
- Peters M D J, Marnie C, Tricco A C, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2020; 18(10): 2119-26. doi: 10.11124/JBIES20-00167.
- Boel S, Vinther A, Hansen A Ø, Juhl C B, Landgren M, Kristensen H K. Factors influencing functioning after volar locking plate fixation of distal radius fractures: a scoping review protocol. JBI Evid Synth 2022; 20(9): 2387-94. doi: 10.11124/JBIES-21-00459.
- Tricco A C, Lillie E, Zarin W, O’Brien K K, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169(7): 467-73. doi: 10.7326/M18-0850.
- Stinton S B, Graham P L, Moloney N A, Maclachlan L R, Edgar D W, Pappas E. Longitudinal recovery following distal radial fractures man-aged with volar plate fixation. Bone Joint J 2017; 99-b(12): 1665-76. doi: 10.1302/0301-620X.99B12.BJJ-2017-0348.R1.
- Wilcke M K T, Hammarberg H, Adolphson P Y. Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop 2013; 84(3): 292-6. doi: 10.3109/17453674.2013.792035.
- Luo P, Lou J, Yang S. Pain management during rehabilitation after distal radius fracture stabilized with volar locking plate: a prospective cohort study. BioMed Res Int 2018; 2018: 5786089. doi: 10.1155/2018/5786089.
- Souer J S, Buijze G, Ring D. A prospective randomized controlled trial comparing occupational therapy with independent exercises after volar plate fixation of a fracture of the distal part of the radius. J Bone Joint Surg Am 2011; 93(19): 1761-6. doi: 10.2106/JBJS.J.01452.
- Bot A G, Souer J S, van Dijk C N, Ring D. Association between individual DASH tasks and restricted wrist flexion and extension after volar plate fixation of a fracture of the distal radius. Hand (NY) 2012; 7(4): 407-12. doi: 10.1007/s11552-012-9447-8.
- Marchewka J, Szczechowicz J, Marchewka W, Golec E. Long-term outcomes and complications associated with operative and nonoperative treatment of distal radius fractures. Do we need to restore anatomy to have satisfactory clinical outcome? Folia Med Cracov 2021; 61(1): 35-48.
- Fitzpatrick S K, Casemyr N E, Zurakowski D, Day C S, Rozental T D. The effect of osteoporosis on outcomes of operatively treated distal radius fractures. J Hand Surg 2012; 37(10): 2027-34. doi: 10.1016/j.jhsa.2012.06.025.
- Hodel S, Schraner C, Oehme F, van Leeuwen R, Link B-C, Babst R, et al. Factors predicting adverse outcome in complete intra-articular distal radius fractures. Eur J Trauma Emerg Surg 2020; 46(6): 1413-9. doi: 10.1007/s00068-019-01102-8.
- Lee S J, Park J W, Kang B J, Lee J I. Clinical and radiologic factors affecting functional outcomes after volar locking plate fixation of dorsal angulated distal radius fractures. J Orthop Sci 2016; 21(5): 619-24. doi: 10.1016/j.jos.2016.05.007.
- Lee J I, Park K C, Joo I-H, Jeong H W, Park J W. The effect of osteoporosis on the outcomes after volar locking plate fixation in female patients older than 50 years with unstable distal radius fractures. J Hand Surg 2018; 43(8): 731-7. doi: 10.1016/j.jhsa.2018.05.028.
- Krippendorff K. Content analysis: an introduction to its methodology. 4th ed. Los Angeles, CA: SAGE Publications; 2018.
- Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil 2019; 41(5): 574-83. doi: 10.3109/09638288.2016.1145258.
- Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustün B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med 2005; 37(4): 212-18. doi: 10.1080/16501970510040263.
- Rudolf K D, Kus S, Chung K C, Johnston M, LeBlanc M, Cieza A. Development of the International Classification of Functioning, Disability and Health core sets for hand conditions: results of the World Health Organization International Consensus process. Disabil Rehabil 2012; 34(8): 681-93. doi: 10.3109/09638288.2011.613514.
- Chung K C, Kotsis S V, Kim H M. Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg Am 2007; 32(1): 76-83. doi: 10.1016/j.jhsa.2006.10.010.
- Choi W S, Lee H J, Kim D Y, Lee C H, Lee B G, Kim J H, et al. Does osteoporosis have a negative effect on the functional outcome of an osteoporotic distal radial fracture treated with a volar locking plate? Bone Joint J 2015; 97-B(2): 229-34. doi: 10.1302/0301-620X.97B2.34613.
- Roh Y H, Noh J H, Gong H S, Baek G H. Effect of low appendicular lean mass, grip strength, and gait speed on the functional outcome after surgery for distal radius fractures. Arch Osteoporosis 2017; 12(1): 41. doi: 10.1007/s11657-017-0335-2.
