Similar revision rate after cemented and cementless femoral revisions for periprosthetic femoral fractures in total hip arthroplasty: analysis of 1,879 revision hip arthroplasties in the Dutch Arthroplasty Register
Bart VAN DOOREN 1,2,a, Rinne M PETERS 1,3,a, Paul C JUTTE 2, Martin STEVENS 2, B Willem SCHREURS 4,5, and Wierd P ZIJLSTRA 1
1 Department of Orthopaedics, Medical Center Leeuwarden, Leeuwarden; 2 Department of Orthopaedics, University of Groningen, University Medical Center Groningen, Groningen; 3 Department of Orthopaedics, Martini Hospital, Groningen; 4 Department of Orthopaedics, Radboudumc, Nijmegen; 5 Dutch Arthroplasty Register (LROI), ‘s Hertogenbosch, The Netherlands
a Shared first authorship
Background and purpose — Periprosthetic femoral fracture (PPF) after total hip arthroplasty (THA) is a serious complication, as it often is followed by functional deficits and morbidity. There is no consensus regarding the optimal stem fixation method and whether additional cup replacement is beneficial. The aim of our study was to perform a direct comparison of reasons and risk of re-revision between cemented and uncemented revision THAs following PPF using registry data.
Patients and methods — 1,879 patients registered in the Dutch Arthroplasty Registry (LROI) who underwent a first-time revision for PPF between 2007 and 2021 (cemented stem: n = 555; uncemented stem: n = 1,324) were included. Competing risk survival analysis and multivariable Cox proportional hazard analyses were performed.
Results — 5- and 10-year crude cumulative incidence of re-revision following revision for PPF was similar between cemented (resp. 13%, 95% CI 10–16 and 18%, CI 13–24) and uncemented (resp. 11%, CI 10–13 and 13%, CI 11–16) revisions. Multivariable Cox regression analysis, adjusting for potential confounders, showed a similar risk of revision for uncemented and cemented revision stems. Finally, we found no difference in risk of re-revision between a total revision (HR 1.2, 0.6–2.1) compared with a stem revision.
Conclusion — We found no difference in the risk of re-revision between cemented and uncemented revision stems after revision for PPF.
Citation: Acta Orthopaedica 2023; 94: 260–265. DOI: https://doi.org/10.2340/17453674.2023.13211.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-07. Accepted: 2023-04-22. Published: 2023-05-22.
Correspondence: Correspondence: bart.van.dooren@mcl.nl
The authors thank Nic Veeger, statistician of the Medical Center Leeuwarden (MCL) for his assistance in performing the statistical analysis.
Authors contributed to: (1) study design and study protocol, (2) gathered data, (3) analyzed data, (4) initial draft, and (5) final draft. BvD contributed to 1,3-5; RMP, WPZ, and BWS contributed to 1, 4, and 5; PCJ and MS contributed to 4 and 5.
Handling co-editors: Cecilia Rogmark and Philippe Wagner
Acta thanks Johan Kärrholm and Dominic Meek for help with peer review of this study.
Revision arthroplasty for periprosthetic femoral fracture (PPF) accounts for 14% of all revisions following primary THA in the Netherlands (1). For patients, PPF is a serious complication, as it often results in pain, functional deficits, and increased mortality. PFF often occurs in fragile patients (2-5).
Essential in the management of PPFs is assessing the stability of the femoral stem and bone quality (6). The most frequently used classification for PPFs is the Vancouver classification, which describes the fracture configuration with corresponding treatment (2,7). Vancouver B2 or B3 fractures occur around or just distal to the tip of the stem, resulting in a loose femoral stem, generally requiring revision surgery (6). Surgery to treat such PPFs can be complex, requiring fracture fixation with or without revision of the implant depending on fracture pattern, bone defect size, patient characteristics, and experience of the surgeon (2,7).
The fixation technique during stem revision has been subject to debate over the last decades. In the past, long cemented revision stems have been advocated based on various studies (8-9). However, other studies suggest favorable outcomes in terms of implant survival for uncemented revision stems (10-12). Most of these studies are limited by design and number of patients. Stronger evidence is needed regarding evaluation of fixation technique during revision for PPFs. Moreover, it is unknown whether additional cup revision is beneficial in order to reduce the risk of postoperative dislocation.
