Hip survival after periacetabular osteotomy in patients with acetabular dysplasia, acetabular retroversion, congenital dislocation of the hip, or Legg-Calvé-Perthes disease: a cohort study on 1,501 hips
Anne ROSENDAHL KRISTIANSEN 1, Anders HOLSGAARD-LARSEN 1, Morten BØGEHØJ 1, Søren OVERGAARD 2, Martin LINDBERG-LARSEN 1,a, and Ole OVESEN 1,a
1 Department of Orthopaedic Surgery and Traumatology, Odense University Hospital, and Orthopaedic Research Unit, Department of Clinical Research, University of Southern Denmark; 2 Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg, and Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark
a Shared last authorship
Background and purpose — Previous studies on hip survival following periacetabular osteotomy (PAO) have reported isolated data for the treatment of 1 underlying condition, making comparison between patient groups difficult. We report the hip survival after PAO in patients with acetabular dysplasia (AD), acetabular retroversion (AR), congenital dislocation of the hip (CDH), and Legg-Calvé-Perthes disease (LCPD) with total hip arthroplasty (THA) as primary endpoint and secondarily the risk of subsequent hip-related operations other than THA.
Patients and methods — From 1997 to December 2021, 1,501 hips (1,203 patients) underwent PAO in a single center (Odense University Hospital). We identified conversions to THA and other subsequent hip-related operations through patient files and the Danish National Patient Registry (DNPR).
Results — 123 (8.2%) of the total cohort of 1,501 hips were converted to THA within the study period. The overall Kaplan–Meier hip survival rate was 71% (95% confidence interval [CI] 61–79) at 24 years with a mean follow-up of 7.6 years (range 0.02–25). The individual Kaplan–Meier hip survival rates at 15 years were 81% (CI 76–86) for AD, 94% (CI 91–96) for AR, 84% (CI 66–93) for CDH, and 66% (CI 49–79) for LCPD. In total, the overall risk of additional hip-related operations was 48% (of which 92% were screw removal).
Conclusion — Encouragingly, 71% of hips were preserved 24 years after PAO. We found that AR patients had the highest (94%) PAO survivorship at 15 years compared with the other underlying hip conditions. Almost half of PAO patients may undergo later additional surgery, of which screw removal is the primary intervention. Overall long-term survival, risk factors for conversion to THA, and risk of additional surgery are relevant information for shared decision-making.
Citation: Acta Orthopaedica 2023; 94: 250–256. DOI: https://doi.org/0.2340/17453674.2023.12403.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-09-24. Accepted: 2023-04-09. Published: 2023-05-10.
Correspondence: Annek17@student.sdu.dk
OO was the initiator of this study. OO, SO, and MBØ performed the PAO procedures and registered data in the database at OUH during the study period. ARK, MLL, OO, AHL, MBØ, and SO were involved in the first outline and methodology of this study. ARK and MLL defined the analysis plan and did the first draft of the protocol and manuscript. All authors revised and approved the final protocol and manuscript. ARK and OO did the supplementary data collection. ARK did the statistics.
The authors would like to thank Odense Patient data Explorative Network (OPEN) for contribution of methodological advice.
Handling co-editors: Bart Swierstra and Philippe Wagner
Acta thanks Enrico De Visser and George Grammatopoulos for help with peer review of this study.
Periacetabular osteotomy (PAO) is a procedure used to treat a variety of hip-related conditions when non-surgical treatment has failed (1). The procedure is used for treatment of acetabular dysplasia (AD) – a condition with insufficient bony coverage of the femoral head; acetabular retroversion (AR) – a disorder where the acetabulum is retroverted and the hip has over-coverage anteriorly; congenital dislocation of the hip (CDH) – a rare condition seen in newborns, which can lead to residual dysplasia of the hip later in life; and Legg-Calvé-Perthes disease (LCPD) – primarily a childhood disease, where there is not enough blood flow to the femoral head, potentially leading to a complex deformity of the hip in adults/adolescents on both the femoral and acetabular side. All the above-mentioned conditions can lead to hip pain and secondary osteoarthritis (OA) (2-4).
