Minimum 20-year follow-up of a press-fit acetabular cup in cementless total hip replacement in young patients
Andre LUNZ 1, Moritz VON FALKENHAYN 1, Sebastian JAEGER 1, Tobias REINER 1, Christian MERLE 2, Marcus R STREIT 3, Tobias RENKAWITZ 1, and Moritz M INNMANN 1
1 Department of Orthopaedics, Heidelberg University Hospital, Heidelberg; 2 Diakonie Klinikum Stuttgart; 3 ARCUS Sportklinik, Pforzheim, Germany
Purpose — We aimed to determine the minimum 20-year survival rates of a cementless press-fit cup in young patients.
Patients and methods — This is a retrospective, single-center, multi-surgeon cohort study investigating the minimum 20-year clinical and radiological outcome of the first 121 consecutive total hip replacements (THRs) using a cementless, press-fit cup (Allofit, Zimmer, Warsaw, IN, USA) performed between 1999 and 2001. 28-mm metal-on-metal (MoM) and ceramic-on-conventionally not highly crosslinked polyethylene (CoP) bearings were used in 71% and 28%, respectively. Median patient age at surgery was 52 (range 21–60) years. Kaplan–Meier survival analysis was conducted for different endpoints.
Results — The 22-year survival rate for the endpoint aseptic cup or inlay revision was 94% (95% confidence interval [CI] 87–96) and 99% (CI 94–100) for aseptic cup loosening. 20 patients (21 THRs; 17%) had died and 5 (5 THRs; 4%) were lost to follow-up. No THR showed evidence of radiographic cup loosening. Osteolysis was observed in 40% of THRs with MoM and 77% with CoP bearings. 88% of THRs with CoP bearings showed significant polyethylene wear.
Conclusion — The investigated cementless press-fit cup, which is still in clinical use today, showed excellent long-term survival rates in patients under the age of 60 years at surgery. However, osteolysis due to polyethylene and metal wear was frequently observed and is a matter of concern in the third decade after surgery.
Citation: Acta Orthopaedica 2023; 94: 321–327. DOI: https://doi.org/10.2340/17453674.2023.13385.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-27. Accepted: 2023-04-23; Published: 2023-07-04.
Correspondence: andre.lunz@med.uni-heidelberg.de
Conceptualization: AL and MMI; formal analysis: AL, MvF, SJ, and MMI; investigation: AL and MvF; methodology: AL, MvF, SJ, TRr, CM, MRS, TRz, and MMI; supervision: TRz and MMI; visualization: AL, MvF, MRS, and MMI; writing—original draft: AL; writing—review and editing: AL, MvF, TRz, and MMI.
Handling co-editors: Keijo Mäkelä and Robin Christensen
Acta thanks Erik Lenguerrand, Jyrki Nieminen, and Marina Torre for help with peer review of this manuscript.
Cementless press-fit cups are being widely used worldwide. National arthroplasty registry data reports survival rates of 95% and 91% after 10 and 18 years, respectively (1,2). However, most registries lack data on radiological or functional outcome. Furthermore, there is no registry data on minimum 20-year survival rates for cementless cups that are still in clinical use today (1-3). In the long term, wear and osteolysis of especially not highly crosslinked polyethylene liners are at risk of causing aseptic loosening and consecutive failure of the total hip replacement (THR) (4,5), which is a particular problem for young patients with a longer life expectancy (6). Additionally, patients who are potentially at risk of revision cannot be identified in registry studies until revision surgery has taken place. Thus, data from retrospective long-term single-center studies including radiographic outcomes is a meaningful supplement to registry studies.
Therefore, we aimed to determine the radiographic results and cumulative survival rates at a minimum of 20 years of follow-up for the endpoints (1) acetabular revision for any reason, (2) acetabular revision for any aseptic reasons (including isolated inlay and femoral head revisions), (3) acetabular revision for aseptic loosening (without isolated inlay and femoral head revisions), and (4) survival in patients younger than 55 years at index surgery using the non-porous, uncemented, press-fit Allofit cup (Zimmer Biomet, Warsaw, IN, USA).
Patients and methods
This study is reported according to STROBE guidelines.
