Does choice of bearings influence the survival of cementless total hip arthroplasty in patients aged 20–55 years? Comparison of 21,594 patients reported to the Nordic Arthroplasty Register Association dataset 2005–2017
Rasmus Tyrsted MIKKELSEN 1,2, Søren OVERGAARD 3-5, Alma B PEDERSEN 6, Johan KÄRRHOLM 7,8, Ola ROLFSON 7,8, Anne Marie FENSTAD 9, Ove FURNES 9,10, Geir HALLAN 9,10, Keijo MÄKELÄ 11,12, Antti ESKELINEN 12,13, and Claus VARNUM 1,2,5,14
1 Department of Orthopedic Surgery, Lillebaelt Hospital—Vejle, University Hospital of Southern Denmark, Denmark; 2 Department of Regional Health Research, Faculty of Health Science, University of Southern Denmark, Odense, Denmark; 3 Department of Orthopedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg, Denmark; 4 Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark; 5 The Danish Hip Arthroplasty Register, Århus, Denmark; 6 Department of Clinical Epidemiology, Aarhus University Hospital and Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 7 Department of Orthopedics, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 8 The Swedish Arthroplasty Register, Gothenburg, Sweden; 9 The Norwegian Arthroplasty Register, Department of Orthopedic Surgery, Haukeland University Hospital, Bergen, Norway; 10 Department of Clinical Medicine, University of Bergen, Bergen, Norway; 11 Department of Orthopedics and Traumatology, Turku University Hospital, Turku, and University of Turku, Finland; 12 The Finnish Arthroplasty Registry, Helsinki, Finland; 13 Coxa Hospital for Joint Replacement, and Faculty of Medicine and Health Technologies, University of Tampere, Tampere, Finland; 14 Department of Orthopaedic Surgery and Traumatology, Odense University Hospital, Odense, Denmark
Background and purpose — The bearings with the best survivorship for young patients with total hip arthroplasty (THA) should be identified. We compared hazard ratios (HR) of revision of primary stemmed cementless THAs with metal-on-metal (MoM), ceramic-on-ceramic (CoC), and ceramic-on-highly-crosslinked-polyethylene (CoXLP) with that of metal-on-highly-crosslinked-polyethylene (MoXLP) bearings in patients aged 20–55 years with primary osteoarthritis or childhood hip disorders.
Patients and methods — From the Nordic Arthroplasty Register Association dataset we included 1,813 MoM, 3,615 CoC, 5,947 CoXLP, and 10,219 MoXLP THA in patients operated on between 2005 and 2017 in a prospective cohort study. We used the Kaplan–Meier estimator for THA survivorship and Cox regression to estimate HR of revision adjusted for confounders (including 95% confidence intervals [CI]). MoXLP was used as reference. HRs were calculated during 3 intervals (0–2, 2–7, and 7–13 years) to meet the assumption of proportional hazards.
Results — Median follow-up was 5 years for MoXLP, 10 years for MoM, 6 years for CoC, and 4 years for CoXLP. 13-year Kaplan–Meier survival estimates were 95% (CI 94–95) for MoXLP, 82% (CI 80–84) for MoM, 93% (CI 92–95) for CoC, and 93% (CI 92–94) for CoXLP bearings. MoM had higher 2–7 and 7–13 years’ adjusted HRs of revision (3.6, CI 2.3–5.7 and 4.1, CI 1.7–10). MoXLP, CoC, and CoXLP had similar HRs in all 3 periods. The 7–13-year adjusted HRs of revision of CoC and CoXLP were statistically non-significantly higher.
Conclusion — In young patients, MoXLP for primary cementless THA had higher revision-free survival and lower HR for revision than MoM bearings. Longer follow-up is needed to compare MoXLP, CoC, and CoXLP.
Citation: Acta Orthopaedica 2023; 94: 266–273. DOI: https://doi.org/10.2340/17453674.2023.13384.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-10-11. Accepted: 2023-03-28. Published: 2023-06-05.
Correspondence: Rasmus.tyrsted.mikkelsen@rsyd.dk
All authors designed the study. RM analyzed the data and wrote the initial draft of the manuscript. All authors discussed the results, revised the draft, and accepted the final version of the manuscript.
Handling co-editors: Bart Swierstra and Robin Christensen
Acta thanks Peter Lewis and Willem B Schreurs help with peer review of this study.
Young patients under age 55 have a higher revision risk of their total hip arthroplasty (THA) than older patients 10 years after surgery (1-3). This is problematic, as younger patients risk undergoing multiple revisions and revision surgery may be associated with poor clinical outcome (4). Therefore, the implants with the best survival and lowest risk of revision should be identified.