For AD, the hip survival rates following PAO, with total hip arthroplasty (THA) as endpoint, have been reported to be 84–90% at 10 years (5,6) and 80–92% at 15 years (7,8). Studies on PAO in patients with AR have reported 10-year hip survival rates of 79–100% (9,10). Other studies have reported hip survival rates for CDH and AD merged as 1 group of developmental dysplasia (DDH) (5,7,8). Consequently, the hip survival rate after PAO in CDH patients is unknown.
Finally, a few studies report survival analysis on LCPD patients, but with varying methods, making a valid comparison impossible (11-13).
In summary, previous studies on hip survival following PAO have reported isolated data for the treatment of 1 underlying condition making comparison between patient groups difficult. Therefore, we investigated (i) the long-term hip survival rate after PAO in AD, AR, CDH, and LCPD patients using THA as primary endpoint, and (ii) risk factors of subsequent hip-related operations other than THA.
Patients and methods
The “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) Statement was used as guideline for reporting this observational retrospective cohort study (14).
Study population
The study population includes the entire consecutive cohort of all patients undergoing primary PAO at Odense University Hospital (OUH), Denmark. The patients were all operated on in the period from February 1997 to December 2021, which includes the very first patients operated on at OUH. The majority of procedures were performed by 3 surgeons (OO, SO, and MBØ). Before the first surgery we visited other centers with considerable experience and had a very experienced surgeon assisting us with the first procedures.
Indications for PAO
We started out operating on patients with traditional AD and later also patients with CDH and LCPD. AR patients were offered PAO from 2003. In a few cases patients had a combination of AD and AR. Patients with AD were defined as having a reduced center edge (CE) angle and increased acetabular inclination angle (AIA). Patients with AR had retroversion signs on standing pelvic radiographs defined as crossover sign (COS), posterior wall sign, and most often also ischial spine sign but normal or increased CE angle and not a steep roof. These patients with AR had a wedge osteotomy to create flexion of the acetabular fragment. Some patients with AD also had a small COS but not necessitating a wedge osteotomy. In cases with a wedge taken out, the patient was grouped as AR. Patients with CDH and LCPD were all diagnosed in childhood and received treatment, either conservative or surgical (i.e., open reduction, femoral and/or pelvic osteotomy). In the CDH group 27 of 63 had earlier surgery and in the LCPD group 18 of 57. We have gradually tightened up the indications for PAO, especially regarding secondary OA, which contraindicates PAO. If in doubt regarding OA we did an MRI scan. Furthermore, we do not routinely offer PAO to patients older than 45 years or patients with a body mass index (BMI) > 30. We also hesitate to offer PAO to patients who have had chronic pain for years. In patients with atypical symptoms, we perform a preoperative diagnostic block.
Institutional database and the Danish National Patient Registry
Patients were identified from our institutional database on patients undergoing PAO. Data on all patients included: sex, height, weight, BMI, age at surgery, right or left hip, type of underlying hip condition leading to PAO, degree of OA before surgery, and previous surgery on the same hip. Data was prospectively entered by the surgeon before surgery on every patient. In the case of missing preoperative data in the database, patient records were reviewed. Furthermore, all patient records were scrutinized for follow-up data on subsequent operations.
A retrospective patient file survey could only detect subsequent operations performed within the Region of Southern Denmark. To ensure complete follow-up on reoperation with THA, data was achieved from the Danish National Patient Registry (DNPR) via Statistics Denmark on procedure code level. The DNPR is a national registry containing patient admissions and surgical procedures on all patients at Danish hospitals (15) (Figure 1).
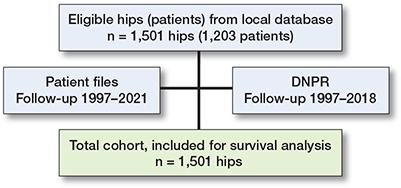
Figure 1. Study cohort. Flowchart showing inclusions and follow-up from patient files with full follow-up from 1997 to 2021 and follow-up from the Danish National Patient Registry (DNPR) from 1997 to 2018. A total of 1,501 hips were included in this study.
Outcomes
The primary outcome was long-term hip survival rate after PAO in AD, AR, CDH, and LCPD patients using THA as primary endpoint at up to 24 years’ follow-up. When reporting survival time for the individual indications this is done at 15 years to make them comparable, as AR and CDH have shorter follow-up. Risk factors for conversion to THA was also analyzed as part of the primary outcome. The risk factors included were sex, age, BMI, Tönnis arthritis grade, year of index operation, and underlying hip condition, as other studies found increased risk with increasing age and Tönnis arthritis grade (6,7,12,16,17).