This retrospective, single-center, multi-surgeon, cohort study was conducted at the Orthopedic Department of Heidelberg University Hospital. We included the first 121 consecutive cementless THRs, using a cementless, grit-blasted, nonporous, titanium alloy press-fit cup (Allofit acetabular cup; Zimmer Inc., Warsaw, IN, USA) (Figure 1) in 116 patients. We have reported on the 10-year results of the present cohort in the past (7). All patients were followed up for a minimum of 20 years after index surgery and the data was collected using our institutional joint replacement registry (Table 1). The procedures were performed in a multi-surgeon series (17 surgeons) at our institution between January 1999 and June 2001. Osteoarthritis (64%), followed by congenital dysplasia of the hip (17%) and avascular necrosis of the femoral head (11%) were the most common diagnoses leading to THR in this cohort.
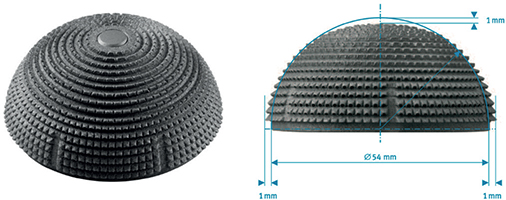
Figure 1. The uncemented acetabular press-fit component with macro-textured surface, hemispherical periphery, and a flattened polar region (Allofit; Zimmer Biomet, Warsaw, IN, USA).
| Factor | MoM (Metasul) | CoP (Sulene) | Total |
| Hips | 86 (71) | 34 (28) | 120 (99) |
| Patients | 83 (72) | 32 (28) | 115 (99) |
| Mean age (SD) | 50 (7.9) | 54 (6.5) | 51 (7.8) |
| Hips aged < 50 year | 32 (37) | 6 (18) | 38 (32) |
| Mean BMI (SD) | 27.3 (4.5) | 27.0 (4.7) | 27.2 (4.5) |
| Sex of hips (male:female) | 55:31 | 18:16 | 73:47 |
| Side (right:left) | 40:46 | 21:13 | 61:59 |
| Diagnosis | |||
| Osteoarthritis | 58 | 18 | 76 (63) |
| CDH | 14 | 7 | 21 (18) |
| Avascular necrosis | 6 | 7 | 13 (11) |
| other | 8 | 2 | 10 (8.3) |
| Femoral stem | |||
| CLS | 62 | 6 | 68 (57) |
| G2 | 22 | 27 | 49 (41) |
| other | 2 | 1 | 3 (2.5) |
| Surgical approach | |||
| Watson-Jones | 4 (4.7) | 4 (12) | 8 (6.7) |
| Bauer | 82 (95) | 30 (88) | 112 (93) |
| Mean inclination of cup (range) | 44° | 44° | 44° (27–62) |
| Inclination outside safe zone | 9 (10) | 6 (18) | 15 (13) |
| Any revision | 5 (4.1) | 3 (2.5) | 8 (6.6) |
| Liner revision only | 3 (3.5) | 1 (2.9) | 4 (3.3) |
| Dead | 12 (14) | 9 (27) | 21 (18) |
| Clinical and radiographic FU | 49 (57) | 17 (50) | 66 (55) |
| Clinical FU only | 13 (15) | 3 (8.8) | 16 (13) |
| Dropped out | 5 (5.8) | 3 (8.8) | 8 (6.7) |
| Lost to FU | 4 (4.7) | 1 (2.9) | 5 (4.2) |
| a One patient with one hip was treated with the only ceramic-on-ceramic (Cerasul) articulation in this patient cohort. He did not undergo any revision surgery and was not included in this table for the sake of clarity. CDH = congenital dysplasia of the hip, FU = follow-up. |
|||
The Allofit acetabular component is modular, allowing the use of different bearing surfaces. As bearings, either a 28-mm Metasul (Zimmer, Winterthur, Switzerland), forged, high-carbide (0.2%–0.25%) cobalt chrome (CoCr) alloy sandwich metal-on-metal articulation (86 hips) or a 28-mm Al2O3 ceramic head (Biolox forte; CeramTec, Plochingen, Germany) articulating with conventional (not-highly crosslinked) calcium stearate-free UHMW polyethylene liner (Sulene; Zimmer, Winterthur, Switzerland) (34 hips) was used. In one hip, a 28-mm Cerasul (Zimmer, Winterthur, Switzerland) sandwich ceramic-on-ceramic articulation was used. For femoral reconstruction, a cementless tapered titanium stem was used in 118 hips: 69 hips received a CLS Spotorno stem (Zimmer, Winterthur, Switzerland) and 49 hips received a G2 stem (Depuy Orthopaedics, Warsaw, IN, USA). A cementless Vision2000 stem (Depuy Orthopaedics, Warsaw, IN, USA) was used in 2 hips, and a MUTARS proximal femoral replacement (Implantcast GmbH, Buxtehude, Germany) was implanted in 1 hip.