Our primary aim was to examine the difference in modes of failure and risk of re-revision between cemented and uncemented femoral stem revision in the case of a PPF, using Dutch arthroplasty registry data. In addition, we examined the difference in risk of re-revision of a stem revision only compared with a total revision following a PPF.
Patients and methods
The study was designed in accordance with STROBE guidelines (13). A retrospective observational study was performed using data from the Dutch Arthroplasty Register (LROI), a nationwide population-based register initiated by the Dutch Orthopaedic Association. The register started in 2007 and collects data on all primary and revision joint arthroplasties in the Netherlands. The register covers 100% of Dutch hospitals with a completeness of 99% for primary THAs. The coverage of revision hip arthroplasties has been estimated to be over 97% in the last 5 years (1). The register contains demographic data, procedures, and prosthesis characteristics.
Selection of procedures
All registered first-time revision THAs due to a PPF between 2007 and 2021 were eligible for inclusion. We included only cases which after the revision had both components cemented or uncemented, thus implants which after revision for PPF remained or became converted to hybrids or reverse hybrids were excluded from our analysis. 1,879 revision THAs for PPF were analyzed (Figure 1). Revision was defined as change, addition, or removal of one or more components of the prosthesis. Fracture fixation alone by open reduction and internal fixation (ORIF) was not registered in the LROI. Similarly, cases in which non-surgical treatment was chosen were not included in the registry.
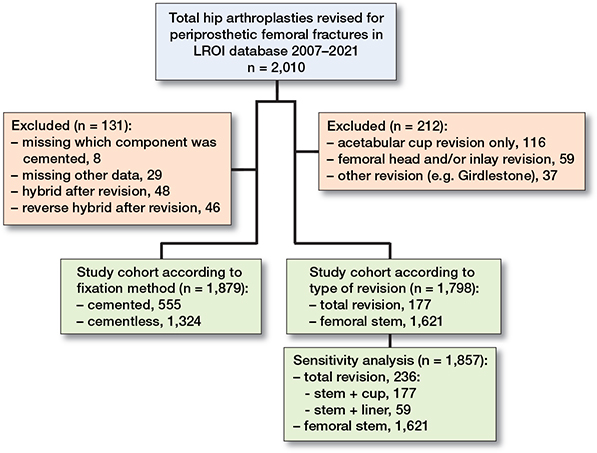
Figure 1. Flowchart of included procedures.
Outcome measures
Risk of re-revision for any reason in cemented and uncemented femoral stem revisions for a PPF was defined as our primary outcome variable. In addition, we examined the difference in reasons for re-revision between cemented and uncemented revision stems after revision of a PPF. Finally, we investigated the difference in risk of re-revision due to any reason after stem revision only, compared with stem and cup revision (total revision) at the revision procedure. Additional cup revision in the total revision group was defined as a complete revision of the acetabular shell. Conversion of a fixed acetabular shell to a dual mobility cup by cementing a dual mobility cup into a fixed metallic shell was registered as a cup revision. An additional liner exchange was excluded from our main analysis. However, we assume that stem revisions combined with liner exchange can affect the risk of re-revision. Therefore, we performed an additional sensitivity analysis where we calculated the risk of re-revision due to any reason after stem revision only, compared with stem and cup revision and/or liner exchange (Figure 1).
Statistics
Group comparisons were made using a chi-square test to test for differences in patient and prosthesis characteristics. A competing risk analysis was used to estimate the time to re-revision for any reason after revision for PPF. The event of interest was the first re-revision, with mortality as a competing risk. Furthermore, we calculated the crude cumulative incidence of re-revision between a total revision and a stem revision only.
