No difference in 1-year improvement of patient-reported physical functioning and pain between resurfaced and unresurfaced patellae: analysis of 17,224 primary total knee arthroplasties in the Dutch Arthroplasty Register
Bart J ROBBEN 1, Astrid J DE VRIES 1, Liza N VAN STEENBERGEN 2, Rob G H H NELISSEN 2,3, and Reinoud W BROUWER 1
1 Department of Orthopaedic Surgery, Martini Hospital Groningen, Groningen; 2 Dutch Arthroplasty Register (LROI), ’s-Hertogenbosch; 3 Department of Orthopaedics, Leiden University Medical Center, Leiden, The Netherlands
Background and purpose — Whether or not to resurface the patella during primary total knee arthroplasty (TKA) remains controversial. We aimed to investigate the association between patellar resurfacing and patient-reported outcome measure (PROM) improvement 1 year postoperatively in terms of physical functioning and pain following TKA.
Patients and methods — We performed an observational study using the Dutch Arthroplasty Register on prospectively collected PROM data (n = 17,224, years 2014–2019). Preoperative and 1-year PROM pain scores (NRS at rest; during activity) and physical functioning scores (KOOS-PS, OKS) were examined. Stratification was performed for cruciate-retaining (CR) and posterior-stabilized (PS) and for the 4 most frequently used TKA implants in the Netherlands (Nexgen, Genesis II, PFC/Sigma, Vanguard) using multivariable linear regression adjusting for age, ASA classification, preoperative general health (EQ VAS), and preoperative PROMs.
Results — 4,525 resurfaced and 12,699 unresurfaced patellae in TKA were analyzed. Overall, no significant difference in 1-year PROM improvement was found between the 2 groups. In CR TKAs, resurfacing resulted in less improvement in KOOS-PS and OKS (adjusted difference between groups (B) –1.68, 95% confidence interval (CI) –2.86 to –0.50 and B –0.94, CI –1.57 to –0.31. Fewer improvements for patellar resurfacing in TKA were found for the Genesis TKA on NRS pain at rest (B –0.23, CI–0.40 to –0.06) and Oxford knee score (B –1.61, CI –2.24 to –0.98).
Conclusion — No significant differences were found in 1-year improvement of physical functioning and pain between TKA with resurfaced and unresurfaced patellae.
Citation: Acta Orthopaedica 2023; 94: 274–279. DOI https://doi.org/10.2340/17453674.2023.13430.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-10-12. Accepted: 2023-04-23. Published: 2023-06-05.
Correspondence: bjrobben@gmail.com
BR: design and interpretation of the work and writing of manuscript. AV: design of the work, analysis of the data, and revision. LS: analysis of the data and revision. RN: interpretation of work and revision. RB: design and interpretation of the work and revision. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Handling co-editors: Keijo Mäkelä and Philippe Wagner
Acta thanks Andrea Baldini, Stergios Lazarinis, and Ola Rolfson for help with peer review of this manuscript.
When performing a total knee arthroplasty (TKA) the surgeon has the choice to resurface the patella. Contradictory results exist among countries, making patellar resurfacing during primary TKA an ongoing topic of debate. There is also wide variation in the proportion of patellar resurfacing between national arthroplasty registries, ranging from 2% to 80% (1). In the Netherlands the patella is resurfaced in 21% of all 25,000 TKAs performed annually (2).
The main cause of anterior knee pain (AKP) after knee replacement is thought to be associated with osteoarthritis of the patellofemoral joint, which articulates with the metal femoral component. The design of the femoral prosthetic flange may thus play a role in the presence of patellofemoral problems after TKA. A less biomechanically optimal trochlear design may lead to AKP after TKA (3). Conflicting findings have been reported on secondary patellar resurfacing: it could reduce AKP and increase patient satisfaction, even though 36–41% of patients report having persistent postoperative complaints (4-6).
Conflicting evidence is also found for clinical outcomes of primary patellar resurfacing. While a recent meta-analysis showed statistically significant differences in Knee Society Scores (KSS) favoring patellar resurfacing (7), another showed no evidence that patellar resurfacing or prosthetic design affects the clinical outcome of a TKA (8).
The aim of our study is to investigate the association between patellar resurfacing and patient-reported outcome measure (PROM) improvement 1 year postoperatively for physical functioning and pain after TKA. A secondary aim was to investigate the association in the 4 most commonly used TKA implants, and the prosthesis design (CR/PS) for both males and females separately.