Either a modified Watson-Jones approach (12 hips) or a transgluteal Bauer approach (109 hips) was used with the patient in the supine position. At our institution postoperative routine clinical and radiographic follow-up is recommended for hip arthroplasty patients at 1, 3, 5 years and every 5 years thereafter. The collected data is transferred and saved in our institutional joint replacement registry. Every patient of this patient cohort who had not yet completed the clinical and radiological minimum 20-year follow-up at our institution was invited for a routine examination in the setting of this study. For radiographic evaluation, standard anteroposterior (AP) pelvic radiographs and lateral radiographs of the hip were taken. Acetabular inclination was measured using the trans-ischial line as reference. The prevalence, location, and extent of radiolucent gaps or osteolysis at the acetabular bone–prosthesis interface were recorded at the last follow-up using the 3 zones described by DeLee and Charnley (8). Osteolysis was defined as a lucent zone devoid of trabecular bone and usually with a sclerotic border not visible on the immediate postoperative radiograph (9). The acetabular component was considered to be loose if there was migration of > 3 mm horizontally or vertically over time or a circumferential radiolucent line. Heterotopic ossification was graded according to Brooker et al. (10).
Statistics
Descriptive statistics are presented as numbers of occurrence, percentage or arithmetic mean, and standard deviation (SD). We used Kaplan–Meier (K–M) survivorship analysis to determine survival rates for different endpoints. Differences in survival rates between groups of patients were tested for statistical significance using the 2-sided log-rank (Mantel–Cox) test. Hazard ratios for the risk of revision with 95% confidence intervals (CIs) were calculated using the Mantel–Haenszel method. The assumption of proportional hazards was investigated by calculating the estimated hazard rate over time using a Epanechnikov kernel-smoothed hazard function. The plots were inspected visually, and we found that the rates were almost equally distributed over time in both groups. A Kolmogorov–Smirnov test was performed after exploratory data analysis, testing the variables for normal distribution. As not all variables met the criteria for a normal distribution, the Wilcoxon and Mann–Whitney U-test were used. The level of significance was set at P < 0.05 for all statistical tests and the statistical analyses were performed using SPSS (version 27.0; IBM, Armonk, NY, USA) and GraphPad Prism 9 (GraphPad Prism; GraphPad Software, San Diego, CA, USA).
Ethics, data sharing, funding, and disclosures
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the University of Heidelberg, Germany (S-191/2021). Informed consent was obtained from all subjects involved in the study. The data presented in this study is available on request from the corresponding author. The data is not publicly available due to patients’ data protection. This research received no external funding. The authors declare no conflict of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, DOI: 10.2340/17453674.2023.13385
Results
Cohort
The median age at index surgery was 52 (range 21–60) years with 71 (61%) patients under 55 years. There were 73 male (74 hips, 61%) patients. At latest follow-up at a minimum of 20 years (mean 21.4; range 20.2–22.8), 20 (17%) patients with 21 hips (17%) had died. According to phone inquiries and oral statements from the patients’ relatives, it has been determined that all deaths were unrelated to the total hip replacement (THR) procedure, and no revision surgeries have been conducted. A total of 5 (4.3%) patients with 5 hips (4.1%) were lost to follow-up. 4 (3.4%) patients with 4 hips (3.3%) underwent acetabular revision with removal of the cup, and the remaining 91 hips (90 patients) were available for the latest follow-up at a minimum of 20 years after index surgery. 7 of these 91 hips had had no revision surgery or any other complications with the THR but refused to participate in the latest follow-up and withdrew their informed consent. They approved that this information could be used for the study and are listed as dropouts. Another 17 of the 91 available hips had no radiographic follow-up at 20 years or more, as they had either had a radiograph taken less than 5 years previously or they had refused to come to our institution (Figure 2).
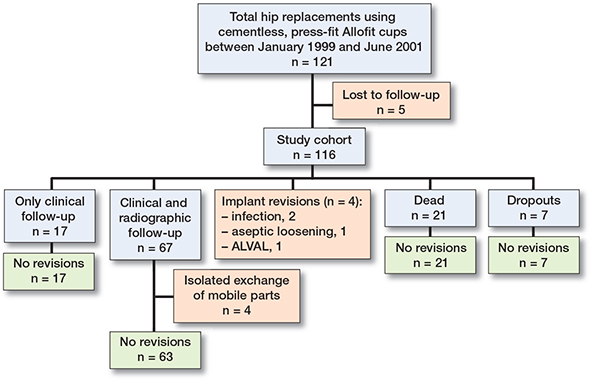
Figure 2. Patient flowchart at latest follow-up at a minimum of 20 years after index surgery. Patients and hips that were lost to follow-up were excluded from the Kaplan–Meier survival analysis.
