10-year evolution of day-case hip and knee arthroplasty: a Danish nationwide register study of 166,833 procedures from 2010 to 2020
Christian Bredgaard JENSEN 1, Anders TROELSEN 1, Nicolai Bang FOSS 2, Christian Skovgaard NIELSEN 1, Martin LINDBERG-LARSEN 3, and Kirill GROMOV 1
1 Department of Orthopaedic Surgery, Clinical Orthopaedic Surgery Hvidovre (CORH), Copenhagen University Hospital Hvidovre, Hvidovre; 2 Department of Anaesthesiology, Copenhagen University Hospital Hvidovre, Hvidovre; 3 Department of Orthopaedic Surgery, Orthopaedic Research Unit (ORU), Odense University Hospital, Odense, Denmark
Background and purpose — No previous studies have investigated the use of day-case arthroplasty in Denmark on a national scale. We investigated the frequency of day-case surgery in total hip (THA), total knee (TKA), and unicompartmental knee arthroplasty (UKA) from 2010 to 2020 in Denmark.
Patients and methods — Primary unilateral THAs, TKAs, and UKAs performed for osteoarthritis were identified in the Danish National Patient Register using procedural and diagnosis codes. Day-case surgery was defined as discharge on the day of surgery. 90-day readmissions were defined as any overnight admissions following discharge.
Results — From 2010 to 2020 Danish surgical centers performed 86,070 THAs, 70,323 TKAs, and 10,440 UKAs. From 2010 to 2014, less than 0.5% of THAs and TKAs were day-case procedures. They increased to 5.4% (95% confidence interval [CI] 4.9–5.8) of THAs and 2.8% (CI 2.4–3.2) of TKAs in 2019. From 2010 to 2014, 11% of UKAs were day-case procedures, but they increased to 20% (CI 18–22) in 2019. This increase was driven by a few surgical centers (3–7 centers). In 2010, readmission rates within 90 days of surgery were 10% after THAs and 11% after TKAs, and 9.4% for both THAs and TKAs in 2019. Readmission rates after UKA fluctuated between 4% and 7%.
Conclusion — From 2010 to 2020 the use of day-case surgery in THA, TKA, and UKA increased in Denmark, driven by only a few centers. During the same period readmissions did not increase.
Citation: Acta Orthopaedica 2023; 94: 178–184. DOI https://doi.org/10.2340/17453674.2023.11961.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-10-14. Accepted: 2023-03-13. Published: 2023-04-18.
Correspondence: christian.bredgaard.jensen@regionh.dk
CBJ and KG had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: CBJ, AT, and KG. Acquisition, analysis, and interpretation of data: all authors. Drafting of the manuscript: CBJ and KG. Critical revision of the manuscript for important intellectual content: all authors.
Handling co-editors: Bart Swierstra and Philippe Wagner
Acta thanks Michael Clarius and Stephan Vehmeijer for help with peer review of this study.
The perioperative setup of arthroplasty for hip and knee osteoarthritis (OA) has undergone multiple changes as a result of increased use of rapid recovery protocols (1). Reductions in length of stay, postoperative morbidity, and costs associated with hip and knee arthroplasty have been demonstrated over time (2,3). However, challenges in nationwide implementation of rapid recovery protocols remain (1).
As the demand for arthroplasties is projected to increase due to an increasingly morbid and ageing population, further optimizing length of stay without compromising safety following hip and knee arthroplasty remains an objective. Therefore, day-case arthroplasty surgery has been a topic of increasing interest for orthopedic researchers and healthcare providers. Multiple studies have demonstrated that day-case hip and knee arthroplasty is feasible and safe in selected patients, while also offering a cost reduction (3).
Varying reports of national use of day-case surgery are present. A study from the United Kingdom found that between 2018 and 2019 only 0.55% of total hip arthroplasty (THA) and 0.52% of total knee arthroplasty (TKA) were day-case procedures (4). In the United States (US) an increase in day-case use from 1.9% to 4.7% in TKA from 2010 to 2017 was reported (5).
Investigations from 2 public Danish surgical centers demonstrated that, given certain criteria for day-case eligibility, 54% of THA and TKA patients were eligible for day-case surgery, with day-case being successful in 15% of unselected THA and TKA patients (6,7). However, demonstrating the usefulness and feasibility of day-case surgery in published literature does not equal implementation in widespread clinical settings.
We investigated the frequency of day-case surgery in THA, TKA, and unicompartmental knee arthroplasty (UKA) from 2010 to 2020 in Denmark. Furthermore, we investigated the preoperative comorbidity, length of stay, and readmission and mortality rates during the same period.