Patients and methods
This study is reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines.
Dutch Arthroplasty Register
The Dutch Arthroplasty Register (LROI) is a population-based register with information on all arthroplasties performed in the Netherlands. The LROI started in 2007 and 100% coverage of all Dutch hospitals was achieved in 2012. The increased reporting of arthroplasties in the register resulted in 96% completeness for primary TKAs in 2012 and 90% for knee revision in 2013 (9), reaching 99% for primary TKAs and 97% for knee revision arthroplasty in 2019 (10). The LROI contains information on patient characteristics, surgery, and prosthesis characteristics. In 2014, patient-reported outcome measures (PROMs) and BMI, smoking, and Charnley score were added to the register. The response rate for the PROMs for patients filling in preoperative and 1-year postoperative PROMs is on average 30–40%, with an increase over time (11). The opt-out system is used by the LROI, where completion of the questionnaires is considered to be implied consent.
Data selection
LROI TKA register data up to January 1, 2020 was obtained. All patients with primary osteoarthritis aged 18 years or older, with a primary TKA between January 1, 2014 and December 31, 2019, and who had PROM questionnaires available at all timepoints, were included. We included the 4 most commonly used TKA implants in the Netherlands: Genesis II (Smith and Nephew, Memphis, TN, USA), Nexgen (Zimmer Biomet, Warsaw, IN, USA), Vanguard (Zimmer Biomet, Warsaw, IN, USA), PFC/Sigma (DePuy Synthes, Warsaw, IN, USA). These total knee systems comprise 72% of all total knee implants used in the Netherlands between 2014 and 2019. The fifth most-used knee prosthesis in the Netherlands was the LCS (DePuy Synthes, Raynham, MA, USA); as only a limited proportion of patellae were resurfaced with this prosthesis (2.5%) and as it is no longer produced, the LCS was excluded from analysis.
PROMs
5 PROMs are registered in the LROI: (i) NRS pain at rest (range 0–10); (ii) NRS pain during activity (range 0–10); (iii) EQ VAS (scale 0–100) as a measure of general health status; (iv) Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS, range 0–100), which measures difficulties with activity due to knee-related problems; and (v) Oxford knee score (OKS) (range 0–48) as a measure of function and pain after TKA (12-14). These PROMs were prospectively collected preoperatively and 1 year postoperatively (14).
Statistics
Descriptive statistics were used to present the data, means, and standard deviations (SD) in ratio/interval data (normally distributed); numbers and frequencies were used for categorical data. 4 PROMs were considered relevant to assess clinical outcome after a TKA: NRS pain at rest, NRS pain during activity, KOOS-PS, and OKS. To analyze the improvement in these PROMs, the difference between preoperative and 1-year postoperative measurements was calculated. For all variables, a positive difference is an improvement. To determine whether there was a difference in improvement in PROMs between resurfaced and unresurfaced patellae in TKA, a complete-cases analysis of covariance (ANCOVA) was performed for each separate PROM, where the preoperative PROM was included as the covariate to correct for a potential effect of regression to the mean (15). Multivariable regression analysis was performed where the association between patellar resurfacing in improvement of PROMs—adjusting for age, ASA classification, general health (EQ VAS), and preoperative PROMs—was investigated, as done previously by Baker et al. (16). Adjustment variables were chosen based on their association with the outcome variable (the difference in NRS pain scores, KOOS-PS, and OKS) and their association with the choice whether or not to resurface the patella. The regression coefficients (beta) and the 95% confidence interval (CI) of patellar resurfacing (yes/no) were presented. An overall analysis and stratified analyses for cruciate-retaining (CR) and posterior-stabilized (PS) TKAs and sex as well as stratified analyses for the 4 most commonly used TKA implants were performed. As a measure of the fit of the regression models the adjusted R square was used. Prior to performing all statistical tests, the required assumptions were checked (e.g., normality and independent observations). Bilateral observations were left in the analysis and handled as being independent, as the proportion of bilateral observations is low and the sample size is large, as was discussed by Ranstam et al. (17). A P value below 0.05 was considered statistically significant. IBM SPSS version 25.0 (IBM Corp, Armonk, NY, USA) was used for the data analysis.