The secondary outcome was to report subsequent reoperations other than THA. All operations in the same anatomical hip region were registered from patient files. Data is presented as (i) all subsequent operations in the same anatomical region other than THA (n total), (ii) all subsequent operations potentially related to PAO surgery (risk estimate [%], only 1 per patient).
Statistics
Categorical data is presented as numbers with percentages, normally distributed data is displayed as means (range), non-normally distributed data is given as medians with interquartile ranges (IQR). Survival rates will be assessed using Kaplan–Meier analysis with THA as endpoint. Risk factors will be assessed in a Cox regression model to calculate hazard rate ratios and 95% confidence intervals (CI). The model assumption of proportional hazards was assessed with the use of the Schoenfeld residuals test. Patients who emigrated (n = 7) or died (n = 15) were censored at the time of migration and/or death; this data was collected from the DNPR. If patients were bilaterally operated, both hips were included and analyzed as separate observations (18).
All statistical analyses were performed using STATA/IC, version 17 (StataCorp LLC, College Station, TX, USA). For all risk estimates a 95% CI was estimated.
Ethics, funding, and disclosures
Data processing and storage is registered in the Region of Southern Denmark record of data-processing activities. The right to access data in accordance with the Danish Health Act was applied for from the Region of Southern Denmark. The Region of Southern Denmark approved permission to access patient files without informed consent (case no. 21/47010 and 21/42892). All data was processed and stored in compliance with the EU General Data Protection Regulation (GDPR) and the Danish Data Protection Act.
This study received funding from The OUH Fund for Pregraduate Stipends—“OUHs Prægraduatpulje,” to cover salary for ARK and from the Local Tissue Bank (Knoglebanken) to cover expenses for data extraction from the DNPR. The authors have no conflicts of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.12403
Results
Demographics
1,501 hips in 1,203 patients were eligible and included in this study. The following diagnoses lead to PAO: AD (n = 891), AR (n = 490), CDH (n = 63), and LCPD (n = 57). Mean patient age at time of operation was 29 years (SD 11) and the ratio of male to female was 1:3. Patient demographic and preoperative data are presented in Table 1.
| Factor | Overall | AD | AR | CDH | LCPD |
| Hips (% of total) | 1,501 | 891 (59) | 490 (33) | 63 (4) | 57 (4) |
| Age at operation | |||||
| mean (SD) | 29.7 (11) | 33.4 (11) | 23.8 (8.0) | 26.6 (11) | 25.4 (9.6) |
| range | 11–63 | 11–63 | 13–55 | 12–53 | 14 – 51 |
| Female sex | 1,155 (77) | 706 (79) | 370 (76) | 57 (90) | 22 (39) |
| Body mass index | |||||
| mean (SD) | 24.5 (4.0) | 24.9 (4.2) | 23.8 (3.7) | 24.2 (4.0) | 25.3 (4.3) |
| range | 15.4–42.9 | 15.6–42.9 | 16.4–35.5 | 15.4–35.9 | 17.2–37.2 |
| missing | 12 (0.8) | 7 (0.8) | 1 (0.2) | 2 | 2 |
| ASA score | |||||
| 1 | 1,076 (72) | 594 (67) | 407 (83) | 40 | 35 |
| 2 | 294 (20) | 195 (22) | 80 (16) | 9 | 10 |
| 3 | 6 (0.4) | 5 (0.6) | 0 | 1 | 0 |
| missing | 125 (8) | 97 (11) | 3 (0.6) | 13 | 12 |
| Side of operation | |||||
| right | 829 (55) | 500 (56) | 260 (53) | 30 | 39 |
| left | 672 (45) | 391 (44) | 230 (47) | 33 | 18 |
| Previous surgery on the same hip a | 92 (6) | 29 (3) | 18 (4) | 27 | 18 |
| Tönnis arthritis grade | |||||
| 0 | 1,412 (94) | 829 (93) | 484 (99) | 48 | 51 |
| 1 | 83 (6) | 56 (6) | 6 (1) | 15 | 6 |
| 2 | 5 (0.3) | 5 (0.6) | 0 | 0 | 0 |
| 3 | 1 (0.1) | 1 (0.1) | 0 | 0 | 0 |
| Concurrent surgery on the same hip (femur) | |||||
| none | 1,428 (95) | 864 (97) | 485 (99) | 52 | 27 |
| osteotomy | 46 (3) | 12 (1) | 0 | 8 | 26 |
| resection of bone | 3 (0.2) | 1 (0.1) | 2 (0.4) | 0 | 0 |
| curettage of cyst | 1 (0.1) | 0 | 0 | 0 | 1 |
| other b | 32 (2) | 20 (2) | 4 (1) | 4 | 4 |
| a Previous surgery: acetabular osteotomies, femoral osteotomies, hip arthroscopies, open/closed reposition and other. b Other: arthrotomy, psoas tenotomy, cheilectomy, trochanter distalization, removal of osteosynthesis material. AD, acetabular dysplasia; AR, acetabular retroversion; CDH, congenital dislocation of the hip; LCPD, Legg-Calve-Perthes disease. |
|||||
Hip survival
In the study period, 123 (8.2%) of the 1,501 hips were converted to THA. The mean time from index surgery to THA was 7 years (range 0.7–19.5). The mean follow-up time was 7.6 years (range 0.02–24.6).
