Hip precautions after posterior-approach total hip arthroplasty among patients with primary hip osteoarthritis do not influence early recovery: a systematic review and meta-analysis of randomized and non-randomized studies with 8,835 patients
Christoffer B KORFITSEN 1,2,3, Lone R MIKKELSEN 4,5, Marie-Louise MIKKELSEN 1, Jeanett F ROHDE 1,6, Pætur M HOLM 7,8, Simon TARP 1, Holger-Henning F CARLSEN 9, Kirsten BIRKEFOSS 1, Thomas JAKOBSEN 10, Erik POULSEN 11, Jane S LEONHARDT 12, Søren OVERGAARD 13,14, and Inger MECHLENBURG 4,15,16
1 Danish Health Authority, Evidence-based Medicine, Copenhagen; 2 Cochrane Denmark & Centre for Evidence-Based Medicine Odense (CEBMO), Department of Clinical Research, University of Southern Denmark; 3 Open Patient Data Explorative Network (OPEN), Odense University Hospital, Odense; 4 Department of Clinical Medicine, Aarhus University; 5 Elective Surgery Centre, Silkeborg Regional Hospital; 6 The Parker Institute, Bispebjerg and Frederiksberg Hospital, Capital Region, Frederiksberg; 7 The Research Unit PROgrez, Department of Physiotherapy and Occupational Therapy, Næstved-Slagelse-Ringsted Hospitals; 8 The Research Unit for Musculoskeletal Function and Physiotherapy, University of Southern Denmark; 9 Særslev Medical Center, Søndersø; 10 Department of Orthopaedics, Aalborg University Hospital; 11 Department of Sports Science and Clinical Biomechanics, University of Southern Denmark; 12 Department of Orthopedics, Lillebaelt Hospital, Vejle; 13 Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg; 14 University of Copenhagen, Department of Clinical Medicine, Faculty of Health and Medical Sciences; 15 Department of Public Health, Aarhus University; 16 Department of Orthopaedics, Aarhus University Hospital, Denmark
Background and purpose — Hip precautions are routinely prescribed to patients with osteoarthritis to decrease dislocation rates after total hip arthroplasty (THA) using a posterior approach. However, recommendations have been based on very low certainty of evidence. We updated the evidence on the influence of hip precautions on early recovery following THA by this systematic review.
Materials and methods — We performed systematic searches for randomized controlled trials (RCT) and non-randomized (NRS) studies in MEDLINE, Embase, PEDro, and CINAHL published from 2016 to July 2022. 2 reviewers independently included studies comparing postoperative precautions with minimal or no precautions, extracted data, and assessed the risk of bias. Random effects meta-analyses were used to synthesize the results. The certainty of the evidence was rated by the Grading of Recommendations Assessment and Evaluation approach. The critical outcome was the risk of hip dislocations within 3 months of surgery. Other outcomes were long-term risk of dislocation and reoperation, self-reported and performance-based assessment of function, quality of life, pain, and time to return to work.
Results — 4 RCTs and 5 NRSs, including 8,835 participants, were included. There may be no or negligible difference in early hip dislocations (RCTs: risk ratio [RR] 1.8, 95% confidence interval [CI] 0.6–5.2; NRS: RR 0.9, CI 0.3–2.5). Certainty in the evidence was low for RCTs and very low for NRSs. Finally, precautions may reduce the performance-based assessment of function slightly, but the evidence was very uncertain. For all other outcomes, no differences were found (moderate to very low certainty evidence).
Conclusion — The current evidence does not support routinely prescribing hip precautions post-surgically for patients undergoing THA to prevent hip dislocations. However, the results might change with high-quality studies.
Citation: Acta Orthopaedica 2023; 94: 141–151. DOI https://doi.org/10.2340/17453674.2023.11958.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-08-26. Accepted: 2023-03-09. Published: 2023-04-05.
Correspondence: ckorfitsen@health.sdu.dk
Conceptualization: all authors; methodology: CBK, LRM, MLM, ST, KB; investigation: CBK, LRM, MLM, JFR, IM; data curation: CBK; formal analysis: CBK, ST; writing, review, and editing: all authors; supervision: TJ, PTH, ST, HHC, EP, JSL, SO, IM.
Handling co-editors: Bart Swierstra, Urban Rydholm and Philippe Wagner Acta thanks Maziar Mohaddes and Bart Pijls for help with peer review of this study.
Dislocation has been reported in 2–4% of cases after hip arthroplasty and is considered a serious complication associated with reduced quality of life and anxiety (1). The patients do not appear to achieve full relieving potential (2), and a substantial proportion experience recurring dislocations (3). The surgical approach is considered the most important risk factor for dislocation (4). A posterior (posterolateral) surgical approach has historically been associated with a higher risk of dislocation than a lateral surgical approach (1,5). Still, a recent study suggests that the risk of reoperation due to dislocation is equal to that of a direct lateral approach (6). However, surgeons may prefer the posterior approach owing to the risk of limping and increased pain in patients using the lateral approach (7).