Ethics, funding, data sharing, and potential conflicts of interest
This study used data from the LROI, where data is collected for the purpose of improving quality of care, hence not falling under the scope of the Medical Research Involving Human Subjects Acts (WMO). A research dataset with anonymous patient data was obtained by the researchers; no approval by a local ethics committee was required. The authors received no funding and have no conflict of interest regarding this article. Completed disclosure forms for this article following the ICMJE template are available on the article page DOI: 10.2340/17453674.2023.13430
Results
Between 2014 and 2019, 143,954 primary TKAs for osteoarthritis were registered in the Netherlands, 30,588 (21.2%) of which underwent primary patellar resurfacing. Selecting the 4 most commonly used knee prostheses, 102,969 primary TKAs remained, 26,252 (24.8%) with primary patellar resurfacing. 17,224 TKA patients completed the PROMs at all time-points; the unresurfaced group had 12,669 (73.7%) patients and the resurfaced group 4,525 (26.3%) (Figure 1). Patients who filled out the PROMs were slightly younger (mean 68.3 [SD 8.5] vs. 69.0 [SD 9.6]) and had ASA III–IV classification less often (18% vs 20%) compared with those patients who did not complete the questionnaires. In total, 127 patients (0.7%) had a revision within 1 year, 93 patients (0.7%) in the unresurfaced group and 34 patients (0.8%) in the resurfaced group. Altogether, 683 bilateral patients were included in the dataset (4.0%). Percentages of primary patellar resurfacing between TKA implants are presented in Figure 2. There are some differences in the percentages of primary patellar resurfacing among the implants, with Genesis II at 22.6%, Nexgen 24.4%, PFC/Sigma 42.4%, and Vanguard 22.5%.
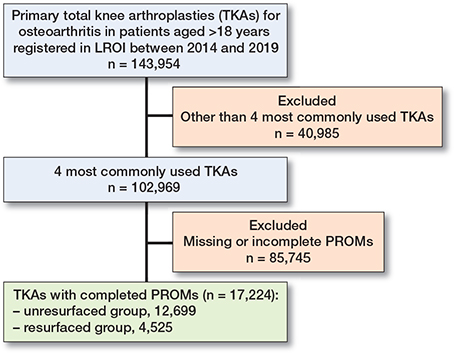
Figure 1. Flowchart of included and excluded patients.
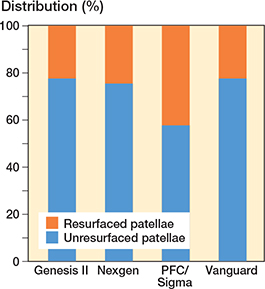
Figure 2. Percentages of primary patellar resurfacing of the 4 prosthesis types.
Baseline characteristics
Baseline characteristics showed that patients with resurfaced patellae were slightly younger, had a higher BMI, were more often female, had more ASA II and Charnley B1 classifications, and had a lower general health status (EQ VAS) than patients with unresurfaced patellae (Table 1).
PROMs
Comparing preoperative with 1-year postoperative PROMs, no significant difference in improvement at 1 year for physical functioning and pain relief was found between resurfaced and unresurfaced patellae (Table 2). Only on the OKS did the resurfaced group improve more than the unresurfaced patella group. In the multivariable analysis no significant difference was found between resurfaced and unresurfaced patellae (Table 2).