A frequent long-term revision cause of THA is aseptic loosening (1-3), which may result from wear debris causing an inflammatory response (5). To reduce wear-related complications, metal-on-metal (MoM), ceramic-on-ceramic (CoC), and ceramic-on-highly-crosslinked-polyethylene (CoXLP) have been used in especially young active patients (6,7).
MoM THA has since shown inferior survivorship compared with all other combinations of THA bearings (1,2,8). Most countries have stopped using MoM THA and implemented follow-up programs for patients as long as they have a MoM THA (9).
It is still debated whether CoC, CoXLP, or metal-on-highly-crosslinked-polyethylene (MoXLP) is the optimal bearing for young patients (6). CoC and CoXLP bearings are increasingly used for young patients (6,10) although their superiority remains unclear (1,3,11,12). CoC and MoXLP THA have shown similar survival up to 9 years after surgery (13). However, only a few population-based follow-up studies have been conducted on the survival and risk of revision of primary stemmed (not resurfacing) cementless (uncemented stem and cup) THA with these bearings beyond 10 years in young patients (11,12).
We compared the survival and hazard ratio (HR) of revision of primary stemmed cementless THA with MoM, CoC, and CoXLP with that of MoXLP bearings in patients aged 20–55 years diagnosed with osteoarthritis or childhood hip disorders.
Patients and methods
We conducted a population-based cohort study with prospectively collected data from each of the registries in the Nordic Arthroplasty Register Association (NARA) including data from Denmark, Norway, Sweden, and Finland. These 4 countries have a combined population of approximately 27 million citizens and similar tax-supported public healthcare systems (14).
Data source
In May 2020, the NARA dataset had registered information on 848,787 THAs since 1995 (15). Data originates from all THAs performed in the 4 countries. Registration completeness ranges from 90–98% for primary surgery and 81–94% for revision surgery when compared with the national patient registers in the respective countries. Data is frequently validated within the national registers, ensuring high data quality (16).
Study population
We included all patients aged 20–55 years who received stemmed cementless THA because of primary osteoarthritis (OA) or childhood hip disorders. They had MoM, CoC, CoXLP, or MoXLP bearings, were operated on from January 1, 2005 to December 31, 2017 and had a minimum of 1-year follow-up until end of study (December 31, 2018). We chose 2005 because the 4th generation of ceramic was introduced in 2004 according to the manufacturer (CeramTec, Plochingen, Germany) and because this type of ceramic material is not captured in the NARA dataset, we had no other way of adjusting for generation of ceramic.
Childhood hip disorders cover hip dysplasia, slipped capital femoral epiphysis or Perthes disease. Previous studies with this definition of childhood hip disorders have shown survival of THA similar to that for OA despite surgery often being more complex (17), while other diagnoses such as femoral neck fracture and rheumatoid arthritis have inferior THA survival (1).
We excluded THAs with dual mobility cups. Cup and stem implants used in fewer than 50 cases for each country were also excluded as they may have been subjected to a learning curve. THAs with missing data for any of the variables studied were excluded, except revised THAs with missing revision cause. These patients were still included in the analyses of HR of revision for any cause. THAs with femoral heads smaller than 28 mm were excluded as only 50 cases were found. In patients with bilateral THA only the first operation was included to make observations independent. After these exclusions 21,594 patients remained (Figure 1).
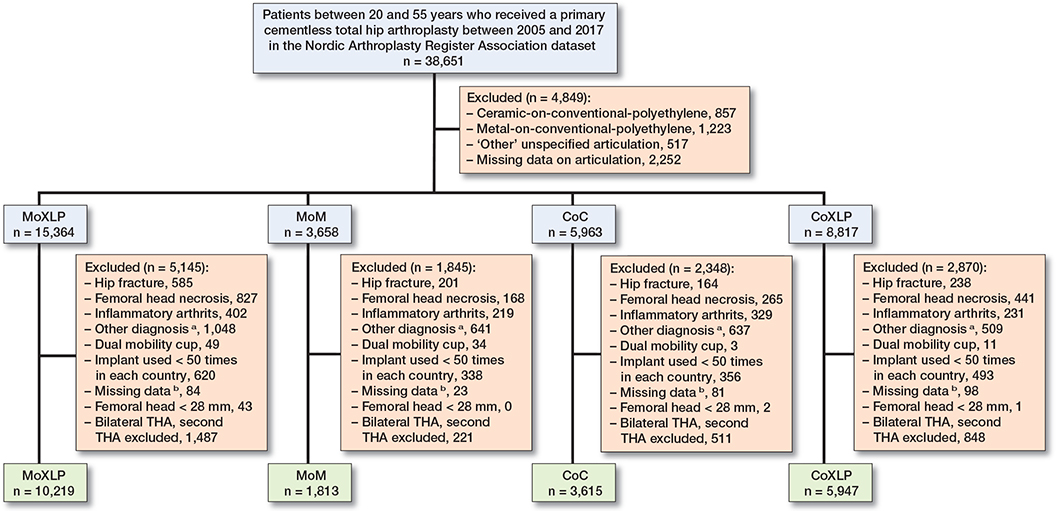
Figure 1. Flowchart of patient exclusion from the cohort. a Other diagnoses than primary osteoarthritis, childhood hip disorders, hip fracture, femoral head necrosis, and inflammatory arthritis. b Missing information on fixation, diagnosis, cup, stem or femoral head size.