Patients and methods
Our study was designed as a descriptive cohort study based on prospectively collected register data from the Danish National Patient Register (DNPR). The reporting of this study complies with the REporting of studies Conducted using Observational Routinely-collected Data (RECORD) statement.
Data sources
Data on patient demographics, surgical procedures, diagnostic codes related to hospital contacts, and hospitals was received from the DNPR. The DNPR is a nationwide administrative register containing information on all treatments and examinations performed in Danish hospitals. The DNPR has a completeness of > 99% (8), as all Danish healthcare facilities are required to report to the DNPR. Codes used in the DNPR are based on surgical procedure codes from the Nordic Medico-Statistical Committee (NOMESCO) classification of surgical procedures (NCSP) (9) and diagnostic codes from the International Classification of Diseases and Related Health Problems 10th Revision (ICD-10).
Data on mortality was supplied by the Danish Civil Registration System (CPR) register. Cases of mortality were linked to procedures in the DNPR using the civil registration number, a personal identification number required for all residents of Denmark.
Study population
All primary THA (NFB20, NFB30, NFB40), TKA (NGB20, NGB30, NGB40), or UKA procedures (NGB01, NGB02, NGB11, NGB12) registered in the DNPR between January 2010 and February 2020 were identified. Procedures were primarily performed at public surgical centers, but also in privately funded surgical centers. Procedures performed after February 2020 were not included due to changes in hospital standard operating procedures due to COVID-19 restrictions implemented in Denmark in March 2020.
Simultaneous bilateral procedures in DNPR identified as 2 procedures on the same patient performed on the same date but coded as right and left side or 1 procedure coded as both right and left side, were excluded. Procedures not coded with hip (M16n) or knee OA (M17n) as the primary diagnosis were also excluded (Figure 1).
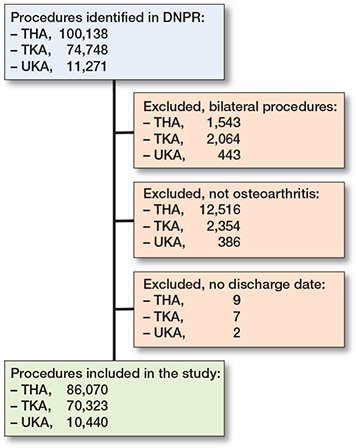
Figure 1. Flowchart for study. THA = total hip arthroplasty; TKA = total knee arthroplasty; UKA = unicompartmental knee arthroplasty; Not osteoarthritis includes surgical indications such as inflammatory arthritis, fractures, and tumors.
Data on age and sex was supplied by the DNPR. Preoperative comorbidity was evaluated using the Charlson Comorbidity Index based on ICD-10 codes from the DNPR from 10 years prior to the arthroplasty surgery (10,11).
Outcome measures
Day-case surgery was defined as discharge recorded on the same date as the surgery. Length of stay (LOS) was defined as the number of nights admitted following surgery. Admissions within 4 hours of discharge were coupled to the index admission and LOS is calculated as the total nights of the coupled admittances (12). Utilization of day-case surgery was evaluated in public non-low-volume surgical centers for each of the different arthroplasty procedures. Non-low-volume public surgical centers were defined as ≥ 100 THAs/TKAs each (13) or ≥ 52 UKAs each year (14). Readmission within 90 days of surgery was defined as any admissions with LOS > 1 day in a Danish hospital at least 4 hours after discharge from index admission. Mortality within 90 days of surgery was based on deaths recorded in the CPR register. In the case of mortality before or on the date of discharge the case (n = 63) was excluded from analysis of LOS and readmissions.
Statistics
Q–q plots and histograms were used to evaluate normality of data. Normally distributed data was presented as mean and standard deviations (SD) and non-normally distributed data was presented as median and interquartile range (IQR). Percentages are presented with 95% confidence intervals (CI). Outliers within LOS were evaluated using boxplots (defined as > 95 percentile) and were excluded from descriptions of LOS and readmission. 63 cases of mortality prior to discharge and 5 outliers with LOS > 100 days were excluded from the following descriptive analyses of LOS and readmission. Comparison of readmission rates in each arthroplasty group between the time periods 2010–2013, 2014–2017, and 2018–2020 was done using logistic regression adjusted for age, sex, and CCI score. Adjusting variables were chosen based on previous studies associating these patient characteristics with increased risk of readmission (15). A similar but unadjusted analysis for mortality risk was conducted, due to the rare occurrence of mortality. The overall fit of the logistic regression models was evaluated using binned residual plots of average residuals within bins. Multicollinearity between variables included in the regression models was evaluated using variance inflation factors (VIF). Variables with a VIF > 5 were not included in the adjusted model, as this was considered indicative of collinearity. For logistic regression models an odds ratio (OR) and CI was presented. Statistical analyses were conducted in R-studio with R v. 3.6.1 and ggplot2 (v. 3.3.5) (R Foundation for Statistical Computing, Vienna, Austria).