The Kaplan–Meier analysis with THA defined as endpoint showed a cumulative hip survival rate of 71% (CI 61–79) at 24 years for the entire cohort. The overall hip survival rate at 5-, 10-, and 15-years was 96% (CI 94–97), 91% (CI 88–92), and 82% (CI 77–85), respectively (Figure 2).
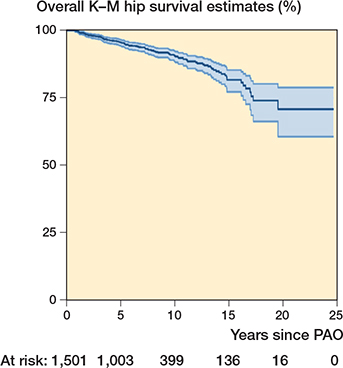
Figure 2. Kaplan–Meier survivorship curve (with 95% CI) after periacetabular osteotomy in 1,501 hips (1,479 hips at risk after censoring) with total hip arthroplasty (THA) as endpoint. Each conversion to THA is seen as a decrease on the curve. The hip survival rate is 71% (CI 61–79) at 24 years.
Of the 891 hips with AD, 81 hips (9.1%) later underwent THA. The individual Kaplan–Meier hip survival rate for AD was 81% (CI 76–86) at 15 years and 70% (CI 60–79) at 20 years. In the AR group 20/490 hips (4.1%) were converted to THA. The Kaplan–Meier hip survival rate for AR was 94% (CI 91–96) at 15 years. In the CDH group of 63 hips, 7 hips underwent THA. The Kaplan–Meier hip survival rate was 84% (CI 66–93) at 15 years and 75% (CI 50–89) at 20 years. Of the 57 hips with LCPD, 15 hips underwent THA. The Kaplan–Meier hip survival rate for LCPD at 15 years was 66% (CI 49–79) (Figure 3).
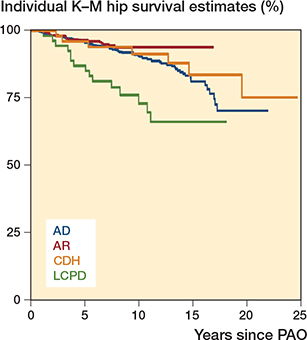
Figure 3. Kaplan–Meier survivorship curve for the 4 individual indications with total hip arthroplasty as endpoint. Each conversion to total hip arthroplasty is seen as a decrease on the curve. AD, acetabular dysplasia; AR, acetabular retroversion; CDH, congenital dislocation of the hip; LCPD, Legg-Calvé-Perthes disease.
Risk factors
The hazard ratio for risk factors associated with conversion to THA are presented in Table 2. The significant risk factors for conversion to THA were age group 30–44 years (HR 1.7, CI 1.1–2.8) age group ≥ 45 years (HR 2.2, CI 1.2–3.8), patients with a Tönnis arthritis grade of 1 or more (HR 3.5, CI 2.2–5.6), and patients diagnosed with LCPD (HR 2.7, CI 1.5–5.0).