Revisions
4 (3.3%) acetabular components had to be removed during revision surgery, 2 (1.7%) due to periprosthetic joint infection at 4 and 6 years after index surgery, 1 (0.8%) due to aseptic loosening of the cup at 3 years after index surgery and 1 (0.8%) due to pain that was associated with an aseptic lymphocyte-dominant vasculitis-associated lesion (ALVAL) at 21 years after index surgery.
In addition to the above-mentioned implant revisions, 4 (3.3%) THRs (4 patients) underwent isolated revision of the modular components (liner and femoral head exchange) with retention of the well-fixed cup and stem, 3 THRs with a metal-on-metal (MoM) articulation because of pathologically elevated metal ion levels in the blood at 14, 15, and 16 years after index surgery, and 1 THR with a ceramic-on-polyethylene bearing (CoP) because of significant polyethylene wear at 17 years after index surgery. There were no isolated stem revisions.
Survival
The K–M survival analysis, using acetabular revision for any reason as endpoint, estimated the 22-year survival rate at 92% (CI 86–96; 18 hips at risk) (Figure 3). The K–M survival analysis, using acetabular revision for any aseptic reason as endpoint, estimated the 22-year survival rate at 94% (CI 87–96; 20 hips at risk) (Figure 4). The K–M survival rate after 22 years with acetabular revision for aseptic loosening (without isolated revision of modular components) as endpoint was estimated at 99% (CI 94–100; 21 hips at risk) (Figure 5).
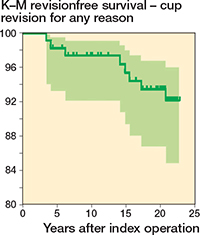
Figure 3. K–M survivorship and CI with acetabular revision, including isolated exchange of modular components (liner and femoral head), for any reason as endpoint. 22-year survival 92% (CI 84.5–96; initially: 116; revised: 8; censored due to death: 21; at risk at 22 years: 18).
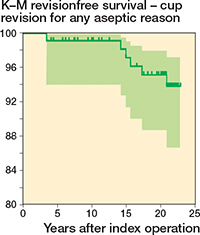
Figure 4. K–M survivorship and CI with acetabular revision, including isolated exchange of modular components (liner and femoral head), for any aseptic reason as endpoint. 22-year survival 94% (CI 87–96; initially: 116; revised: 6; censored due to death: 21, at risk at 22 years: 20).
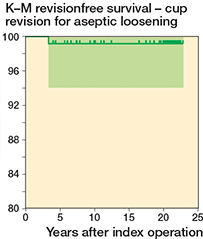
Figure 5. K–M survivorship and CI with acetabular revision for aseptic loosening as endpoint. 22-year survival 99% (CI 94–100; initially: 116; revised: 1; censored due to death: 21, at risk at 22 years: 21).
Patients aged 50 years or younger at index surgery (n = 45) had an implant survival rate of 97% (CI 89–98) after 22 years and did not have a higher revision risk than patients aged over 50 years (n = 76) (log-rank test, P = 0.3) (Figure 6).
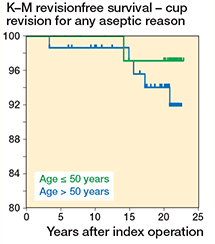
Figure 6. Comparison of K–M survivorship curves with acetabular revision for any aseptic reason as endpoint for patients aged ≤ 50 at the time of surgery (n = 45) vs. patients aged > 50 (n = 76) (log-rank test, P = 0.3).
The survival rate with acetabular revision for any aseptic reason as endpoint was similar between hips with MoM (n = 86) articulations and CoP (n = 34) bearings (log-rank test, P = 0.5) (Figure 7).
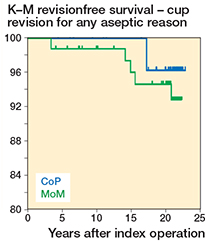
Figure 7. Comparison of K–M survivorship curves with acetabular revision for any reason as endpoint for hips with 28-mm (Metasul) MoM articulation (n = 86) vs. ceramic-on-conventional polyethylene (CoP) articulation (n = 34) (log-rank test, P = 0.5).