| Factor | Unresurfaced patellae mean (SD) | Resurfaced patellae mean (SD) | Difference between resurfaced and unresurfaced groups | |
| unadjusted score (CI) a | adjusted score (CI) b | |||
| NRS pain at rest (0–10) | 3.7 (2.9) | 3.8 (3.0) | 0.06 (–0.01 to 0.14) | –0.06 (–0.12 to 0.02) |
| NRS pain during activity (0–10) | 5.0 (2.9) | 5.1 (2.9) | 0.02 (–0.07 to 0.10) | 0.00 (–0.09 to 0.09) |
| KOOS-PS (0–100) | 22.8 (17.4) | 24.0 (18.1) | 0.14 (–0.36 to 0.64) | –0.08 (–0.58 to 0.42) |
| Oxford Knee Score (0–48) | 15.4 (8.8) | 15.4 (9.1) | 0.30 (0.03 to 0.56) c | –0.26 (–0.52 to 0.01) |
| a Unadjusted analyzed using ANCOVA with preoperative PROM as covariate. b Adjusted for age, EQ VAS, ASA classification, and the preoperative score of each PROM by including them in the regression model. c Significant difference. A positive difference indicates a difference favoring resurfacing for all outcomes. Numbers of preoperative PROMs missing: NRS pain at rest, n = 1,337; NRS pain during activity, n = 1,344; KOOS-PS, n = 322; Oxford knee score, n = 1,074. |
||||
Stratified analysis
CR-type prostheses with resurfaced patellae were associated with less improvement in KOOS-PS and OKS compared with unresurfaced patellae, when adjusted for confounders (Table 3). Male patients with resurfaced patellae showed less improvement in NRS pain at rest and OKS with CR-type prostheses and in OKS with PS-type prostheses compared with unresurfaced patellae. Female patients with resurfaced patellae showed less improvement in KOOS-PS with CR-type prostheses and more improvement in NRS pain during activity with PS-type prostheses than those with unresurfaced patellae. Adjusted analyses show that Genesis II TKAs with resurfaced patellae had less improvement 1 year post-operatively compared with preoperatively in NRS pain at rest and OKS than Genesis II TKAs with unresurfaced patellae (Table 4).
| Factor | n | Adjusted difference score (CI) a |
| NRS pain at rest (0–10) | ||
| CR | 5,231 | –0.16 (–0.33 to 0.02) |
| Males | 2,050 | –0.30 (–0.58 to –0.01) b |
| Females | 3,179 | –0.09 (–0.31 to 0.14) |
| PS | 10,346 | –0.03 (–0.12 to 0.05) |
| Males | 4,071 | –0.12 (–0.25 to 0.01) |
| Females | 6,270 | 0.02 (–0.09 to 0.14) |
| NRS pain during activity (0–10) | ||
| CR | 5,225 | –0.11 (–0.31 to 0.10) |
| Males | 2,052 | –0.19 (–0.53 to 0.14) |
| Females | 3,171 | –0.04 (–0.30 to 0.22) |
| PS | 10,345 | 0.03 (–0.07 to 0.13) |
| Males | 4,068 | –0.15 (–0.31 to 0.00) |
| Females | 6,272 | 0.15 (0.02 to 0.28)b |
| KOOS-PS (0–100) | ||
| CR | 5,326 | –1.7 (–2.9 to –0.50) b |
| Males | 2,149 | –1.6 (–3.6 to 0.48) |
| Females | 3,174 | –1.6 (–3.1 to –0.15) b |
| PS | 10,759 | 0.08 (–0.49 to 0.66) |
| Males | 4,305 | –0.39 (–1.4 to 0.56) |
| Females | 6,449 | 0.52 (–0.20 to 1.23) |
| Oxford knee score (0–48) | ||
| CR | 5,220 | –0.94 (–1.6 to –0.31) b |
| Males | 2,072 | –1.9 (–2.9 to –0.84) b |
| Females | 3,145 | –0.41 (–1.2 to 0.39) |
| PS | 10,297 | –0.09 (–0.39 to 0.22) |
| Males | 4,104 | –0.53 (–1.0 to –0.06) b |
| Females | 6,190 | 0.25 (–0.15 to 0.65) |
| CR = cruciate-retaining, PS = posterior-stabilized. a Adjusted differences correcting for differences in age, ASA classification, preoperative general health (EQ VAS), and the relevant preoperative PROMs score are reported. A positive difference indicates a difference favoring resurfacing. b Significant associations. |
||
| Factor | n | Adjusted difference score (CI) a |
| NRS pain at rest (0–10) | ||
| Nexgen | 5,060 | –0.05 (–0.18 to 0.07) |
| Genesis II | 3,672 | –0.23 (–0.40 to –0.06) b |
| FPC/Sigma | 2,584 | 0.01 (–0.15 to 0.17) |
| Vanguard | 4,272 | –0.08 (–0.23 to 0.07) |
| NRS pain during activity (0–10) | ||
| Nexgen | 5,059 | –0.03 (–0.18 to 0.12) |
| Genesis II | 3,668 | –0.11 (–0.31 to 0.08) |
| FPC/Sigma | 2,583 | 0.05 (–0.13 to 0.24) |
| Vanguard | 4,271 | –0.02 (–0.20 to 0.15) |
| KOOS-PS (0–100) | ||
| Nexgen | 5,641 | –0.34 (–1.2 to 0.52) |
| Genesis II | 3,615 | –0.94 (–2.0 to 0.16) |
| FPC/Sigma | 2,485 | 0.18 (–0.96 to 1.3) |
| Vanguard | 4,354 | 0.18 (–0.85 to 1.2) |
| Oxford knee score (0–48) | ||
| Nexgen | 5,534 | –0.03 (–0.47 to 0.41) |
| Genesis II | 3,305 | –1.6 (–2.2 to –0.98) b |
| FPC/Sigma | 2,443 | 0.33 (–0.24 to 0.91) |
| Vanguard | 4,247 | –0.23 (–0.77 to 0.32) |