Multivariable Cox proportional hazards models were used to estimate hazard ratios associated with implant survival following revision arthroplasty for PPF. We included sex, age, BMI, ASA score, and head size as confounders because these factors influence both exposure (fixation) and outcome (risk of re-revision). We checked the proportional hazard assumption by evaluating the Schoenfeld residuals for each variable and found that the proportional hazard assumption was not violated. For all tests, a 2-tailed significance level of p < 0.05 was used. Results were reported as hazard ratios (HR) with 95% confidence intervals (CI). The statistical software programs SPSS version 24.0 (IBM Corp, Armonk, NY, USA) and R Statistical Software (version 2022.12.0: R Foundation for Statistical Computing, Vienna, Austria) were used.
Sensitivity analysis
First, we examined the difference in risk of re-revision following revision of a PPF with a stem revision only, compared with a total revision (including cup revision). We assume the increased dislocation risk after femoral revision only might be partly explained by worn polyethylene of the acetabular component in hip prostheses that were placed years ago. Therefore, we performed a sensitivity analysis where patients in whom a femoral head/liner change was performed were added to the total revision group (Figure 1).
Ethics, funding, data sharing, and disclosures
The study was approved by the scientific advisory committee and board of the LROI and the Medical Ethics Committee of our local hospital (no. METc 2021/280). The dataset was processed in compliance with the regulations of the LROI governing research on registry data. Data is available from the LROI, but restrictions apply to the availability of this data. This project was supported by an unrestricted grant from a non-profit foundation (Stichting MCL fonds). No benefits in any form have been received or will be received related directly or indirectly to the subject of this article. No conflicting interests were declared. Completed disclosure forms for this article following the ICMJE template are available on the article page, DOI: 10.2340/17453674.2023.13211
Results
Of all registered primary THAs in the LROI, 2,010 had been revised due to a PPF since the start (January 1, 2007) until the end of the follow-up period (December 31, 2021). The study cohort, after excluding hybrids, reverse hybrids, and cases with missing data, comprised 1,879 revisions. The mean follow-up of the revision was 4.1 years (range 0–14.7 years), without differences between groups (cemented vs. uncemented revisions). We found significant differences in sex, head size, and articulation between cemented and cementless revisions (Table 1).
| Factor | Femoral fixation at revision | Total n = 1,879 | |
| Cemented n = 555 | Cementless n = 1,324 | ||
| Age | |||
| < 60 | 55 (10) | 122 (9.2) | 177 (9.4) |
| 60–74 | 234 (42) | 581 (44) | 815 (43) |
| 75 | 266 (48) | 620 (47) | 886 (47) |
| Sex | |||
| Male | 144 (26) | 419 (32) | 563 (30) |
| Female | 411 (74) | 903 (68) | 1,314 (70) |
| ASA score a | |||
| I | 39 (7.0) | 108 (8.2) | 147 (7.9) |
| II | 280 (51) | 712 (54) | 992 (53) |
| III–IV | 232 (42) | 490 (37) | 722 (39) |
| Primary diagnosis a,b | |||
| Osteoarthritis (OA) | 429 (79) | 1,088 (83) | 1,517 (82) |
| Non-OA | 113 (21) | 225 (17) | 338 (18) |
| Operation year | |||
| 2007–2011 | 48 (8.7) | 166 (13) | 214 (11) |
| 2012–2016 | 185 (33) | 411 (31) | 596 (32) |
| 2017–2021 | 322 (58) | 747 (56) | 1,069 (57) |
| Smoking a | |||
| Yes | 405 (10) | 917 (10) | 1,322 (10) |
| No | 44 (90) | 102 (90) | 146 (90) |
| Body mass index a | |||
| < 18.5 | 12 (2.7) | 23 (2.2) | 35 (2.4) |
| 18.5–25 | 201 (45) | 455 (44) | 656 (44) |