Statistics
We calculated survival and HR of revision for any reason and specific causes. In the dataset revision causes are categorized as aseptic loosening, prosthetic joint infection, periprosthetic fracture, dislocation, pain only and ‘other’. ‘Other’ being reasons not covered by the beforementioned categories. Revision was defined as any surgical intervention with partial or complete exchange or removal of the THA components. Patients were censored at the time of revision surgery, death or end of study.
For demographic characteristics we used descriptive statistics. Age and follow-up were given in medians with interquartile range (IQR) due to skewness. We used the Kaplan–Meier estimator for survival function. Cox regression was used to calculate HR for revision. Adjustments were made for possible confounders (1,2): sex, age, diagnosis, year of primary surgery, and femoral head size in the Cox regression for revision due to any cause. The strata of these variables in the analyses are equal to those in Table 1. In our Cox regression we allowed no more than 1 degree of freedom of the covariates for every 10 events to prevent the model from being overfitted. We could therefore only perform revision cause-specific Cox regression for revision caused by “others” as too few events occurred in each period due to the remaining revision causes (Table 2). Cox regression for revision caused by “others” was adjusted for sex, diagnosis, year of primary surgery, and size of femoral head.
Sensitivity analyses were performed to study effect modification for sex (adjusted for diagnosis and year of primary surgery), OA (sex, age, year of primary surgery, and femoral head size) and the 5 most common combinations of brand-specific cup and stem with CoC articulation with all 28 mm head CoC THAs excluded (adjusted for sex and diagnosis). The latter analysis was performed as ‘other’ was the most common revision cause for CoC, which could cover head and liner fracture, a revision cause that is not specified in the NARA dataset. All MoXLP THAs served as reference. We excluded 28 mm head CoC THAs as this head size constitutes the major difference in risk of fracture between 3rd and 4th generation ceramic (18). We did not perform this analysis for CoXLP as we found no clear difference in revision causes between MoXLP and CoXLP.
For missing information on bearings, we performed 4 worst-case scenarios where all patients with missing information concerning bearings were included in either the MoXLP, MoM, CoC, or CoXLP groups.
MoXLP was the most frequently used bearing (Table 1), therefore considered as the standard bearing and used as reference in all analyses. We tested the assumption of proportional hazards by log–log plots and Schoenfeld residuals. To meet the assumption of proportional hazards we split the analyses into 3 periods: 0–2, 2–7 years, and 7–13 years. 95% confidence intervals (CI) were given and a p-value below 0.05 was considered statistically significant. The statistical analyses were performed in STATA version 16.1 (STATACorp, College Station, TX, USA).
This paper is written according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and the Reporting of studies Conducted using Observational Routinely-collected Data (RECORD) guidelines.
Ethics, funding, and disclosures
This study was approved by the Record of Data Processing Activities in the Region of Southern Denmark, journal number 19/48212. The ethical approval for the NARA dataset was approved by the appointed authorities in each country: the Swedish Ethical Review Authority (Dnr: 1184-18/2019-00812), the Finnish National Institute of Health and Welfare (Dnro THL/1743/5.05.00/2014), the Norwegian Data Inspectorate (ref 24.1.2017: 16/01622-3/CDG and Ethical approval 2015/880/REK Vest), and the Danish Data protection agency (1-16-02-54-17). We acknowledge support from the Region of Southern Denmark (grant number 20/14821), which had no role in the study design, data collection and analysis, or in the preparation of the manuscript. The authors of this study have no conflicts of interest related to this study. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.13384
Results
Description of study population
47% of patients had MoXLP, 8% had MoM, 17% had CoC, and 28% had CoXLP bearings. Median age was similar but median follow-up was longer in MoM and CoC (Table 1). More men had MoM THA than women. The distribution of patient characteristics between the bearing groups was similar in the 0–2, 2–7, and 7–13 years intervals except size of femoral head. The majority of MoM and CoC bearings were used in 1 country. 28 mm femoral heads were more prevalent in the 7–13 years interval than the other intervals, but equally more prevalent in MoXLP and CoC.