- Roh Y H, Lee B K, Noh J H, Oh J H, Gong H S, Baek G H. Factors delaying recovery after volar plate fixation of distal radius fractures. J Hand Surg Am 2014; 39(8): 1465-70. doi: 10.1016/j.jhsa.2014.04.033.
- Teunis T, Meijer S, van Leeuwen W, Jupiter J, Rikli D. Are radiographic characteristics associated with outcome in surgically treated distal radius fractures? J Hand Surg 2021; 15; S0363-5023(21)00615-8. doi: 10.1016/j.jhsa.2021.09.020.
- Rose B W, Kasch M C, Aaron D H, Stegink-Jansen C W. Does hand therapy literature incorporate the holistic view of health and function promoted by the World Health Organization. J Hand Ther 2011; 24(2): 84-8. doi: 10.1016/j.jht.2010.12.003.
- Esakki S, MacDermid J, Vajravelu S. Linking of the American Academy of Orthopaedic Surgeons Distal Radius Fracture Clinical Practice Guidelines to the International Classification of Functioning, Disability, and Health; International Classification of Diseases; and ICF Core Sets for Hand Conditions. Hand (N Y) 2016; 11(3): 314-21. doi: 10.1177/1558944715627305.
- Boel S, Juhl C B. The predictive value of disability at 2 weeks after plating of distal radial fractures: a prospective study of 101 patients. J Hand Surg Eur Vol 2022; 47(2): 150-6. doi: 10.1177/17531934211055935.
- American Academy of Orthopaedic Surgeons. Management of distal radius fractures evidence-based clinical practice guideline [Internet]. American Academy of Orthopaedic Surgeons; 2020 [cited 2022 Nov 25]. Available from: www.aaos.org/drfcpg.
- Stacey D, Légaré F, Lewis K, Barry M J, Bennett C L, Eden K B, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017; 4(4): Cd001431. doi: 10.1002/14651858.CD001431.pub5.
- Stern B Z, Howe T H, Njelesani J. “I didn’t know what I could do”: behaviors, knowledge and beliefs, and social facilitation after distal radius fracture. J Hand Ther 2021; S0894-1130(21)00146. doi: 10.1016/j.jht.2021.09.003.
- Heng B Q H, Lim J X Y, Chee K G, Kang Y C. Epidemiology of distal radius fixations and functional outcomes in the superelderly population. J Hand Surg Asian Pac Vol 2020; 25(1): 26-31. doi: 10.1142/S2424835520500034.
- Hall M J, Ostergaard P J, Rozental T D. Outcome measurement for distal radius fractures. Hand Clin 2021; 37(2): 215-27. doi: 10.1016/j.hcl.2021.02.004.
- Hansen A, Kristensen H K, Cederlund R, Möller S, Tromborg H. An occupation-based intervention in patients with hand-related disorders grouped using the sense of coherence scale: a randomized controlled trial. J Hand Ther 2020; 33(4): 455-69. doi: 10.1016/j.jht.2019.12.009.
- Roh Y H, Lee B K, Noh J H, Oh J H, Gong H S, Baek G H. Effect of anxiety and catastrophic pain ideation on early recovery after surgery for distal radius fractures. J Hand Surg Am 2014; 39(11): 2258. doi: 10.1016/j.jhsa.2014.08.007.
- Fang C, Fang E, Lau T-W, Fok M W M, Yee D K H, Pun T, et al. Patient expectations predict outcomes following distal radius fracture: a prospective cohort study using the TEFTOM questionnaire. Injury 2021; 52(4): 877-82. doi: 10.1016/j.injury.2020.10.091.
- Wright J G. Evaluating the outcome of treatment. Shouldn’t we be asking patients if they are better? J Clin Epidemiol 2000; 53(6): 549-53. doi: 10.1016/s0895-4356(99)00225-5.
- Orbay J L. The treatment of unstable distal radius fractures with volar fixation. Hand Surg 2000; 5(2): 103-12. doi: 10.1142/s0218810400000223.
- Goldhahn J, Beaton D, Ladd A, MacDermid J, Hoang-Kim A. Recommendation for measuring clinical outcome in distal radius fractures: a core set of domains for standardized reporting in clinical practice and research. Arch Orthop Trauma Surg 2014; 134(2): 197-205. doi: 10.1007/s00402-013-1767-9.
- Uchiyama S, Itsubo T, Nakamura K, Fujinaga Y, Sato N, Imaeda T, et al. Effect of early administration of alendronate after surgery for distal radial fragility fracture on radiological fracture healing time. Bone Joint J 2013; 95-B(11): 1544-50. doi: 10.1302/0301-620X.95B11.31652.
Complete list of references is available in Supplementary data.