Radiographic evaluation
Radiographs with a minimum of 20 years after index surgery were available for a total of 67 (74%) of the remaining THRs. None of them showed radiographic evidence of cup loosening.
Asymptomatic but significant osteolytic lesions were found in 20 out of 50 THRs with an MoM articulation (Figure 8), and in 13 out of 17 THRs with a conventional (not-highly crosslinked) liner and CoP bearing. Furthermore, 15 out of 17 of the THRs with a CoP bearing also showed asymptomatic but a significant polyethylene wear with decentration of the femoral head on the anteroposterior (AP) pelvic radiograph (Figure 9).

Figure 8. Example of an osteolytic lesion on a lateral radiograph of the right hip showing a cementless stem (CLS) and the cementless press-fit Allofit cup with a 28mm (Metasul) metal-on-metal (MoM) articulation.

Figure 9. Example of a cementless THR (CLS stem and Allofit cup) with a ceramic-on-not highly crosslinked polyethylene bearing (CoP). Note the high cup inclination and significant polyethylene wear leading to decentration of the femoral head and significant osteolytic lesions in Gruen zones 1 and 7.
Of the 67 THRs at final follow-up the median inclination angle of the acetabular cup was 44° (range 27–62). An inclination angle outside Lewinnek’s “safe zone” (cup inclination of 40° ± 10°) was found in 15 hips.
Clinical evaluation
For better comparison with other studies, the WOMAC score (11) was converted to a 100-point scale, 0 being poor and 100 being the best possible outcome. The mean WOMAC score was 85 (SD 17) at our latest follow-up at a minimum of 20 years after index surgery and was available for a total of 84 (92%) of the remaining THRs.
To assess the pain level of the hip, the VAS score (12), with 0 being no pain and 10 being the worst pain imaginable, was collected at our latest follow-up. The mean VAS was 1.1 (SD 1.7) at a minimum of 20 years after index surgery and was available for a total of 84 (92%) of the remaining THRs.
Discussion
At present, cementless primary THR is most commonly performed using a modular, press-fit acetabular component (3,13). Nevertheless, there are only a few studies reporting on the minimum 20-year outcome of cementless acetabular cups (Table 2) and, to the best of our knowledge, there is no study reporting on the minimum 20-year results of a cementless cup that is still in clinical use today. Despite the frequent implantation of the Allofit acetabular component in primary THR for over 20 years, there are still only very few reports on mid- to long-term outcome for this specific type (14). In our previous report on this patient cohort, we had found a 97.5% survivorship at 11 years’ follow-up with acetabular revision for any reason as endpoint (7). This finding is consistent with data from the recent annual report of the Swedish Hip Arthroplasty Register, where an implant survival of 98.8% at 10 years was found for the Allofit cup (15). The strength of the present study is not only the long-term follow-up with a mean of 21.4 years (range 20.2–22.8) and the low rate of patients lost to follow-up (4.1%), but also the availability and analysis of the individual radiological results and hip function. The survivorship with any acetabular revision (including isolated exchange of modular components), for any aseptic reason as endpoint was 94% at 22 years with an acetabular cup survival of 99% at 22 years using cup revision for aseptic loosening as the endpoint. It is interesting to note in this context that the cumulative acetabular survival in patients younger than 50 years of age at the time of index surgery was not inferior to survival in patients older than 50 years. However, this could be attributed to the inclusion of a limited number of patients, leading to a potential issue with statistical power. The remarkably low rate of aseptic loosening of 1% at 22 years’ follow-up confirms that cementless, press-fit acetabular fixation using the Allofit cup was extremely durable despite young patient age at surgery and significant wear-related osteolysis. Primary stability can be sufficiently achieved by the press-fit effect without supplemental screw fixation in young patients with good bone quality.