| a Adjusted differences correcting for differences in age, ASA classification, preoperative general health (EQ VAS), and the relevant preoperative PROMs score are reported. A positive difference indicates a difference favoring resurfacing. b Significant associations. |
||
Discussion
Our study is the first national arthroplasty register study, using a large, unselected cohort to investigate the association between patellar resurfacing and physical functioning and pain improvement at 1-year follow-up. We found no significant difference in 1-year improvement on physical functioning and pain in patients after primary TKA with resurfaced patellae compared with those with unresurfaced patellae. Our stratified analysis showed that CR-type prostheses and Genesis II prostheses with resurfaced patellae led to significantly less improvement in physical functioning and pain than the unresurfaced patella TKAs. It is important to keep in mind that the small differences found in our study, although statistically significant, may not be clinically relevant.
No clinically relevant differences in 1-year postoperative PROM improvement were found between the resurfaced and unresurfaced groups, or in subgroups. This finding concurs with a meta-analysis of 18 RCTs with a cumulative sample size of 7,075 TKAs (8), 2 recent RCTs, and a systemic review (18-20). Deroche et al. (2022) performed 250 TKAs in 245 consecutive patients with a mean follow-up of 18 months, concluding there is no superiority of resurfaced over unresurfaced patellae in terms of clinical or radiological outcomes (19). One exception in that study was more pain when climbing stairs in the unresurfaced TKAs. However, Teel et al. showed no clinically relevant differences favoring resurfacing in the knee component and functional component of KSS (7). A meta-analysis by Longo et al. of 35 studies showed a significantly higher postoperative KSS and Hospital for Special Surgery score with patellar resurfacing (21). A limitation of the studies included in this trial is that they performed only univariable analysis, not correcting for other variables. 2 recent meta-analyses also showed some differences between patellar resurfacing and unresurfaced groups. Chen et al. (2021) concluded based on 32 RCTs that patellar resurfacing could reduce the reoperation rate and occurrence of a clunk or crepitus after surgery (22). Also, an increase in the KSS and function score was found in resurfaced patellae compared with unresurfaced patellae. No influence on outcomes such as AKP, range of motion, Oxford score, KOOS, VAS, Feller score, patellar tilt, and patient satisfaction could, however, be evidenced. We found that CR-type TKA prostheses and Genesis II TKA implants with resurfaced patellae showed less postoperative improvement than unresurfaced knees. An effect of TKA design was not found by Baker et al., who performed a linear regression analysis on the national Joint Register for England and Wales (16). As they analyzed the PROMs 6 months postoperatively, this might be too early to find a difference. Several RCTs with a PS-type TKA found a higher incidence of patellar crepitus and worse outcome of OKS and patellar score in unresurfaced TKAs (23,24). Our study shows that CR-type prostheses with patellar resurfacing result in less improvement on the functional outcome measures (KOOS-PS and OKS). Some studies suggest that more modern “patella-friendly” femoral designs outperform other TKA designs by reducing AKP and patellar complications in the unresurfaced knees (25,26). We compared resurfaced and unresurfaced knees for several surgical systems and saw no benefit of patellar resurfacing. The only significant difference was with the Genesis II prosthesis, favoring unresurfaced.
Male patients with resurfaces patellae showed less improvement in NRS pain at rest and OKS with a CR-type prosthesis and in OKS with a PS-type prosthesis compared with unresurfaced patellae. Female patients with resurfaced patellae showed less improvement than TKAs with unresurfaced patellae on KOOS-PS with a CR-type prosthesis and more improvement on NRS pain activity with a PS-type prosthesis. These results are also different from those of Baker et al., where no benefit was evidenced of resurfacing in CR- or PS-type prostheses, irrespective of patient gender (16). To our knowledge, no other studies have examined specific results for sex in relation to patellar resurfacing.