Reoperations
The risk of reoperations other than THA (only 1 per hip and only the first reoperation) was 47.8% and is presented in detail in Table 3. 107 hips had more than 1 subsequent surgery. Screw removal was the most common subsequent procedure accounting for 92% of the subsequent surgeries.
| Indication | Total reoperations | Removal of osteosynthesis material | Arthroscopy | Re-PAO | Other |
| Total (n = 1,501) | 715 (48) | 656 (44) | 6 (0.4) | 6 (0.4) | 12 (0.8) |
| AD (n = 891) | 435 (49) | 395 (44) | 2 (0.2) | 3 (0.3) | 7 (0.8) |
| AR (n = 490) | 222 (45) | 210 (43) | 3 (0.6) | 3 (0.6) | 3 (0.6) |
| CDH (n = 63) | 27 | 25 | 1 | 0 | 0 |
| LCPD (n = 57) | 31 | 26 | 1 | 0 | 0 |
For Abbreviations, see Table 1. |
|||||
807 subsequent operations were performed in the entire cohort (including multiple subsequent operations per hip) (Table 4, see Appendix).
Of the 123 hips that were converted to THA, 76 hips (62%) had an additional surgery prior to the THA.
Discussion
We found that PAO preserves 71% (CI 61–79) of hips at 24 years. The risk of conversion to THA increased with age at time of PAO, but also a Tönnis arthritis grade of 1 or more and LCPD was associated with increased risk of THA. The individual Kaplan–Meier rates showed a statistically significant higher hip survival rate for AR patients compared with AD patients. We also found that the risk of reoperations other than THA after PAO was 48%, of which removal of osteosynthesis material accounted for 92% of the interventions.
Overall survival
The overall hip survival rate at 15 years was 82% (CI 77–85). In comparison and very close to our results at 15 years, Larsen et al. (6) reported a 14-year hip survival rate in AD patients of 80%. However, they excluded their first PAO procedures, which in comparison with our results may have improved their survival rate as a potential learning curve was omitted from the analysis. Moreover, Wells et al. (8) reported a slightly higher survival rate of 92% at 15 years in patients with DDH. An explanation could be a smaller cohort of only 154 hips and with 22 hips (13%) lost to follow-up. Another study by Wells et al. (7) reported a survival rate of 74% at 18 years after PAO performed in 121 hips with AD or CDH, which is an accordance with our 20-year survival rate at 71%.
Lerch et al. (16) reported a 30-year survival rate of 43% in 67 hips including learning curve. This is to our knowledge the longest follow-up on hip survival after PAO, though with a small cohort. More long-term studies should be done in larger cohorts especially, when considering the young patient group and resulting long life perspective.
Survival after PAO depending on hip condition
Our survival analysis showed a statistically significant better survival at 15 years in patients with AR at 94% (CI 91–96) compared with AD at 81% (CI 76–86). Only 1 previous study compared the outcome after PAO for AR with AD and found similar better survival in the AR group but in a much smaller cohort (n = 62) and with short follow-up of 3.5 years (19). Two other studies found 10-year survival of AR patients undergoing PAO of 79% (10) and 100% (9) but in very small cohorts (n = 67 and n = 29 hips respectively).
Our patients with CDH had a hip survival of 84% (CI 66–93) at 15 years comparable to that of the AD group. The 20- and 24-year survival was 75% (CI 50–89), which has not been reported earlier.
Our patients with LCPD had a slightly inferior hip survival rate of 66% (CI 49–79) at 15 years compared with AD; however, the difference was not statistically significant. The 5- and 10-year survival rate was 87% and 73%, respectively. This is not surprising as some of the patients did not have a congruent joint. In the later period very few patients with LCPD were operated on. Our result corresponds to data from Albers et al. (12), who reported a 5-year survival rate of 86% and an 8-year survival rate at 61% in 53 hips.
Risk factors
We found that increasing age was associated with higher risk of conversion to THA. Other studies have also reported on higher age leading to higher risk of THA (5-7,12,16,17). We also found that a Tönnis arthritis grade of 1 or more leads to a significantly higher risk of conversion to THA (HR 3.5, CI 2.2–5.6). This also corresponds well with the literature (5,12,16,17). The above-mentioned risk factors support thorough consideration of indications, especially in patients aged above 30 years and when arthritis is present. Patients diagnosed with LCPD also had a higher risk of conversion to THA after PAO (HR 2.7, CI 1.5–5.0). They often have complex hip deformities and have inferior hip survival compared with AD, but further studies on larger cohorts are needed to report the outcome after PAO.