Ethics, funding, and disclosures
The Knowledge Center on Data Protection Compliance in the Capital Region of Denmark approved this study (approval nr. P-2021-132). As this was an observational study with no clinical intervention and using only register data, no approval from regional or national research ethical committees was required and informed consent was waived. No funding was received directly for this study. CBJ has received ph.d. funding from a grant from the Novo Nordisk Foundation unrelated to this study. KG and AT has received research support and speaker fees from Zimmer Biomet, and AT has received research support from Pfizer. NBF has received speaker fees from Masimo Cooperation and Edwards Lifesciences. All of the above conflicts are unrelated to this study.Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.11961
Results
Study population
From January 2010 to February 2020 Danish surgical centers performed 86,070 THAs, 70,323 TKAs, and 10,440 UKAs unilaterally as treatment for hip and knee OA (Figure 1). Patient demographics are reported in Table 1. THA and TKA patients were older and more comorbid than UKA patients.
| Type of surgery | |||
| Factor | THA | TKA | UKA |
| Count, n | 86,070 | 70,323 | 10,440 |
| Age, mean (SD) | 68.5 (11) | 68.2 (9.6) | 65.3 (9.6) |
| Female sex | 48,341 (56) | 41,732 (59) | 5,493 (52) |
| Public surgical center | 81,171 (94) | 65,318 (93) | 9,812 (94) |
| Charlson Comorbidity Index score | |||
| 0 | 59,782 (70) | 47,530 (68) | 7,493 (72) |
| 1 | 12,118 (14) | 11,055 (16) | 1,465 (14) |
| 2 | 9,724 (11) | 8,071 (12) | 1,052 (10) |
| > 2 | 4,446 (5) | 3,667 (5) | 430 (4) |
| Year of surgery, n | |||
| 2010 | 7,836 | 7,265 | 630 |
| 2011 | 7,804 | 6,740 | 681 |
| 2012 | 7,644 | 7,042 | 636 |
| 2013 | 7,779 | 6,945 | 649 |
| 2014 | 8,222 | 7,123 | 730 |
| 2015 | 8,509 | 6,701 | 1,033 |
| 2016 | 9,027 | 6,347 | 1,234 |
| 2017 | 8,680 | 5,760 | 1,272 |
| 2018 | 9,200 | 6,928 | 1,337 |
| 2019 | 9,535 | 7,757 | 1,854 |
| 2020a | 1,834 | 1,494 | 384 |
| a Year 2020 includes data only from January and February. SD = standard deviation. | |||
The number of THAs performed increased from 7,836 in 2010 to 9,535 in 2019 (22% increase). The number of knee arthroplasties increased from 7,895 in 2010 to 9,611 (22% increase). UKAs constituted 8.0% (n = 630) of knee arthroplasties in 2010 and 19% (n = 1,854) of knee arthroplasties in 2019.
The overall LOS, DOS discharge, 90-day readmission rate, and 90-day mortality rate are presented in Table 2.
| Factor | Type of surgery | ||
| THA | TKA | UKA | |
| Count | 86,070 | 70,323 | 10,440 |
| LOS (days)a | |||
| mean (SD) | 2.3 (1.9) | 2.6 (1.8) | 1.3 (1.1) |
| median (IQR) | 2 (1–3) | 2 (2–3) | 1 (1–2) |
| Day-case procedures | 1,606 (1.9) | 654 (0.9) | 1,763 (17) |
| 90-day readmissiona | 8,132 (9.5) | 6,497 (9.2) | 624 (6.0) |
| 90-day mortality | 298 (0.35) | 178 (0.25) | 10 (0.10) |
| LOS = length of stay; SD = standard deviation; IQR = interquartile range. | |||
| a Excluding 68 cases due to mortality occurring before discharge or outliers in LOS. | |||
Day-case surgery and its use in public surgical centers
The use of day-case surgery increased from 2010 to 2020 in hip and knee arthroplasties (Figure 2A). In UKAs, day-case surgery remained around 11% from 2010 to 2014. This increased to 20% (CI 18–22) in 2019 and 23% (CI 19–27) in the first months of 2020. In THAs, day-case surgery remained below 0.8% from 2010 to 2014. This increased to 5.4% (CI 4.9–5.8) in 2019 and 7.1% (CI 5.9–8.2) in the first months of 2020. In TKAs, day-case surgery remained below 0.8% from 2010 to 2018. This increased to 2.8% (CI 2.4–3.2) in 2019 and 4.2% (CI 3.2–5.2) in the first months of 2020.