| 25–30 | 161 (36) | 383 (37) | 544 (37) |
| 30–40 | 70 (16) | 161 (16) | 231 (16) |
| > 40 | 7 (1.6) | 12 (1.2) | 19 (1.3) |
| Charnley a | |||
| A | 168 (50) | 407 (50) | 575 (50) |
| B1 | 56 (17) | 128 (16) | 184 (16) |
| B2 | 87 (26) | 216 (26) | 303 (26) |
| C | 24 (7.2) | 65 (8.0) | 89 (7.7) |
| Head size, mm | |||
| 22–28 | 206 (37) | 298 (23) | 504 (27) |
| 32 | 214 (39) | 584 (44) | 798 (43) |
| 36 | 92 (17) | 306 (23) | 398 (21) |
| ≥ 38 | 43 (7.7) | 136 (10) | 179 (9.5) |
| Articulation a,c | |||
| CoC | 14 (3.0) | 43 (3.9) | 57 (3.6) |
| CoM | 0 (0) | 5 (0.4) | 5 (0.3) |
| CoP | 155 (33) | 562 (50) | 717 (45) |
| MoC | 0 (0) | 3 (0.3) | 3 (0.2) |
| MoP | 257 (55) | 398 (36) | 655 (41) |
| MoM | 1 (0.2) | 24 (2.2) | 25 (1.6) |
| ZoP | 41 (8.8) | 79 (7.1) | 122 (7.6) |
| a Numbers do not add up to total due to unknown or missing values. b Non-OA was defined as fracture, late post-traumatic OA, osteonecrosis, dysplasia, post-Perthes, rheumatoid arthritis or tumor. c CoC: ceramic-on-ceramic, CoM: ceramic-on-metal, CoP: ceramic-on-polyethylene, MoC: metal-on-ceramic, MoP: metal-on-polyethylene, ZoP: oxidized-zirconium-on-polyethylene. |
|||
Reason for revision
The most frequently registered reasons for re-revision were infection (3.4%) and dislocation (3.3%). Reasons for re-revision were similar between groups. However, cemented revision stems (3.6%) were re-revised more often for PPF compared with uncemented revision stems (1.6%) (Table 2). In addition, cemented revisions (2.7%) were re-revised more often because of loosening of the acetabular component compared with cementless revisions (1%).
Risk of re-revision
205 (11%) revisions for PPF were re-revised during the follow-up period (Table 2). 164 (80%) re-revisions were registered within 2 years after the initial revision for PPF. The overall 2-year mortality rate was 8.2% (155/1,879 patients). 67/555 (12%) of the cemented revision stems were re-revised compared with 138/1,324 (10%) in the uncemented revision group.
The 5- and 10-year crude cumulative incidence of re-revision following revision for PPF was similar between cemented (13%, 95% CI 10–16 and 18%, CI 13–24) and uncemented (11%, CI 10–13 and 13%, CI 11–16) revisions (Figure 2). Multivariable Cox regression analysis, adjusting for age, sex, ASA score, BMI, and head size, showed no significant difference in risk of re-revision between cemented and uncemented revisions (HR 1.1, CI 0.8–1.6) (Table 3).
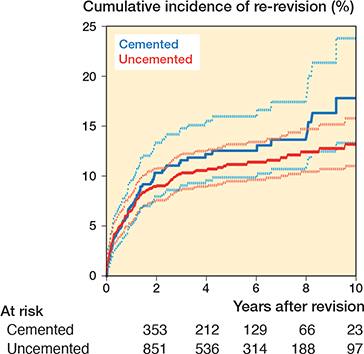
Figure 2. Crude cumulative incidence of re-revision for any reason in revision THAs following a periprosthetic fracture between 2007 and 2021 in the Netherlands. Cemented vs. uncemented fixation, including number at risk by time.
| Fixation | Re-revisions n = 205 | Crude hazard ratio (CI) | Adjusted a hazard ratio (CI) |
| Uncemented | 138 | 1.0 (reference) | 1.0 (reference) |
| Cemented | 67 | 1.2 (0.9–1.6) | 1.1 (0.8–1.6) |
| a Adjusted for age, sex, ASA-score, BMI, and head size. | |||
Femoral stem revision vs. total revision
In 1,621 patients an isolated femoral stem revision was performed. A total revision (femoral revision + additional cup replacement) was performed in another 177 patients. 168/1,621 (10%) with a femoral revision only and 17/177 (9.6%) with a total revision were re-revised (Table 4).
The 1- and 3-year crude cumulative incidence of re-revision was similar after isolated femoral stem revisions (6.5%, CI 5–8 and 10%, CI 9–12) and after total revisions (7%, CI 4–12 and 10%, CI 6–16) (Figure 3). Patients who underwent a total revision for PPF had an adjusted risk of re-revision for any reason similar to patients who received an isolated femoral stem revision (HR 1.2, CI 0.6–2.1) (Table 5).