| A | B | C | D | E | F | G | H | I | J | K |
| Schmolders et al. (22) | 2016 | Threaded cup (Bicon SL) | CoP | 111 | 13.5 | 48 | 96.8 at 10 years | 96.8 at 10 years | 11 | – |
| Moon et al. (23) | 2018 | Press-fit cup X (Bicon SL) | MoM | 114 | 20 | 46 | 90 at 23 years | 91 at 23 years | 11 | – |
| Kim et al. (24) | 2019 | Press-fit cup (Duraloc/Pinnacle) | CoC | 324 | 15.6 | 46 | 99 at 15 years | 100 at 15 years | 0 | 0 |
| Erivan et al. (25) | 2019 | Press-fit cup (CLS Spotorno) | MoM | 115 | 20.3 | 57 | 86.1 at 18 years | 92.6 at 18 years | – | – |
| Pisecky et al. (26) | 2020 | Threaded cup (Alloclassic CSF) | CoP | 75 | 29.5 | 53 | 70.6 at 29 years | 97.3 at 29 years | 11 | 15 |
| Jin et al. (27) | 2021 | Press-fit cup (Fitmore) | MoM | 84 | 18.6 | 39 | 93.1 at 18 years | – | 8 | – |
| Mosconi et al. (28) | 2021 | Press-fit cup (TOP) | CoP | 524 | 12 | 66 | 90.5 at 12 years | 92 at 12 years | 10 | 3 |
| Current study | 2022 | Press-fit cup (Allofit) | MoM/CoP | 121 | 21 | 51 | 92 at 22 years | 99 at 22 years | 20 | 88 a |
| A = study. B = year. C = cup. D = articulation with bearing surfaces. E = no. of hips. F = mean follow-up (years). G = mean age at index surgery (years). H = survivorship, all cup revisions (incl. isolated exchange of mobile components) (%). I = survivorship, aseptic cup loosening (%). J = periacetabular osteolysis (%). K = polyethylene wear with decentration of femoral head (%). a of the CoP articulations |
||||||||||
At the time of index surgery of this patient cohort the use of second-generation 28-mm (small femoral head diameter) MoM articulations or the use of conventional (not-highly crosslinked) polyethylene liners were considered to be best clinical practice. However, a major change of paradigm has occurred since, as elevated metal ion blood levels, pseudotumors, and ALVAL were identified to be related to MoM articulations, especially with large femoral head diameters (16-18). These particular problems usually do not occur during the first decade after index surgery. In line with this, no revisions related to the bearings had occurred in our patient cohort during the first 10 years, but during the second decade 4 patients underwent isolated revision of the modular components (liner and femoral head exchange) due to elevated metal ion blood levels, and 1 patient underwent revision of the Allofit cup due to ALVAL. And while radiographic follow-up at 10 years did not show any pathologies related to the bearings used, radiographic follow-up at 20 and more years revealed asymptomatic but significant osteolysis in about 40% of THRs with a MoM articulation and in about 77% of THRs with a CoP articulation. Furthermore, our latest radiological follow-up confirms and highlights the well-known problem of increased wear rates of conventional polyethylene liners as it showed significant polyethylene wear with decentration of the femoral head in around 88% of THRs with a conventional polyethylene liner. The comparison of K–M survivorship curves with acetabular revision for any reason as endpoint between the second-generation 28-mm (Metasul) MoM articulations and conventional (not-highly crosslinked) polyethylene liners with CoP articulations did not show a statistically significant difference (log-rank test, P = 0.5).
The excellent revision and survival rates of our patient cohort reported here are at risk of being compromised in the next 5 to 10 years due to progressive osteolysis and polyethylene wear, potentially resulting in implant loosening or periprosthetic fractures. Almost every second patient was identified to have asymptomatic osteolysis and almost 9 out of 10 THRs had radiological signs of significant polyethylene wear. These worrisome numbers are expected to further rise in the third decade. Based on our findings we recommend routine follow-up examinations of THRs with MoM articulations or conventional, not-highly crosslinked, polyethylene liners, especially in the second and third decade after index surgery to detect potential hazards in time and thereby avoid complications. Our findings complement the robust data of national arthroplasty registries and can help orthopedic surgeons to choose the most reliable implant model, fixation method, and bearing surface to achieve the lowest possible revision rates. This seems particularly important in the context that indications for THR have expanded to ever younger patients who expect a durability of implants into the third or even fourth decade after index surgery (19).
There are several limitations to our study design. Although data was collected prospectively, the design of our study remains retrospective with its inherent limitations. The incidence of osteolysis, pseudotumors, and polyethylene wear might be underestimated, as evaluation was based on conventional radiographs (compared with evaluation based on computed tomography or magnetic resonance imaging) and 26% of the THRs had no radiographic follow-up at latest follow-up (20). The low lost to follow-up rate of 4% (5 THRs) despite a minimum follow-up of 20 years underlines the reliability of our survival rates. We assumed that all patients who were dead at the latest follow-up (21 hips; 17%), had died from unrelated reasons. This assumption was made on statements given by the patientsʼ families. However, some uncertainty remains. Furthermore, death for any reason is a competing risk for revision surgery. In our study, the median age at final follow-up was 75 years. Therefore, a number of deaths from natural causes was expected. More than 80% of patients from the original cohort were alive at our latest follow-up. Thus, we believe that a competing risk analysis would not be superior compared with the K–M survivorship analysis that was conducted. At future follow-ups a competing risk analysis might be a valuable complement. Finally, the study may have been underpowered, due to our cohort size, to show a difference in survival rates between articulation groups or age groups. Likewise, the exploratory element of this study is limited by the small number of revision procedures and therefore a multivariable analysis or Cox model was not conducted.