Reoperations
Following PAO, we found a total risk of reoperations other than THA of 48%. Removal of osteosynthesis material was most frequent (44%) accounting for 92% of cases, which is higher than reported earlier (6,20). Conversely, we found that the frequency of subsequent hip arthroscopy was 0.4%, which is less than the 11% reported by Larsen et al. (6). Most likely, these differences may be explained by differences in indications and traditions between centers. In our center we have been generous regarding removal of the screws if the patient had complaints from the iliac crest, especially in slim patients. An extra-osseous part of a screw may interfere with the iliopsoas muscle and cause pain, and hence we had a low threshold for screw removal. Whether this approach is the right one cannot be confirmed or rejected in this study without functional data.
Strengths and limitations
The strength of this study is the inclusion of different indications; AD, AR, CDH, and LCPD and the outcomes after PAO are presented accordingly. Also, we report data on the largest consecutive cohort so far (1,501 hips) and we also included initial procedures during a potential learning curve. We also report data with a long follow-up period (24 years) compared with previous studies (21).
Finally, a strength of this study is not relying on procedure and diagnostic codes alone in the index population but using prospectively collected data and review of patient records for specific data. This ensures identification of indications for surgery and specific complications postoperatively. The follow-up is enhanced by supplementary data from the DNPR (15), which is a high-quality nationwide register, on all readmissions in Denmark.
The study is limited to reporting on risk of later THA surgery and reoperations. We do not address patient safety (readmissions and in-hospital complications), functional outcomes, and/or patient-reported outcome measures. Also, this study does not include data on the quality of correction after surgery, which might have affected the outcomes.
Data from Statistics Denmark was based solely on procedure and diagnosis codes and not on evaluation of patient files. Hence, this data may include coding errors. Furthermore, data from Statistics Denmark (LPR2) is only available in the period from 1997 to 2018; however, it is not very likely that the patients from 2018 to 2021 are converted to THA in a 3-year period or less. Another limitation is that we may not have complete follow-up from Statistics Denmark regarding subsequent hip-related operations other than THA. Hence, we have registered only those reoperated on in our own region. We do, however, expect that most patients were reoperated on at the same institution as they had their index surgery.
Conclusion
71% of hips were preserved at 24 years after PAO. AR patients had the highest (94%) PAO survivorship at 15 years compared with the other underlying hip conditions. At age ≥ 30, a Tönnis arthritis grade of 1 or more and LCPD diagnosis was associated with increased risk of conversion to THA after PAO. Almost half of PAO patients may undergo other additional surgery with later screw removal as the primary reason, which is information relevant to both patients and surgeons.
- Ganz R, Klaue K, Vinh T S, Mast J W. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res 1988; (232): 26-36. PMID: 3383491.
- Ganz R, Leunig M, Leunig-Ganz K, Harris W H. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008; 466(2): 264-72. doi: 10.1007/s11999-007-0060-z.
- Harris W H. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res 1986; (213): 20-33. PMID: 3780093.
- Giori N J, Trousdale R T. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res 2003; (417): 263-9. doi: 10.1097/01.blo.0000093014.90435.64.
- Matheney T, Kim Y J, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am 2009; 91(9): 2113-23. doi: 10.2106/jbjs.g.00143.
- Larsen J B, Mechlenburg I, Jakobsen S S, Thilleman T M, Søballe K. 14-year hip survivorship after periacetabular osteotomy: a follow-up study on 1,385 hips. Acta Orthop 2020; 91(3): 299-305. doi: 10.1080/17453674.2020.1731159.
- Wells J, Millis M, Kim Y J, Bulat E, Miller P, Matheney T. Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res 2017; 475(2): 396-405. doi: 10.1007/s11999-016-4887-z.
- Wells J, Schoenecker P, Duncan S, Goss C W, Thomason K, Clohisy J C. Intermediate-term hip survivorship and patient-reported outcomes of periacetabular osteotomy: the Washington University Experience. J Bone Joint Surg Am 2018; 100(3): 218-25. doi: 10.2106/jbjs.17.00337.
- Siebenrock K A, Steppacher S D, Tannast M, Büchler L. Anteverting periacetabular osteotomy for acetabular retroversion. JBJS Essent Surg Tech 2015; 5(1): e1. doi: 10.2106/jbjs.m.00842.