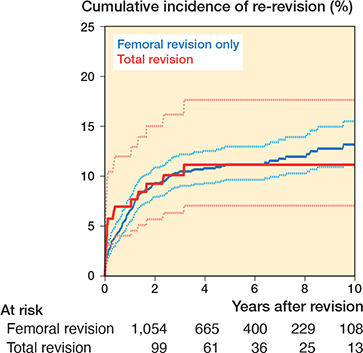
Figure 3. Crude cumulative incidence of re-revision for any reason in revision THAs following a periprosthetic fracture between 2007 and 2021 in the Netherlands. Femoral revision vs. total revision, including number at risk. For the total revision group, crude cumulative incidence of re-revision after 5 years should be interpreted with caution due to low numbers at risk (n < 50).
| Revision | Re-revisions n = 185 | Crude hazard ratio (CI) | Adjusted a hazard ratio (CI) |
| Total | 17 | 1.0 (reference) | 1.0 (reference) |
| Femoral | 168 | 1.0 (0.6–1.6) | 1.2 (0.6–2.1) |
| a Adjusted for age, sex, ASA-score, BMI, and head size. | |||
Revision for dislocation (femoral stem revision vs. total revision)
58/185 (31%) of all re-revisions were performed due to dislocation, in 4/177 (2.3%) as total revisions and in 54/1,621 (3.3%) as isolated stem revisions. The difference in dislocation rate was not statistically significant between a total revision and an isolated femoral stem revision (P = 0.4). Risk (ratio) of re-revision due to dislocation was not estimated as the number of dislocation re-revisions was low in the total revision group.
Sensitivity analysis
In our main analysis we compared subsequent femoral stem revisions with a total revision. We assume that stem revisions combined with liner exchange can affect the risk of re-revision. Therefore, an additional sensitivity analysis was performed. In this sensitivity analysis stem revisions combined with liner exchange (n = 59) were added to the total revision group (Figure 1). Thereafter, we compared the risk of re-revision of a femoral stem revision only with the “new” total revision group (stem revision + acetabular shell revision and/or liner exchange). We found no statistically significant difference in risk of re-revision for patients with a stem revision only compared with the “new” total revision group (HR 1.0, CI 0.6–1.8).
Discussion
Using nationwide data from the Dutch Arthroplasty Register, no differences were found in the risk of re-revision in patients with either a cemented or an uncemented femoral revision stem after a PPF. However, cemented revision stems were re-revised more often for periprosthetic re-fracture compared with the uncemented group (Table 2). Finally, we found no difference in risk of re-revision for patients with a stem revision only compared with a total revision (additional cup replacement) following revision of a PPF. There was no trend towards fewer dislocation revisions if the cup was revised too. Although results were not statistically different, the generalizability of these results is subject to certain limitations, as the number of included patients was low.
The available literature regarding optimal fixation comparing long cemented femoral stems and distally tapered uncemented stems in PPFs is very scarce. Most of these studies are limited by (retrospective) design and number of inclusions (10-11,14-15). One registry-based study with data from the Swedish Hip Arthroplasty Register compared the outcomes of cemented and cementless fixation for Vancouver B2 and B3 periprosthetic fractures (16). They reported no differences in risk of revision among cemented, cementless monoblock, and cementless modular revision components for the treatment of type B2 and B3 fractures, which is in line with our results. A recent study compared the outcome of long cemented stems and uncemented revision stems used in PPFs (10). Although early surgical complications were reported in both groups, an increased morbidity and complication rate was seen in the long-stemmed cemented group. Earlier, Springer et al. evaluated 42 cemented revision THAs and 28 proximally porous-coated uncemented femoral stems in patients with Vancouver type-B PPF (14). They reported that the uncemented, porous-coated implants had the highest likelihood of stable fixation. In contrast, another recent retrospective study reported no difference in revision rate, patient survivorship, complications, readmissions, or length of in-hospital stay between uncemented and cemented stem revisions for a Vancouver B2 periprosthetic fracture (12). When Kennedy et al. (15) compared the outcomes of cement-in-cement revisions versus long uncemented revision stems for B2 fractures, a comparable re-revision rate was found between groups (17% versus 19%). Complication rates did not differ between the cemented and uncemented group, which is in line with our results. In our study, the implant survival up to 10 years of uncemented and cemented revision stems after revision for PPF was similar.