A major strength of this register study is 97% completeness for revision (annual report 2019) (10). This large cohort provides the possibility to perform regression analysis while adjusting for confounders. Our study also has some limitations. The majority of hospitals in the Netherlands perform a selective or rarely patellar resurfacing regime (2). We were unable to analyze the reason for patellar resurfacing in this register study. This makes the indication for patellar resurfacing a possible confounding variable. Second, the response rate for patients filling in either a preoperative or a 1-year postoperative PROM was relatively low (30–40% with an increase over time). This may have led to a selection bias. Third, there are no patella-specific items in the LROI for 2014–2019. It is unclear whether patients had AKP or patellofemoral arthrosis preoperatively, which could have contributed to the decision to resurface the patella. Also, the currently used PROMs might not be sensitive enough to specifically measure differences in AKP between the two groups, as a patellofemoral-specific questionnaire like the Kujala (Anterior Knee Pain Scale) is not part of the PROMs recommended by the Netherlands Orthopedic Association and therefore is not included in the LROI (27). However, we do think that the assessment of KOOS-PS, OKS, and NRS pain at rest and activity would nonetheless detect any present clinically relevant differences. Finally, one should be aware that by performing a series of different statistical tests on several different outcomes, as was done in this study, the risk of false-positive findings increases.
Conclusion
Our results show no difference in 1-year improvement of patient-reported physical functioning and pain scores between resurfaced and unresurfaced patellae after TKA. Our results add to the growing evidence that patellar resurfacing is not associated with better clinical outcomes.
- Fraser J F, Spangehl M J. International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014. J Arthroplasty 2017; 32(1): 83-6. doi: 10.1016/j.arth.2016.06.010.
- Robben B J, De Vries A J, Spekenbrink-Spooren A, Nelissen R G H H, Brouwer R W. Rare primary patellar resurfacing does not lead to more secondary patellar resurfacing: analysis of 70,014 primary total knee arthroplasties in the Dutch Arthroplasty Register (LROI). Acta Orthop 2022; 93: 334-40. doi: 10.2340/17453674.2022.2078.
- Popovic N, Lemaire R. Anterior knee pain with a posterior-stabilized mobile-bearing knee prosthesis: the effect of femoral component design. J Arthroplasty 2003; 18(04): 396-400. doi: 10.1016/s0883-5403(03)00059-7.
- Spencer S J, Young D, Blyth M J G. Secondary resurfacing of the patella in total knee arthroplasty. Knee 2010; 17(3): 187-90. doi: 10.1016/j.knee.2009.08.003.
- van Jonbergen H-P W, Boeddha A V, van Raaij J J A M. Patient satisfaction and functional outcomes following secondary patellar resurfacing. Orthopedics. 2016; 39(5): e850-6. doi: 10.3928/01477447-20160509-05.
- Pakos E E, Ntzani E E, Trikalinos T A. Patellar resurfacing in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am 2005; 87A: 1438-45. doi: 10.2106/JBJS.D.02422.
- Teel A J, Esposito J G, Lanting B A, Howard J L, Schemitsch E H. Patellar resurfacing in primary total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty 2019; 34(12): 3124-32. doi: 10.1016/j.arth.2019.07.019.
- Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am 2011; 93(14): 1301-9. doi: 10.2106/JBJS.J.00594.
- Van Steenbergen L N, Denissen G A W, Spooren A, van Rooden S M, van Oosterhout F J, Morrenhof J W, et al. More than 95% completeness of reported procedures in the population based Dutch Arthroplasty Register: external validation of 311890 procedures. Acta Orthop 2015; 86(4): 498-505. doi: 10.3109/17453674.2015.1028307.
- Dutch Arthroplasty Register (LROI). Previous annual online report of LROI. Available from: https://www.lroi-report.nl/previous-reports/ [Accessed January 28, 2021].
- Dutch Arthroplasty Register (LROI). Knee PROMS response rate. Available from: https://www.lroi-report.nl/knee/proms/response/ [Accessed August 30, 2022].