In conclusion, we have conducted a follow-up of the first 121 cementless, press-fit Allofit cups and determined the radiographic results and cumulative survival rates at a minimum of 20 years after index surgery. The press-fit cup stays very reliable into the third decade with a 22-year Kaplan–Meier revision-free survival of 92%, 94%, and 99% for the endpoints any revision, any aseptic revision, and revisions for aseptic loosening, respectively. However, we have identified very high rates of osteolytic lesions and extensive polyethylene wear at our latest follow-up. These radiological findings can be directly traced to implantation of MoM articulations and not-highly crosslinked liners. Therefore, it is very important to differentiate between the excellent cup survival rate and the high rate of problematic radiological findings resulting from the outdated bearing surfaces used in this patient cohort. Today, there are excellent alternative bearing options such as highly crosslinked polyethylene liners or ceramic-on-ceramic articulations. In accordance with the recommendations of the UK National Institute for Health and Care Excellence (NICE) dating back to 2017 (21), we strongly advise patients with older bearing surfaces (especially MoM articulations) to undergo regular follow-ups every 3 years. These follow-ups should include plain radiographs, ultrasound screening of the hip, and analysis of metal ion levels in the blood. This proactive approach aims to prevent serious complications that could potentially lead to implant failure.
- Ben-Shlomo Y, Blom A, Boulton C, Brittain R, Clark E, Dawson-Bowling S, et al. National Joint Registry Annual Reports. Available from https://www.ncbi.nlm.nih.gov/books/NBK587525/.
- Kärrholm J, Rogmark C, Naucler E, Nåtman J, Vinblad J, Mohaddes M, et al. Swedish Hip Arthroplasty Register Annual report 2019; 2021. doi: 10.18158/H1BdmrOWu.
- Grimberg A, Jansson V, Lützner J, Melsheimer O, Morlock M, Steinbrück A. EPRD Jahresbericht 2021; 2021.
- Kurtz S M, Gawel H A, Patel J D. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res 2011; 469: 2262-77. doi: 10.1007/s11999-011-1872-4.
- Moon N H, Shin W C, Do M U, Kang S W, Lee S M, Suh K T. Wear and osteolysis outcomes for highly cross-linked polyethylene in primary total hip arthroplasty compared with conventional polyethylene: a 15- to 18-year single-centre follow-up study. Hip Int 2021; 31: 526-32. doi: 10.1177/1120700019896970.
- Schreurs B W, Hannink G. Total joint arthroplasty in younger patients: heading for trouble? Lancet 2017; 389: 1374-5. doi: 10.1016/s0140-6736(17)30190-3.
- Streit M R, Weiss S, Andreas F, Bruckner T, Walker T, Kretzer J P, et al. 10-year results of the uncemented Allofit press-fit cup in young patients. Acta Orthop 2014; 85: 368-74. doi: 10.3109/17453674.2014.925351.
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 1976; (121): 20-32.
- Kim Y H, Kim J S, Park J W, Joo J H. Periacetabular osteolysis is the problem in contemporary total hip arthroplasty in young patients. J Arthroplasty 2012; 27: 74-81. doi: 10.1016/j.arth.2011.03.022.
- Brooker A F, Bowerman J W, Robinson R A, Riley L H, Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am 1973; 55: 1629-32.
- Bellamy N, Buchanan W W, Goldsmith C H, Campbell J, Stitt L W. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988: 15: 1833-40.
- Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs 2005; 14: 798-804. doi: 10.1111/j.1365-2702.2005.01121.x.
- Ben-Shlomo Y, Blom A, Boulton C, Brittain R, Clark E, Dawson-Bowling S, et al. National Joint Registry Annual Reports. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576858/.
- Zenz P, Stiehl J B, Knechtel H, Titzer-Hochmaier G, Schwagerl W. Ten-year follow-up of the non-porous Allofit cementless acetabular component. J Bone Joint Surg Br 2009; 91: 1443-7. doi: 10.1302/0301-620x.91b11.22368.