We found no difference in the risk of re-revision after isolated femoral stem versus total revisions at the index revision procedure. As demonstrated, dislocation was one of the most frequently reported indications for re-revisions after revision for PPF (58 of 185 re-revisions after PPF revision arthroplasty). This might be partly explained by worn polyethylene of the acetabular component at the time of the revision, a smaller (i.e., 28 mm) femoral head size which was often used in the past, and the enlarged soft tissue exposure needed to address the PPF. In addition, the frailty of this comorbid and aged patient category may lead to an increased dislocation risk. For primary THAs, larger head sizes reduce the risk of dislocation (17). In our data, larger femoral head sizes (resp. 32 and 36 mm) were more frequently registered for patients with a uncemented revision THA. However, there was no difference in the risk of re-revision and risk of dislocation re-revision between cemented and uncemented revision THAs.
To reduce the risk of dislocation following revision surgery for PPFs, a decision is taken either before or during surgery whether to revise the cup. Based on Swedish registry data, the risk of re-revision was 50% reduced when the cup too was revised after aseptic femoral hip revision surgery (versus femoral revision only) (7). Whether or not this also applies for PPF revision surgery has not been found in the literature. Our data suggests no trend favoring total revision in patients with a PPF in order to reduce the risk of re-revision due to dislocation. Nevertheless, the number of re-revisions for dislocation after a total revision was very low with only 4 revisions due to dislocation. In addition, mixed reasons for re-revision were registered. Therefore, our results should be interpreted with caution.
The major strength of our study is the relatively high number of patients included. To our knowledge, only one previous nationwide registry study reported on the outcomes of cemented and uncemented revisions after PPF (16). Our study has several limitations. First, the LROI does not contain information regarding the presence or magnitude of any femoral bone defect, a factor that can affect the choice for fixation and subsequently the outcome in terms of re-revision rates. Furthermore, treatment strategies and the use of cemented fixation can be influenced by parameters such as the fracture pattern. For example, in the case of a comminuted fracture pattern, cemented fixation may not be feasible. A second limitation is that information on femoral stem type after revision for PPF was missing. Therefore, we could not determine if a standard-length stem or a long cemented stem was used. In addition, a potential weakness of our study is that not all PPFs are registered. When the stem is well fixed (Vancouver A, B1, or C) and the PPF is treated with plate or cable osteosynthesis only, without revision of the femoral component, the procedure is not registered in the LROI. Neither are cases treated non-surgically, for example closed reduction of dislocations, nor patients treated with open reduction without component exchange. Although this is a large cohort study, it has a limited number of patients. This is reflected in the relatively broad confidence intervals seen in our data. The study may remain underpowered for the primary outcome measure. Further studies with larger sample sizes are needed to address this limitation.
Our study raises a number of opportunities for future research. As mentioned earlier, re-revision for dislocation is a common complication after revision for PPF. In our study, additional cup revision was not superior to stem revision only. However, the number of these total revisions after PPF was low in our study. Future research with larger numbers, especially for re-revision for dislocation, will be necessary to compare the difference between a femoral stem revision only compared with a total revision.
Conclusion
Our study demonstrates that cemented and uncemented revision stems have similar re-revision rates and comparable reasons for re-revision. We found no difference in the risk of re-revision between a total revision or a femoral stem revision only. The generalizability of these results is subject to certain limitations, as the number of included patients was low.
- Dutch Arthroplasty Register (LROI). Annual report. LROI report, 2020. Numbers—LROI Report—Information on orthopaedic prosthesis procedures in the Netherlands (lroireport.nl). Last accessed July 2022.
- Bottle A, Griffiths R, White S, Wynn-Jones H, Aylin P, Moppett I, et al. Periprosthetic fractures: the next fragility fracture epidemic? A national observational study. BMJ Open 2020; 10(12): e042371. doi: 10.1136/bmjopen-2020-042371.