- Zurmühle C A, Anwander H, Albers C E, Hanke M S, Steppacher S D, Siebenrock K A, et al. Periacetabular osteotomy provides higher survivorship than rim trimming for acetabular retroversion. Clin Orthop Relat Res 2017; 475(4): 1138-50. doi: 10.1007/s11999-016-5177-5.
- Shinoda T, Naito M, Nakamura Y, Kiyama T. Periacetabular osteotomy for the treatment of dysplastic hip with Perthes-like deformities. Int Orthop 2009; 33(1): 71-5. doi: 10.1007/s00264-007-0476-9.
- Albers C E, Steppacher S D, Ganz R, Siebenrock K A, Tannast M. Joint-preserving surgery improves pain, range of motion, and abductor strength after Legg-Calvé-Perthes disease. Clin Orthop Relat Res 2012; 470(9): 2450-61. doi: 10.1007/s11999-012-2345-0.
- Clohisy J C, Nepple J J, Ross J R, Pashos G, Schoenecker P L. Does surgical hip dislocation and periacetabular osteotomy improve pain in patients with Perthes-like deformities and acetabular dysplasia? Clin Orthop Relat Res 2015; 473(4): 1370-7. doi: 10.1007/s11999-014-4115-7.
- von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147(8): 573-7. doi: 10.7326/0003-4819-147-8-200710160-00010.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sørensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7:449-90. doi: 10.2147/clep.s91125.
- Lerch T D, Steppacher S D, Liechti E F, Tannast M, Siebenrock K A. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2017; 475(4): 1154-68. doi: 10.1007/s11999-016-5169-5.
- Hartig-Andreasen C, Troelsen A, Thillemann T M, Søballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res 2012; 470(11): 2978-87. doi: 10.1007/s11999-012-2386-4.
- Lie S A, Engesaeter L B, Havelin L I, Gjessing H K, Vollset S E. Dependency issues in survival analyses of 55,782 primary hip replacements from 47,355 patients. Stat Med 2004; 23(20): 3227-40. doi: 10.1002/sim.1905.
- Verhaegen J, Salih S, Thiagarajah S, Grammatopoulos G, Witt J D. Is a periacetabular osteotomy as efficacious in retroversion as it is in dysplasia?: The role of femoral anteversion on outcome. Bone Joint Open 2021; 2(9): 757-64. doi: 10.1302/2633-1462.29.bjo-2021-0096.r2.
- Bræmer C N, Langberg S A, Jakobsen S S, Jakobsen S R, Aleixo H, Søballe K, et al. Does pain and hip function improve 2 years after reverse periacetabular osteotomy? A follow-up study of 74 patients. J Hip Preserv Surg 2020; 7(1): 130-9. doi: 10.1093/jhps/hnz066.
- Sohatee M A, Ali M, Khanduja V, Malviya A. Does hip preservation surgery prevent arthroplasty? Quantifying the rate of conversion to arthroplasty following hip preservation surgery. J Hip Preserv Surg 2020; 7(2): 168-82. doi: 10.1093/jhps/hnaa022.
Appendix
| Indication / Reoperatios |
| Total (n = 1,501) |
| Reoperations: 807 |
| – Osteosynthesis material removal: 699 |
| – Arthroscopy: 59 |
| – Re-PAO: 17 |
| – Other: 32 |
| AD (n = 891) |
| Reoperations: 486 |
| – Osteosynthesis material removal: 423 |
| – Arthroscopy: 33 |
| – Re-PAO: 10 |
| – Other: 20 |
|
| AR (n = 490) |
| Reoperations: 257 |
| – Osteosynthesis material removal: 220 |
| – Arthroscopy: 24 |
| – Re-PAO: 6 |
| – Other: 7 |
|
| CDH (n = 63) |
| Reoperations: 32 |
| – Osteosynthesis material removal: 26 |
| – Arthroscopy: 2 |
| – Re-PAO: 1 |
| – Other: 3 |
|
| LCPD (n = 57) |
| Reoperations: 32 |
| – Osteosynthesis material removal: 30 |
| – Arthroscopy: 0 |
| – Re-PAO: 0 |
| – Other: 2 |
|
| For Abbreviations, see Table 1. |