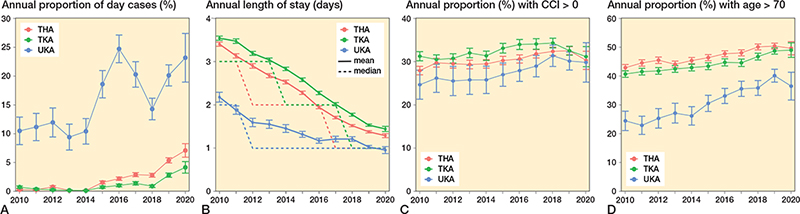
Figure 2. A: The use of day-case surgery sorted for THA, TKA, and UKA as a percentage of total number of performed procedures each year. B: The mean (solid lines) and median (dotted line) length of stay of THA, TKA, and UKA each year. C: The percentage of patients with a CCI score > 0 for THA, TKA, and UKA each year. D: The percentage of patients aged > 70 years for THA, TKA, and UKA each year. Error bars represent 95% confidence intervals of percentages (A, C, D) or mean length of stay (B). CCI = Charlson Comorbidity Index; THA = total hip arthroplasty; TKA = total knee arthroplasty; UKA = unicompartmental knee arthroplasty.
The use of day-case surgery in public non-low-volume surgical centers is presented in Figures 3–5 (see Appendix). In THA and TKA, day-case surgery among the centers increased from 2015. This increase was, however, driven by a small number of centers, as 7/21 THA centers and 2/18 TKA centers performed > 5% day-case procedures in 2019. Most UKA centers appeared to have a developed a systematic use of day-case surgery from 2010 to 2019. However, major differences in the use of day-case surgery between the UKA centers was still present in 2019.
Length of stay, comorbidity, 90-day readmission and mortality rate
LOS decreased from a median of 3 days (IQR 2–4) for THA, 3 days (IQR 3–4) for TKA, and 2 days (IQR 1–3) for UKA in 2010, towards a median 1 day (IQR 1–1) for THA, 1 day (IQR 1–2) for TKA, and 1 day (IQR 1–1) for UKA in 2019 (Figure 2B).
All 3 arthroplasty populations had an increase in the proportion of patients with a CCI score > 0 and age > 70 years (Figure 2C and D). UKAs had the largest increase in patients > 70 years (24% [CI 21–28] in 2010 and 40% [CI 38–42] in 2019).
Readmissions within 90 days of THA and TKA decreased from 10% (CI 9.3–11) and 11% (CI 10–12) in 2010 to 9.4% (CI 8.8–9.9) and 9.4% (CI 8.7–10) in 2019, respectively (Figure 2D). THA and TKA patients treated in 2018–2020 were significantly less likely to be readmitted compared with those treated in 2010–2013 (Table 3, Figure 6). Mortality within 90 days of THAs and TKAs showed a reduction from 0.45% (CI 0.30–0.59) and 0.40% (CI 0.25–0.54) in 2010 to 0.28% (CI 0.18–0.39) and 0.18% (CI 0.09–0.27) in 2019, respectively (Figure 6). Mortality was significantly reduced in THA patients operated on in 2018–2020 compared with 2010–2013 (Table 4). Both readmissions and mortality within 90 days of UKAs have fluctuated between 2010 and 2020 with no clear trend: 90-day readmission between 4% and 7% (Figure 6), and 90-day mortality with cases of mortality only in 2013, 2015, 2016 , and 2017 (Figure 6).