- Robertsson O, Lidgren L, Sundberg M, W-Dahl A. The Swedish Knee Arthroplasty Register—Annual report 2019; 2020. Available from: https://www.myknee.se/en/.
- Hannemann F, Hartmann A, Schmitt J, Lützner J, Seidler A, Campbell P, et al. European multidisciplinary consensus statement on the use and monitoring of metal-on-metal bearings for total hip replacement and hip resurfacing. Orthop Traumatol Surg Res 2013; 99: 263-71. doi: 10.1016/j.otsr.2013.01.005.
- Kwon Y M, Lombardi A V, Jacobs J J, Fehring T K, Lewis C G, Cabanela M E. Risk stratification algorithm for management of patients with metal-on-metal hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, and the Hip Society. J Bone Joint Surg Am 2014; 96: e4. doi: 10.2106/jbjs.M.00160.
- Hopper R H Jr, Ho H, Sritulanondha S, Williams A C, Engh C A Jr. Otto Aufranc Award: Crosslinking reduces THA wear, osteolysis, and revision rates at 15-year followup compared with noncrosslinked polyethylene. Clin Orthop Relat Res 2018; 476: 279-90. doi: 10.1007/s11999.0000000000000036.
- Kurtz S M, Lau E, Ong K, Zhao K, Kelly M, Bozic K J. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009; 467: 2606-12. doi: 10.1007/s11999-009-0834-6.
- Walde T A, Weiland D E, Leung S B, Kitamura N, Sychterz C J, Engh C A Jr, et al. Comparison of CT, MRI, and radiographs in assessing pelvic osteolysis: a cadaveric study. Clin Orthop Relat Res 2005; (437): 138-44. doi: 10.1097/01.blo.0000164028.14504.46.
- (MHRA), M.a.H.p.R.A. Medical Device Alert. All metal-on-metal (MoM) hip replacements: updated advice for follow-up of patients. (NICE), N.I.f.H.a.C.E., editor; 2017.
- Schmolders J, Amvrazis G, Pennekamp P H, Strauss A C, Friedrich M J, Wimmer M D, et al. Thirteen year follow-up of a cementless femoral stem and a threaded acetabular cup in patients younger than fifty years of age. Int Orthop 2017; 41: 39-45. doi: 10.1007/s00264-016-3226-z.
- Moon J K, Kim Y, Hwang K T, Yang J H, Oh Y H, Kim Y H. Long-term outcomes after metal-on-metal total hip arthroplasty with a 28-mm head: a 17- to 23-year follow-up study of a previous report. J Arthroplasty 2018; 33: 2165-72. doi: 10.1016/j.arth.2018.02.089.
- Kim Y H, Park J W. Long-term outcomes of ultra-short metaphyseal-fitting anatomic cementless femoral stem in total hip arthroplasty with ceramic-on-ceramic articulation for young patients. J Arthroplasty 2019; 34: 2427-33. doi: 10.1016/j.arth.2019.04.036.
- Erivan R, Villatte G, Lecointe T, Mulliez A, Descamps S, Boisgard S. Long-term survival of hybrid total hip arthroplasty with the uncemented CLS cup, cemented Müller cobalt-chromium stem, and 28-mm Metasul™ bearings: retrospective review of 115 hips after a minimum of 17.8 years. Orthop Traumatol Surg Res 2019; 105: 1289-95, doi: 10.1016/j.otsr.2019.06.019.
- Pisecky L, Allerstorfer J, Schauer B, Hipmair G, Hochgatterer R, Böhler N, et al. Straight stem and threaded cup in patients under 60 years of age: 28.8–30.2 years of follow-up. J Orthop Surg Res 2020; 15: 563. doi: 10.1186/s13018-020-02102-w.
- Jin S Y, Jin J Y, Kang J K, Yoon T R, Park K S. Minimum 15-year results of metasul 28-mm metal-on-metal total hip arthroplasty in patients younger than 50 years of age. J Orthop Surg Res 2021; 16: 218. doi: 10.1186/s13018-021-02352-2.
- Mosconi L, Cavagnaro L, Zanirato A, Quarto E, Lontaro Baracchini M, Formica M. Long-term follow-up of a low profile, coated, pressfit cup: the trabeculae oriented pattern (T.O.P.) acetabular system. Eur J Orthop Surg Traumatol 2021; 31: 1515-21. doi: 10.1007/s00590-021-02917-1.