Survival and hazard rate of revision
13 years postoperatively the survival was 95% (CI 94–95) for MoXLP, 82% (CI 80–84) for MoM, 93% (CI 92–95) for CoC, and 93% (CI 92–94) for CoXLP bearings (Figure 2).
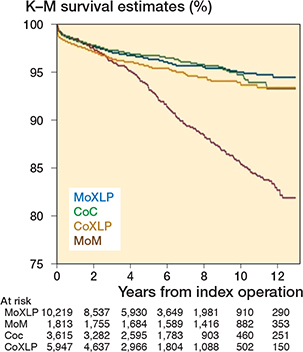
Figure 2. Survival probability with any revision as endpoint. Note that the y-axis interval is 0.75 to 1.
In the study period 1,012 revisions were performed. The most common revision cause was “other,” meaning unspecified reasons followed by prosthetic joint infection (Table 2). 17 patients had missing revision cause.
MoM had similar adjusted HR of revision for any cause to MoXLP during the first period (0–2 years) but had significantly higher HR during the 2 later periods (adjusted HR for revision of any cause 2–7 years: 3.9 [CI 3.0–4.9], 7–13 years: 3.6 [CI 2.3–5.7]). CoC and CoXLP had similar adjusted HR for any cause to MoXLP in all 3 periods. However, the 7–13 years adjusted HR of revision for any cause tended to be higher for both CoC and CoXLP compared with MoXLP, although not statistically significant (Table 3).
| Period Bearing | Number at risk | Number of revisions | Unadjusted HR (CI) | Adjusted a HR (CI) |
| 0–2 years | ||||
| MoXLP | 10,219 | 230 | 1 (ref.) | 1 (ref. ) |
| MoM | 1,813 | 45 | 1.1 (0.8–1.5) | 1.3 (0.8–2.4) |
| CoC | 3,615 | 79 | 1.0 (0.7–1.2) | 1.0 (0.8–1.3) |
| CoXLP | 5,947 | 166 | 1.3 (1.0–1.5) | 1.2 (1.0–1.5) |
| 2–7 years | ||||
| MoXLP | 8,538 | 120 | 1 (ref.) | 1 (ref. ) |
| MoM | 1,756 | 141 | 3.9 (3.0–4.9) | 3.6 (2.3–5.7) |
| CoC | 3,284 | 42 | 0.8 (0.6–1.1) | 0.8 (0.6–1.1) |
| CoXLP | 4,640 | 69 | 1.1 (0.8–1.5) | 1.2 (0.9–1.6) |
| 7–13 years | ||||
| MoXLP | 2,726 | 12 | 1 (ref.) | 1 (ref. ) |
| MoM | 1,536 | 79 | 8.0 (4.3–14) | 4.1 (1.7–10) |
| CoC | 1,294 | 16 | 2.7 (1.3–5.7) | 2.1 (1.0–4.5) |
| CoXLP | 1,412 | 13 | 2.0 (0.9–4.3) | 2.1 (1.0–4.6) |
| a Adjusted for sex, age, diagnosis, year of primary surgery, and femoral head size. | ||||
MoM had an increased adjusted HR for revision due to “other” causes during all 3 periods, CoC only during the first 2, and CoXLP in neither of the periods (Table 4).
| Period Bearing | Number at risk | Number of revisions | Unadjusted HR (CI) | Adjusted a HR (CI) |
| 0–2 years | ||||
| MoXLP | 10,219 | 33 | 1 (ref.) | 1 (ref.) |
| MoM | 1,813 | 13 | 2.1 (1.1–4.1) | 3.1 (1.1–9.1) |
| CoC | 3,615 | 30 | 2.5 (1.5–4.1) | 2.3 (1.4–3.8) |
| CoXLP | 5,947 | 17 | 0.9 (0.5–1.6) | 0.9 (0.5–1.6) |
| 2–7 years | ||||
| MoXLP | 8,538 | 21 | 1 (ref.) | 1 (ref.) |
| MoM | 1,756 | 102 | 15 (9.7–25) | 10 (5.0–22) |
| CoC | 3,284 | 20 | 2.2 (1.2–4.0) | 2.0 (1.1–3.7) |
| CoXLP | 4,640 | 14 | 1.3 (0.7–2.6) | 1.4 (0.7–2.7) |
| 7–13 years | ||||
| MoXLP | 2,726 | 5 | 1 (ref.) | 1 (ref.) |
| MoM | 1,536 | 58 | 14 (5.6–35) | 4.9 (1.2–19) |
| CoC | 1,294 | 5 | 2.0 (0.6–8.0) | 1.6 (0.5–5.8) |
| CoXLP | 1,412 | 4 | 1.5 (0.4–5.5) | 1.6 (0.4–6.0) |
| a Adjusted for sex, diagnosis, year of primary surgery, and size of femoral head. | ||||
Sensitivity analyses
For males with MoM THA, the adjusted 7–13-year HR was lower than for both sexes together: 2.2 (CI 0.6–8.5) vs. 4.1 (CI 1.7–10). For males with CoC THA, the adjusted 7–13 years HR was higher than for both sexes together: 3.0 (CI 1.0–9.3) vs. 2.1 (CI 1.0–4.5). Note that these differences had overlapping 95% CIs. No other differences were found when stratifying for sex and OA as diagnosis (Table 3 and Table 6, see Appendix).