| Type Year | n (%) | 90-day readmissions | |
| Unadjusted OR [CI] | Adjusted a OR [CI] | ||
| Total hip arthroplasty | |||
| 2010–2013 | 3,129 (10) | Reference | Reference |
| 2014–2017 | 3,191 (9.3) | 0.9 [0.9–1.0] b | 0.9 [0.8–0.9] b |
| 2018–2020 | 1,812 (8.8) | 0.9 [0.8–0.9] b | 0.8 [0.8–0.9] b |
| Total knee arthroplasty | |||
| 2010–2013 | 2,815 (10) | Reference | Reference |
| 2014–2017 | 2,262 (8.7) | 0.9 [0.8–0.9] b | 0.8 [0.8–0.9] b |
| 2018-2020 | 1,420 (8.8) | 0.9 [0.8–0.9] b | 0.8 [0.8–0.9] b |
| Unicompartmental knee arthroplasty | |||
| 2010–2013 | 148 (5.7) | Reference | Reference |
| 2014–2017 | 251 (5.8) | 1.0 [0.8–1.3] | 1.0 [0.8–1.2] |
| 2018–2020 | 225 (6.3) | 1.1 [0.9–1.4] | 1.0 [0.8–1.3] |
| a Adjusted for sex, age, and Charlson Comorbidity Index score. | |||
| b Statistically significant. | |||
| OR = odds ratio; CI = 95% confidence interval. | |||
| Type Year | n (%) | 90-day mortality Unadjusted OR [CI] |
| Total hip arthroplasty | ||
| 2010–2013 | 129 (0.42) | Reference |
| 2014–2017 | 110 (0.32) | 0.8 [0.6–1.0] a |
| 2018–2020 | 59 (0.29) | 0.9 [0.5–0.9] a |
| Total knee arthroplasty | ||
| 2010–2013 | 85 (0.32) | Reference |
| 2014–2017 | 68 (0.26) | 0.9 [0.6–1.2] |
| 2018–2020 | 25 (0.15) | 0.7 [0.4–1.1] |
| Unicompartmental knee arthroplasty b | ||
| 2010–2013 | < 5 | |
| 2014–2017 | < 5 | |
| 2018-2020 | < 5 | |
| a Statistically significant. | ||
| b Too few cases of mortality and therefore no regression analyses. | ||
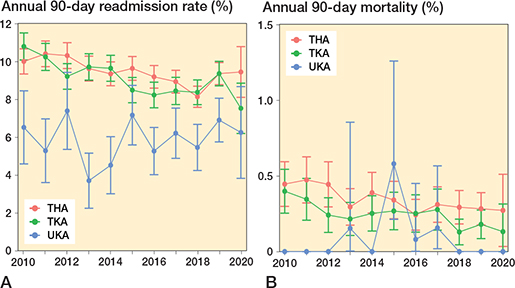
Figure 6 A: 90-day readmission rate for each arthroplasty procedure. B: 90-day mortality rate for each arthroplasty procedure. THA = total hip arthroplasty; TKA = total knee arthroplasty; UKA = unicompartmental knee arthroplasty. Error bars represent 95% confidence intervals of percentages.
Similar trends in DOS discharge, LOS, CCI, age, and readmissions were present in procedures performed in public or private surgical centers (Figures 7 and 8, see Appendix).
Discussion
In this nationwide register study on 166,833 THAs, TKAs and UKAs from 2010 to 2020 we found an increase in use of day-case surgery within all 3 arthroplasty procedures. In 2010 less than 1% of THAs and TKAs were day-case procedures. At the beginning of 2020, prior to the first COVID-19 lockdown, 7.0% of THAs and 4.3% of TKAs were day-case procedures. In 2010, 11% of UKAs were day-case procedures and this increased to 23% at the beginning of 2020. However, the increase in use of day-case THA and TKA appears to be driven by only a few surgical centers. The use of day-case UKA surgery varied greatly between centers, but very few centers had little or no use of day-case surgery. Additionally, from 2010 to 2020 the proportion of hip and knee arthroplasty patients aged > 70 years and with a CCI score > 0 increased, but overall LOS, readmission rates, and mortality rates declined within the same period.
International differences in LOS and use of day-case surgery are present. Only 0.6%, 0.5%, and 5.4% of THAs, TKAs, and UKAs, respectively, were performed as day-case procedures during a period of 1 year from the middle of 2018 to 2019 in the National Healthcare Service (NHS, United Kingdom) (4). While the use of day-case surgery is low compared with our results, this supports our and previously reported findings that UKAs are more likely to be day-case procedures (16). Based on data from the PearlDiver Mariner Database in the USA it was reported that from 2010 to 2017 the use of day-case THA increased from 1.5% to 5.3% and the use of day-case TKA increased from 1.9% to 4.7% (5). Studies reporting the proportion of day-case TKA or THA procedures registered in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) found that 0.6% and 1.8% were day-case procedures between 2005–2014 and 2005– 2018, respectively (17,18). This indicates that similar developments in day-case use have taken place in other countries.