- Menken L G, Rodriguez J A. Femoral revision for periprosthetic fracture in total hip arthroplasty. J Clin Orthop Trauma 2020; 11(1): 16-21. doi: 10.1016/j.jcot.2019.12.003.
- Abdel M P, Cottino U, Mabry T M. Management of periprosthetic femoral fractures following total hip arthroplasty: a review. Int Orthop 2015; 39(10): 2005-10. doi: 10.1007/s00264-015-2979-0.
- Duncan C P, Masri B A. Fractures of the femur after hip replacement. Instr Course Lect 1995; 45: 293-304.
- Stoffel K, Horn T, Zagra L, Mueller M, Perka C, Eckardt H. Periprosthetic fractures of the proximal femur: beyond the Vancouver classification. EFORT Open Rev 2020; 5(7): 449-56. doi: 10.1302/2058-5241.5.190086.
- Tyson Y, Rolfson O, Kärrholm J, Hailer N P, Mohaddes M. Uncemented or cemented revision stems? Analysis of 2,296 first-time hip revision arthroplasties performed due to aseptic loosening, reported to the Swedish Hip Arthroplasty Register. Acta Orthop 2019; 90(5): 421-6. doi: 10.1080/17453674.2019.1624336.
- Hernigou P, Dupuys N, Delambre J, Guissou I, Poignard A, Allain J, et al. Long, titanium, cemented stems decreased late periprosthetic fractures and revisions in patients with severe bone loss and previous revision. Int Orthop 2015; 39(4): 639-44. doi: 10.1007/s00264-014-2528-2.
- Weiss R J, Stark A, Kärrholm J. A modular cementless stem vs. cemented long-stem prostheses in revision surgery of the hip: a population-based study from the Swedish Hip Arthroplasty Register. Acta Orthop 2011; 82(2): 136-42. doi: 10.3109/17453674.2011.566145.
- Sponer P, Korbel M, Grinac M, Prokes L, Bezrouk A, Kucera T. The outcomes of cemented femoral revisions for periprosthetic femoral fractures in the elderly: comparison with cementless stems. Clin Interv Aging 2021; 16: 1869-76. doi: 10.2147/CIA.S306463.
- Klasan A, Millar J, Quayle J, Farrington B, Misur P N. Comparable outcomes of in-cement revision and uncemented modular stem revision for Vancouver B2 periprosthetic femoral fracture at 5 years. Arch Orthop Trauma Surg 2022; 142(6): 1039-46. doi: 10.1007/s00402-021-03776-5.
- Schmale G A, Lachiewicz P F, Kelley S S. Early failure of revision total hip arthroplasty with cemented precoated femoral components: comparison with uncemented components at 2 to 8 years. J Arthroplasty 2000; 15(6): 718-29. doi: 10.1054/arth.2000.6623.
- Von Elm E, Altman D G, Egger M, Pocock S J, Gotzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370(9596): 1453-7. doi: 10.1016/S0140-6736(07)61602-X.
- Springer B D, Berry D J, Lewallen D G. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am 2003; 85(11): 2156-62. doi: 10.2106/00004623-200311000-00015.
- Kennedy J W, Hrycaiczuk A, Ng N Y B, Sheerins O, Patil S R, Jones B G, et al. Cement-in-cement versus uncemented modular stem revision for Vancouver B2 periprosthetic fractures. J Orthop 2022; 31: 124-8. doi: 10.1016/j.jor.2022.03.008.
- Chatziagorou G, Lindahl H, Kärrholm J. Surgical treatment of Vancouver type B periprosthetic femoral fractures: patient characteristics and outcomes of 1381 fractures treated in Sweden between 2001 and 2011. Bone Joint J 2019; 101-B(11): 1447-58. doi: 10.1302/0301-620X.101B11.BJJ-2019-0480.R2.
- Zijlstra W P, De Hartog B, Van Steenbergen L N, Scheurs B W, Nelissen R G H H. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop 2017; 88(4): 395-401. doi: 10.1080/17453674.2017.1317515.