The 5 most common combinations of cup and stem in CoC THA without 28 mm heads (55% of all CoC) were Pinnacle/Corail (n = 1,039), R3/Synergy (n = 351), Igloo/Filler (n = 234), Continuum/M/L Taper (n = 262) and Exceed/Bi-metric collarless (n = 105). The sensitivity analysis with these 5 combinations revealed a higher adjusted 7–13-year HR 4.4 (CI 1.6–12) compared with HR for CoC THA for the complete study population and period, HR 2.1 (CI 1.0-4.5) (Table 3 and Table 6, see Appendix).
Analyses of missing data
The 4 worst-case scenarios that all 2,252 excluded patients with missing information on bearings had received either a MoXLP, MoM, CoC, or CoXLP were analyzed. Only the adjusted 7–13-year HR if all missing bearings were CoC or CoXLP was markedly different. If all missing bearings were CoC the adjusted HR for CoC increased from 2.1 CI (1.0–4.5) to 2.5 (CI 1.2–5.0). If all missing bearings were CoXLP the adjusted 7–13-year HR for CoXLP increased from 2.1 (CI 1.0–4.6) to 2.3 (CI 1.2–4.6) (Table 3 and Table 7, see Appendix). 53% of patients with missing bearings were operated on between 2005 and 2009.
Discussion
To our knowledge this study has the longest follow-up compared with other population-based studies on the HR of revision based on THA bearings in young patients. Compared with MoXLP, MoM had higher HR from 2 years postoperatively. MoXLP, CoC, and CoXLP had similar HRs.
Stemmed cementless MoM THAs have previously shown a higher risk of revision than metal-on-polyethylene THAs up to 8 years after surgery (8), but our study shows the increased HR persists up to 13 years after surgery. Continued surveillance of patients having MoM THA is therefore merited although the format may be discussed (9). The reasons for this increased HR were mainly revision due to “other” reasons, which include adverse reaction to metal debris (ARMD). However, ARMD is not specifically identified as a revision cause in the NARA dataset. A register that identifies ARMD as a specific revision cause has observed an increased revision rate for ARMD in MoM THA (19). Fewer women had MoM THA, possibly founded in precautions concerning teratogenicity from metal ion release in patients in the fertile age.
The adjusted 7–13-year HR for revision of CoC was similar to that of MoXLP in our study. This is in accordance with the results in annual reports of some national registers for all diagnoses and age groups (1,3). It is also in accordance with 1 study (11) but contradicts the results of another study using data from the National Joint Registry of England, Wales, Northern Ireland, and Isle of Man. However, the latter did not exclude hip fracture, inflammatory arthritis, femoral head osteonecrosis, or “unspecified diagnoses” (12). Earlier generations of CoC had a higher risk of liner and head fracture (18,20,21), and we could not adjust for generation of ceramic in our study. However, the sensitivity analysis including only CoC THAs with head size > 28 mm did not change our results statistically significantly. Apart from registry studies, some meta-analyses of short- and mid-term RCTs on the survival of CoC, CoXLP, and MoXLP have shown no difference, but long-term meta-analyses of RCTs are lacking (22). Possible long-term effects of confounding by indication are therefore unknown.
The most common revision cause for CoC THA was “other” reasons. “Other” could partly consist of ceramic liner and head fracture, but the 1.5% of CoC THAs revised for “other” reasons in our study is a much higher frequency than ceramic fractures in other studies (18,20,21). “Other” could also cover revisions performed for squeaking, another well-known complication of CoC THA that negatively affect patient-reported outcomes (23) but rarely leads to revision surgery (24).