The most dramatic increase in day-case hip and knee arthroplasty surgery occurred between 2018 and 2019. We presume that publications demonstrating that day-case hip and knee arthroplasty is safe and feasible within Danish surgical centers might have caused the change, as shown in our study (6,7). However, studies with similar conclusions have been published internationally without a similar change in practice (19). While the change among Danish surgical centers is large enough to impact the national overall use of day-case surgery, it is primarily driven by few centers performing THA and TKA and with large differences among centers performing UKA. Thus, uniform use of day-case surgery is not yet implemented to a similar degree among all surgical centers in Denmark.
Reductions in LOS over time have previously been reported in multiple studies (20). Based on data from 9 high-volume fast-track surgical centers in Denmark a reduction in LOS from median 3 days in 2010 to median 1 day in 2017 following THA and TKA surgery was reported (2). A reduction from around 3.5 days in 2010 to around 2.3 days in 2017 was reported based on data from ACS-NSQIP (21). However, in the same time period between 15% and 33% of THA and TKA patients operated on in surgical centers reporting to ACSNSQIP were discharged to a non-home destination (21). In comparison, home discharge occurs in 93% of hip and knee arthroplasties in patients ≥ 85 years of age in Denmark (22) and presumably close to 100% in younger patient groups.
The proportion of elderly and comorbid patients increased over time within each arthroplasty type. UKA patients experienced the largest increase in age and comorbidity, potentially as a result of the less restrictive indications for UKA used currently (23). Previous investigations have reported either stable or reduced rates of readmission and mortality, in periods with reductions in LOS and increased comorbidity in the arthroplasty populations (2,24,25). While increased comorbidity has been associated with increased risk of readmission, mortality, and prolonged admission (15), mitigation of these risks has been attributed to adherence to rapid recovery protocols (1,2). Rapid recovery has been implemented and honed within surgical centers in Danish hospitals across 2 decades, and the positive results of rapid recovery appear to continue.
Our study is not without limitations. Our definition of day-case surgery relies on admission and discharge dates from the DNPR. While the DNPR offers complete data on hospital contacts, the dates of admission and discharge are for administrative use and were not further validated by chart review. Also, reliability and validation of diagnostic codes associated with contacts in the DNPR is questionable. For this reason, we report only on compound rates of readmission. Our study shows that an increase in day-case use was not accompanied by an increase in readmission rates. However, a more direct comparison between day-case and overnight stay in comparable patient populations with regards to readmission would be needed to evaluate the effect of day-case surgery on readmissions. To increase comparability in day-case capabilities between centers, we report the use of day-case surgery only on an individual center level in non-low-volume public surgical centers. The definition of a non-low-volume surgical center was based on published literature. The yearly day-case use is summarized across all surgical centers, both privately and publicly funded, and most procedures were performed in public surgical centers. While differences in patient selection and perioperative setup might be present between the 2 types of centers, similar trends in day-case use and patient characteristics were observed.
In conclusion, there was an increase in use of day-case surgery in THAs, TKAs, and UKAs from 2010 to 2020, which appears to be driven by a few surgical centers. In that period, the arthroplasty population was increasingly comorbid and elderly, but rates of readmission and mortality decreased.
- Wainwright T W, Kehlet H. Fast-track hip and knee arthroplasty: have we reached the goal? Acta Orthop 2019; 90(1): 3-5. doi: 10.1080/17453674.2018.1550708.
- Petersen P B, Kehlet H, Jørgensen C C. Improvement in fast-track hip and knee arthroplasty: a prospective multicentre study of 36,935 procedures from 2010 to 2017. Sci Rep 2020; 10(1): 21233. doi: 10.1038/s41598-020-77127-6.
- Bemelmans Y F L, Keulen M H F, Heymans M, van Haaren E H, Boonen B, Schotanus M G M. Safety and efficacy of outpatient hip and knee arthroplasty: a systematic review with meta-analysis. Arch Orthop Trauma Surg 2022; 142(8): 1775-91. doi: 10.1007/S00402-021-03811-5.
- Wainwright T W. The current status of daycase hip and knee arthroplasty within the English National Health Service: a retrospective analysis of hospital episode statistics data. Ann R Coll Surg Engl 2021; 103(5): 324-31. doi: 10.1308/RCSANN.2020.7142.
- Debbi E M, Mosich G M, Bendich I, Kapadia M, Ast M P, Westrich G H. Same-day discharge total hip and knee arthroplasty: trends, complications, and readmission rates. J. Arthroplasty 2022; 37(3): 444-8.e1. doi: 10.1016/J.ARTH.2021.11.023.