- Perruccio A V, Lohmander L S, Canizares M, Tennant A, Hawker G A, Conaghan P G, et al. The development of a short measure of physical function for knee OA: KOOS-Physical Function Short-form (KOOS-PS)—an OARSI/OMERACT Initiative. Osteoarthritis Cartilage 2008; 16: 542-50. doi: 10.1016/j.joca.2007.12.014/.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011; 20(10): 1727-36. doi: 10.1007/s11136-011-9903-x.
- Haverkamp D, Breugem S J M, Sierevelt I N, Blankevoort L, Van Dijk C N. Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop 2005; 76(3): 347-52.
- Barnett A G, van der Pols J C, Dobson A J. Regression to the mean: what is it and how to deal with it. Int J Epidemiol 2005: 34: 215-220. doi: 10.1093/ije/dyh299.
- Baker P N, Petheram T, Dowen D, Jameson S S, Avery P J, Reed M R, et al. Early PROMs following total knee arthroplasty: functional outcome dependent on patella resurfacing. J Arthroplasty 2014; 29(2): 314-9. doi: 10.1016/j.arth.2013.05.001.
- Ranstam J, Kärrholm J, Pulkkinen P, Mäkelä K, Espehaug B, Pedersen A B, et al. Statistical analysis of arthroplasty data, II: Guidelines. Acta Orthop 2011; 82(3): 258-67. doi: 10.3109/17453674.2011.588863.
- Van Raaij T M, van der Meij E, de Vries A J, van Raay J J M. Patellar resurfacing does not improve clinical outcome in patients with symptomatic tricompartmental knee osteoarthritis: an RCT study of 40 patients receiving primary cruciate retaining total knee arthroplasty. J Knee Surg 2021; 34(14): 1503-9. doi: 10.1055/s-0040-1710369.
- Deroche E, Batailler C, Swan J, Sappey-Marinier E, Neyret P, Servien E, et al. No difference between resurfaced and non-resurfaced patellae with a modern prosthesis design: a prospective randomized study of 250 total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc 2022; 30(3): 1025-38. doi: 10.1007/s00167-021-06521-y.
- Choi K Y, In Y, Kim M S, Sohn S, Koh I J. Is the patient aware of the difference between resurfaced and nonresurfaced patella after bilateral total knee arthroplasty? A systematic review of simultaneous bilateral randomized trials. Knee Surg Relat Res 2022; 34(1): 4. doi: 10.1186/s43019-022-00133-7.
- Longo U G, Ciuffreda M, Mannering N, D’Andrea V, Cimmino M, Denaro V. Patellar resurfacing in total knee arthroplasty: systematic review and meta-analysis. J Arthroplasty 2018; 33(2): 620-32. doi: 10.1016/j.arth.2017.08.041.
- Chen K, Dai X, Li L, Chen Z, Cui H, Lv S. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: an updated meta-analysis of randomized controlled trials. J Orthop Surg Res 2021; 16(1): 83. doi: 10.1186/s13018-020-02185-5.
- Thiengwittayaporn S, Srungboonmee K , Chiamtrakool B. Resurfacing in a posterior-stabilized total knee arthroplasty reduces patellar crepitus complication: a randomized, controlled trial. J Arthroplasty 2019; 34(9): 1969-74 . doi: 10.1016/j.arth.2019.04.050.
- Ogawa H, Matsumoto K, Akiyama H. Effect of patellar resurfacing on patellofemoral crepitus in posterior-stabilized total knee arthroplasty. J Arthroplasty 2016; 31(8): 1792-6. doi: 10.1016/j.arth.2016.01.023.
- Karachalios T, Komnos G, Hantes M, Varitimidis S. Evaluating the “patella-friendly” concept in total knee arthroplasty: a minimum 15-year follow-up outcome study comparing constant radius, multiradius cruciate-retaining, and nonanatomical cruciate-retaining implants. J Arthroplasty 2021; 36(8): 2771-8. doi: 10.1016/j.arth.2021.03.007.
- Huang Y-F, Gao Y-H, Ding L, Liu B, Liu J-G, Qi X. Influence of femoral implant design modification on anterior knee pain and patellar crepitus in patients who underwent total knee arthroplasty without patella resurfacing. BMC Musculoskelet Disord 2020; 21(1): 364. doi: 10.1186/s12891-020-03391-2.
- Kujala U M, Jaakkola L H, Koskinen S K, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy 1993; 9(2): 159-63. doi: 10.1016/s0749-8063(05)80366-4.