CoXLP and MoXLP had similar HR of revision in all 3 periods. Some studies and annual reports of hip registries show similar survival (1,2,25). Other studies have reported lower revision risk with use of CoXLP, but these studies included other types of fixation and diagnoses than we did (11,12). One of these studies (15) did not distinguish between highly crosslinked polyethylene and conventional polyethylene, which might not be equally distributed between the groups. Nor did they perform separate analyses specifically for young patients. Our follow-up was longer than in these studies but studies with even longer follow-up are needed.
Strengths and limitations
The strength of this study is the large study population with prospectively collected data. Possible selection bias is limited due to high completeness of data.
However, there are also several limitations. The revision causes ARMD as well as liner and head fracture are not specified in the NARA dataset. When these revision causes are merged from the national hip arthroplasty registries they are registered as “other” along with a wide range of other categories (e.g., component failure, osteolysis without loosening, other) that does not fit the 5 previously mentioned specific revision causes in the NARA dataset.
This study contains possible confounding by indication as both MoM and CoC THA were originally introduced for the active and young patients (6). While MoM and CoC was almost used as a standard in 1 country these bearings were used less often in other countries and thus for selected patients (Table 1). High activity level may result in higher wear rates of bearings compared with less active patients with MoXLP bearings. However, we are unable to adjust for unmeasured confounding such as activity, occupation, and comorbidity from the available data.
Well-performing stems and cups might not be equally distributed in all bearing groups, but the possible bias this distribution could create between CoC and MoXLP THA is addressed to some extent by the sensitivity analysis of the 5 most common stems and cups in CoC THA without changing the results.
We cannot adjust for generation of ceramic, which is a known risk factor for femoral head fracture, especially for 28 mm heads (18). Even though the 4th generation of ceramic was introduced in 2004, we cannot know when it became dominant in this dataset. However, the sensitivity analysis with the 5 most common stem and cup combinations in CoC THA without 28 mm heads did not change the results.
We excluded 2,252 patients because of missing information on type of bearing. This could result in possible information bias if 1 bearing group was more likely to have missing bearings. Only the worst-case scenario with all missing bearings being CoC or CoXLP changed the results markedly. However, 53% of the missing bearings were operated on between 2005 and 2009, which is before CoC and CoXLP were widely used. We therefore consider the possible impact of the information bias as low.
Few THAs with femoral heads < 28 mm were found and excluded from the study (Figure 1). This probably means that cups in patients with hip dysplasia and very small acetabulae were fixated using cement and therefore excluded from the study. Our results might therefore not be translated to the more complex patients with childhood hip disorders.
Conclusion
MoXLP had higher revision-free survival and lower HR for revision than MoM, mainly for revision causes we cannot specify. MoXLP, CoC, and CoXLP had similar survival and HR for revision, but longer follow-up is needed to investigate whether they differ significantly. In perspective, we currently believe that either MoXLP, CoC, or CoXLP could be the standard bearings in patients aged 20–55 years.
- Australian Orthopaedic Association. National Joint Replacement Registry Annual Report 2021. Available from: https://aoanjrr.sahmri.com/annual-reports-2021.
- Danish Hip Arthroplasty Register. Annual Report 2021. Available from: danskhoftealloplastikregister.dk/wp-content/uploads/2021/08/ DHR-aarsrapport-2021_Offentliggoerelse.pdf.
- National Joint Registry 17th Annual Report 2020—National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. PMID: 33439585. Available from: www.njrcentre.org.uk.
- Saleh K J, Celebrezze M, Kassim R, Dykes D C, Gioe T J, Callaghan J J, et al. Functional outcome after revision hip arthroplasty: a meta-analysis. Clin Orthop Relat Res 2003; (416): 254-64. doi: 10.1097/01.blo.0000093006.90435.43.
- Jacobs J J, Shanbhag A, Glant T T, Black J, Galante J O. Wear debris in total joint replacements. J Am Acad Orthop Surg 1994; 2(4): 212-20. doi: 10.5435/00124635-199407000-00004.
- Zagra L, Gallazzi E. Bearing surfaces in primary total hip arthroplasty. EFORT Open Rev 2018; 3(5): 217-2. doi: 10.1302/2058-5241.3.180300.
- Australian Orthopaedic Association. National Joint Replacement Registry Annual Report 2012. Available from: https://aoanjrr.sahmri.com/annual-reports-2012.
- Varnum C, Pedersen A B, Mäkelä K, Eskelinen A, Havelin L I, Furnes O, et al. Increased risk of revision of cementless stemmed total hip arthroplasty with metal-on-metal bearings. Acta Orthop 2015; 86(4): 491-7. doi: 10.3109/17453674.2015.1023132.