- Gromov K, Jørgensen C C, Petersen P B, Kjaersgaard-Andersen P, Revald P, Troelsen A, et al. Complications and readmissions following outpatient total hip and knee arthroplasty: a prospective 2-center study with matched controls. Acta Orthop 2019; 90(3): 281-5. doi: 10.1080/17453674.2019.1577049.
- Gromov K, Kjaersgaard-Andersen P, Revald P, Kehlet H, Husted H. Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop 2017; 88(5): 516-21. doi: 10.1080/17453674.2017.1314158.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449–90. doi: 10.2147/clep.S91125.
- Nordic Medico-Statistical Committee (NOMESCO). NOMESCO Classification of Surgical Procedures (NCSP), version 1.16. Available from: http://norden.diva-portal.org/smash/get/diva2:968721/FULLTEXT01.pdf 2011.
- Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5): 373-83. doi: 10.1016/00219681(87)90171-8.
- Raedkjaer M, Maretty-Kongstad K, Baad-Hansen T, Jørgensen P H, Safwat A, Vedsted P, et al. The impact of comorbidity on mortality in Danish sarcoma patients from 2000–2013: a nationwide population-based multicentre study. PLoS One 2018; 13(6): e0198933. doi: 10.1371/JOURNAL.PONE.0198933.
- Danish Health Data Authority. Afrapportering fra teknikergruppe om opgørelse af indlæggelsesforløb baseret på Landspatientregisteret. https://www.ft.dk/samling/20191/almdel/suu/spm/13/svar/1597313/2088474.pdf.
- Laucis N C, Chowdhury M, Dasgupta A, Bhattacharyya T. Trend toward high-volume hospitals and the influence on complications in knee and hip arthroplasty. J Bone Joint Surg Am 2016; 98(9): 707-12. doi: 10.2106/JBJS.15.00399.
- Henkel C, Mikkelsen M, Pedersen A B, Rasmussen L E, Gromov K, Price A, et al. Medial unicompartmental knee arthroplasty: increasingly uniform patient demographics despite differences in surgical volume and usage—a descriptive study of 8,501 cases from the Danish Knee Arthroplasty Registry. Acta Orthop 2019; 90(4): 354-9. doi: 10.1080/17453674.2019.1601834.
- Podmore B, Hutchings A, Skinner J A, MacGregor A J, Van der Meulen J. Impact of comorbidities on the safety and effectiveness of hip and knee arthroplasty surgery: a national observational study. Bone Joint J 2021; 103(1): 56-64. doi: 10.1302/0301-620X.103B1.BJJ-2020-0859.R1/FORMAT/EPUB.
- Jensen C B, Petersen P B, Jørgensen C C, Kehlet H, Troelsen A, Gromov K. Length of stay and 90-day readmission/complication rates in unicompartmental versus total knee arthroplasty: a propensity-score-matched study of 10,494 procedures performed in a fast-track-setup. J Bone Joint Surg Am 2021; 103(12): 1063-71. doi: 10.2106/jbjs.20.01287.
- Kendall M C, Cohen A D, Principe-Marrero S, Sidhom P, Apruzzese P, De Oliveira G. Spinal versus general anesthesia for patients undergoing outpatient total knee arthroplasty: a national propensity matched analysis of early postoperative outcomes. BMC Anesthesiol 2021; 21(1): 226. doi: 10.1186/S12871-021-01442-2.
- Bovonratwet P, Ondeck N T, Tyagi V, Nelson S J, Rubin L E, Grauer J N. Outpatient and inpatient unicompartmental knee arthroplasty procedures have similar short-term complication profiles. J Arthroplasty 2017; 32(10): 2935-40. doi: 10.1016/j.arth.2017.05.018.
- Bradley B, Middleton S, Davis N, Williams M, Stocker M, Hockings M, et al. Discharge on the day of surgery following unicompartmental knee arthroplasty within the United Kingdom NHS. Bone Joint J 2017; 99-b(6): 788-92. doi: 10.1302/0301-620x.99b6.Bjj-2016-0540.R2.
- Shah A, Memon M, Kay J, Wood T J, Tushinski D M, Khanna V. Preoperative patient factors affecting length of stay following total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2019; 34(9): 2124-65.e1. doi: 10.1016/j.arth.2019.04.048.
- DeMik D E, Carender C N, Glass N A, Callaghan J J, Bedard N A. More patients are being discharged home after total knee arthroplasty, however rates vary between large databases. J Arthroplasty 2021; 36(1): 173-9. doi: 10.1016/J.ARTH.2020.07.059.