- Matharu G S, Judge A, Eskelinen A, Murray D W, Pandit H G. What is appropriate surveillance for metal-on-metal hip arthroplasty patients?: a clinical update. Acta Orthop 2018; 89(1): 29-39. doi: 10.1080/17453674.2017.1398011.
- Heckmann N D, Sivasundaram L, Stefl M D, Kang H P, Basler E T, Lieberman J R. Total hip arthroplasty bearing surface trends in the United States from 2007 to 2014: the rise of ceramic on polyethylene. J Arthroplasty 2018; 33(6): 1757-63.e1. doi: 10.1016/j.arth.2017.12.040.
- Holleyman R J, Critchley R J, Mason J M, Jameson S S, Reed M R, Malviya A. Ceramic bearings are associated with a significantly reduced revision rate in primary hip arthroplasty: an analysis from the National Joint Registry for England, Wales, Northern Ireland, and the Isle of Man. J Arthroplasty 2021; 36(10): 3498-506. doi: 10.1016/j.arth.2021.05.027.
- Davis E T, Pagkalos J, Kopjar B. Effect of bearing surface on survival of cementless and hybrid total hip arthroplasty: study of data in the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. JB JS open access 2020; 5(2): e0075. doi: 10.2106/JBJS.OA.19.00075.
- Sedrakyan A, Graves S, Bordini B, Pons M, Havelin L, Mehle S, et al. Comparative effectiveness of ceramic-on-ceramic implants in stemmed hip replacement: a multinational study of six national and regional registries. J Bone Joint Surg Am 2014; 96(Suppl. 1): 34-41. doi: 10.2106/JBJS.N.00465.
- The Nordic Council of Ministers. Formal Nordic Co-Operation. Available from: http//www.norden.org/en.
- Mäkelä K T, Matilainen M, Pulkkinen P, Fenstad A M, Havelin L I, Engesaeter L, et al. Countrywise results of total hip replacement. Acta Orthop 2014; 85(2): 107-16. doi: 10.3109/17453674.2014.893498.
- Mäkelä K T, Furnes O, Hallan G, Fenstad A M, Rolfson O, Kärrholm J, et al. The benefits of collaboration: the Nordic Arthroplasty Register Association. EFORT Open Rev 2019; 4(6): 391-400. doi: 10.1302/20585241.4.180058.
- Engesæter L B, Engesæter I O, Fenstad A M, Havelin L I, Kärrholm J, Garellick G, et al. Low revision rate after total hip arthroplasty in patients with pediatric hip diseases. Acta Orthop 2012; 83(5): 436-41. doi: 10.3109/17453674.2012.736171.
- Howard D P, Wall P D H, Fernandez M A, Parsons H, Howard P W. Ceramic-on-ceramic bearing fractures in total hip arthroplasty. Bone Joint J 2017; 99(8): 1012-9. doi: 10.1302/0301-620X.99B8.BJJ-20170019.R1.
- de Steiger R N, Hatton A, Peng Y, Graves S. What is the risk of THA revision for ARMD in patients with non-metal-on-metal bearings? A study from the Australian National Joint Replacement Registry. Clin Orthop Relat Res 2020; 478(6): 1244-53. doi: 10.1097/CORR.0000000000001277.
- Hoskins W, Rainbird S, Peng Y, Lorimer M, Graves S E, Bingham R. Incidence, risk factors, and outcome of ceramic-on-ceramic bearing breakage in total hip arthroplasty. J Arthroplasty 2021; 36(8): 2992–7. doi: 10.1016/j.arth.2021.03.021.
- Hallan G, Fenstad A M, Furnes O. What is the frequency of fracture of ceramic components in THA? Results from the Norwegian Arthroplasty Register from 1997 to 2017. Clin Orthop Relat Res 2020; 478(6): 1254-61. doi: 10.1097/CORR.0000000000001272.
- Wyles C C, Jimenez-Almonte J H, Murad M H, Norambuena-Morales G A, Cabanela M E, Sierra R J, et al. There are no differences in short- to mid-term survivorship among total hip-bearing surface options: a network meta-analysis. Clin Orthop Relat Res 2015; 473(6): 2031-41. doi: 10.1007/s11999-014-4065-0.
- Varnum C, Pedersen A B, Kjærsgaard-Andersen P, Overgaard S. Do different types of bearings and noise from total hip arthroplasty influence hip-related pain, function, and quality of life postoperatively? Acta Orthop 2016; 87(6): 567-74. doi: 10.1080/17453674.2016.1225649.
- Owen D H, Russell N C, Smith P N, Walter W L. An estimation of the incidence of squeaking and revision surgery for squeaking in ceramicon-ceramic total hip replacement: a meta-analysis and report from the Australian Orthopaedic Association National Joint Registry. Bone Joint J 2014; 96-B(2): 181-7. doi: 10.1302/0301-620X.96B2.32784.
- Cafri G, Paxton E W, Love R, Bini S A, Kurtz S M. Is there a difference in revision risk between metal and ceramic heads on highly crosslinked polyethylene liners? Clin Orthop Relat Res 2017; 475(5): 1349-55. doi: 10.1007/s11999-016-4966-1.
Appendix
| Period Bearing | Number at risk | Number of revisions | Unadjusted HR (CI) | Adjusted a HR (CI) |
| Only males a | ||||
| 0–2 years | ||||
| MoXLP | 5,479 | 124 | 1 (ref.) | 1 (ref.) |
| MoM | 1,240 | 22 | 0.8 (0.5–1.2) | 0.8 (0.4–1.6) |
| CoC | 2,021 | 42 | 0.9 (0.6–1.3) | 1.0 (0.7–1.5) |
| CoXLP | 2,983 | 87 | 1.3 (1.0–1.7) | 1.3 (1.0–1.7) |
| 2–7 years | ||||
| MoXLP | 4,589 | 68 | 1 (ref.) | 1 (ref.) |
| MoM | 1,208 | 63 | 2.4 (1.7–3.4) | 2.8 (1.5–5.0) |
| CoC | 1,846 | 32 | 1.0 (0.6–1.5) | 1.1 (0.7–1.8) |
| CoXLP | 2,320 | 39 | 1.2 (0.8–1.8) | 1.2 (0.8–1.8) |
| 7–13 years | ||||
| MoXLP | 1,420 | 6 | 1 (ref.) | 1 (ref.) |
| MoM | 1,081 | 47 | 6.7 (2.9–16) | 3.4 (1.2–10) |
| CoC | 766 | 19 | 3.3 (1.3–8.3) | 3.3 (1.3–8.7) |
| CoXLP | 662 | 6 | 2.0 (0.7–6.3) | 2.2 (0.7–6.8) |
| Only OA b | ||||
| 0–2 years | ||||
| MoXLP | 8,255 | 205 | 1 (ref.) | 1 (ref.) |
| MoM | 1,960 | 49 | 1.0 (0.8–1.4) | 1.4 (0.8–2.3) |
| CoC | 3,347 | 81 | 1.0 (0.8–1.3) | 1.1 (0.8–1.5) |
| CoXLP | 4,562 | 131 | 1.3 (1.0–1.6) | 1.2 (1.0–1.5) |
| 2–7 years | ||||
| MoXLP | 6,879 | 90 | 1 (ref.) | 1 (ref.) |
| MoM | 1,899 | 132 | 3.3 (2.5–4.2) | 3.4 (2.2–5.4) |
| CoC | 3,055 | 49 | 0.8 (0.6–1.2) | 0.9 (0.6–1.3) |
| CoXLP | 3,508 | 58 | 1.2 (0.9–1.7) | 1.2 (0.9–1.7) |
| 7–13 years | ||||
| MoXLP | 2,190 | 13 | 1 (ref.) | 1 (ref.) |
| MoM | 1,675 | 99 | 6.4 (3.6–12) | 3.2 (1.5–6.6) |
| CoC | 1,326 | 31 | 3.0 (1.6–5.8) | 2.4 (1.2–4.7) |
| CoXLP | 995 | 10 | 1.6 (0.7–3.7) | 1.6 (0.7–3.7) |
| Only 5 most common CoC THAs after 2005 c | ||||
| 0–2 years | ||||
| MoXLP | 10,325 | 231 | 1 (ref.) | 1 (ref.) |
| CoC | 1,979 | 40 | 0.9 (0.6–1.2) | 0.9 (0.6–1.2) |
| 2–7 years | ||||
| MoXLP | 8,639 | 118 | 1 (ref.) | 1 (ref.) |
| CoC | 1,820 | 21 | 0.8 (0.5–1.2) | 0.8 (0.5–1.2) |
| 7–13 years | ||||
| MoXLP | 2,836 | 16 | 1 (ref.) | 1 (ref.) |
| CoC | 564 | 11 | 5.3 (2.4–12) | 5.1 (2.4–11) |
| a Adjusted for diagnosis and year of primary surgery. b Adjusted for sex, age, year of primary surgery, and femoral head size. c Adjusted for sex and diagnosis. |
||||