- Pitter F T, Jørgensen C C, Lindberg-Larsen M, Kehlet H. Postoperative morbidity and discharge destinations after fast-track hip and knee arthroplasty in patients older than 85 years. Anesth Analg 2016; 122(6): 1807-15. doi: 10.1213/ane.0000000000001190.
- Hamilton T W, Pandit H G, Jenkins C, Mellon S J, Dodd C A F, Murray D W. Evidence-based indications for mobile-bearing unicompartmental knee arthroplasty in a consecutive cohort of thousand knees. J Arthroplasty 2017; 32(6): 1779-85. doi: 10.1016/j.arth.2016.12.036.
- Ramaswamy A, Marchese M, Cole A P, Harmouch S, Friedlander D, Weissman J S, et al. Comparison of hospital readmission after total hip and total knee arthroplasty vs spinal surgery after implementation of the Hospital Readmissions Reduction Program. JAMA Netw Open 2019; 2(5): e194634. doi: 10.1001/JAMANETWORKOPEN.2019.4634.
- Harris I A, Hatton A, de Steiger R, Lewis P, Graves S, Wales S, et al. Declining early mortality after hip and knee arthroplasty. ANZ J Surg 2020; 90(1-2): 119-22. doi: 10.1111/ANS.15529.
Appendix
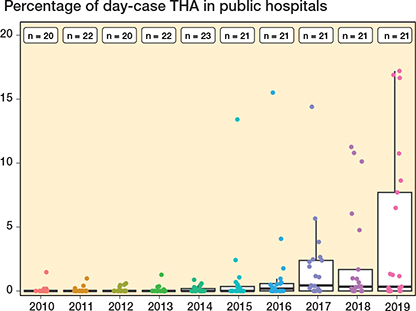
Figure 3. Percentage of day-case THA procedures for each public non-low-volume surgical center (≥ 100 cases/year). Each dot represents a surgical center. Boxplots show 25, 50, and 75 percentiles (box) as well as 5 and 95 percentiles (whiskers) for proportion of day-case surgery in surgical centers. Legends at the top of the figure show the number of surgical centers each year.
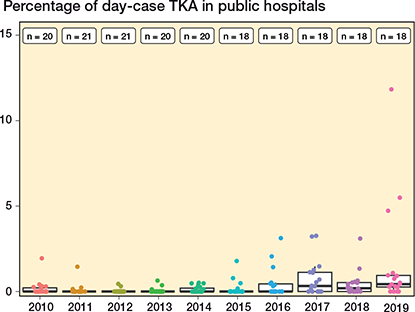
Figure 4. Percentage of day-case TKAs for each public non-low volume surgical center (≥ 100 cases/year). For interpretation, see Figure 3.
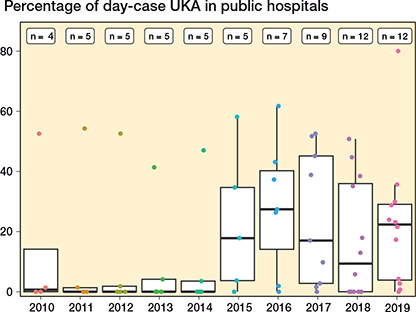
Figure 5. Percentage of day-case UKAs for each public non-low volume surgical center (≥ 52 cases/year). For interpretation, see Figure 3.
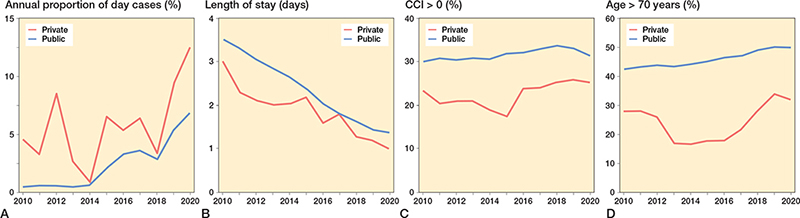
Figure 7. A. The use of day-case surgery sorted for public and private hospitals as a percentage of total number of performed procedures each year. B. The mean length of stay of public and private hospitals each year. C. The percentage of patients with a CCI score > 0 for public and private hospitals each year. D. The percentage of patients aged > 70 years for public and private hospitals each year. For abbreviations, see Figure 2.
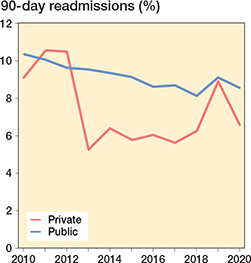
Figure 8. 90-day readmission rate (%) each year sorted for public and private hospitals.