Hip precautions are commonly prescribed postoperatively to reduce the risk of hip dislocation, but variation in clinical practice is common both between and within countries (8-10). Previous systematic reviews have questioned the rationale for prescribing hip precautions, as postsurgical protocols with minimal postoperative restrictions have demonstrated no difference in risk of dislocation and may lead to improved hip function (11-14), reduced healthcare costs, and fewer demands on clinical staff (15). However, no systematic review has included a quantitative synthesis of effectiveness and potential risks (11-14), and the certainty of the evidence has only been assessed in a Cochrane review from 2016 (13). Due to the large variations in clinical practice and uncertainty about the benefits and harms, the Danish Health Authority commissioned a National Clinical Guideline evaluating the evidence of precautions following primary THA in adults with primary hip osteoarthritis (OA) in 2016 (16). The guideline was updated in 2021 based on a systematic review from 2020. This review aimed to update the 2020 review to inform a potential update of the guideline with the following research question: Should patients with primary hip osteoarthritis be prescribed post-surgical movement precautions or minimal or no precautions after primary THA using a posterolateral approach?
Materials and methods
Study design
This work was part of updating a national clinical guideline on rehabilitation after THA in patients with hip OA, first published by the Danish Health Authorities in 2016. A protocol (i.e., description of the population, intervention, comparison, and outcomes) was registered on the Danish Health Authority Website a priori. It can be identified in the appendix (p. 68) of the published guideline (16). This systematic review and meta-analysis were conducted according to the recommendations from the Cochrane Collaboration and the GRADE framework (17,18). It is reported according to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (19).
Eligibility criteria
The clinical question was operationalized according to the population, intervention, comparator, and outcomes format (PICO) (20) and pre-specified explicitly in a protocol approved by the management of the Danish Health Authority. We included studies with patients undergoing THA for primary hip OA, comparing postoperative precautions (i.e., at least restrictions of hip flexion beyond 90°, adduction, and internal rotation) with minimal or no precautions as described by the study. For studies to be eligible for inclusion, more than 90% of the study participants had to receive a femoral prosthesis head of 32 millimeters or larger using a posterior surgical approach. We included published randomized controlled trials (RCTs) and non-randomized controlled studies (NRSs). Non-randomized studies were included as complementary in the analysis of rare-event outcomes (i.e., hip dislocations and reoperations) and as sequential in the case no RCT reported an outcome of interest (21). We included prospective and retrospective NRSs with a control group. Case-control studies were excluded.
Information sources
The literature searches were conducted in Embase, MEDLINE, Cochrane CENTRAL, CINAHL, and Pedro databases in July 2022. One reviewer (CBK) also searched Web of Science for any studies citing the included studies, for publications by the first and last author of included studies, and references of included studies.
Search strategy
The search strategies were initially developed for MEDLINE by the research specialist (KB) and adapted to the other electronic databases (see Supplementary data). No restrictions concerning publication status were applied. Studies in Danish, English, Swedish, and Norwegian were included.
Study selection and risk of bias
Citation management (automatic de-duplication), inclusion process, data extraction, and risk of bias assessment were managed using Covidence (Veritas Health Innovation, Melbourne, Australia). A combination of 2 reviewers (CBK, LRM, MLM, JFR, IM) independently screened all titles, abstracts, and the full text of identified studies against eligibility criteria. 2 reviewers independently extracted data and assessed the risk of bias using Cochrane’s risk of bias tool version 2.0 (RoB2.0) (22) and Risk of Bias In Non-randomized Studies–of Interventions (23) (ROBINS-I) of RCTs and NRSs, respectively. Exclusively for the ROBINS-I assessment of the risk of bias due to confounding, in the NRSs with a historically controlled design, femoral head size was considered an independent confounder for hip dislocations. Disagreements between reviewers were solved by consulting a 3rd reviewer. If a reviewer had a direct conflicting interest regarding an included study (e.g., authoring an included study), the reviewer was not allowed to assess the risk of bias or perform data extraction of the specific study. 1 author (CBK) contacted the corresponding author of included studies in the case of missing data or clarification issues.
Data extraction
We extracted data for studies reporting data based on the intention-to-treat (ITT) principle. Endpoint values were extracted when available and change scores from baseline to endpoint when systematic baseline difference between groups was identified. Median values were imputed as means, and standard deviations were calculated or measured on a graph (18). Studies without any quantification of variance for end-point or change scores had standard deviations imputed from baseline measures.
Data items
Outcomes were informed by the OMERACT-OARSI (Outcome Measures in Rheumatology–Osteoarthritis Research Society International) Core Domain Set for Measurement in Clinical Trials of Hip and/or Osteoarthritis (24). The critical outcome was early hip dislocations, defined as the number of patients with dislocations within 3 months post-surgery. Important outcomes included: hip dislocation at longest follow-up; reoperation from all causes at longest follow-up; return to work at longest follow-up; patient-reported function at the end of treatment and longest follow-up (close to 12 months and within 6 and 12 months post-surgery), preferably assessed with Hip disability and Osteoarthritis Outcome Score (HOOS) (25) activities of daily living; patient-reported hip-related pain at the end of treatment, preferably assessed with HOOS pain subscale; patient-reported health-related quality of life at the end of treatment, preferably assessed with HOOS quality of life subscale; performance-based assessment of function at the end of treatment, preferably assessed with 30-second Chair test, 40 meters fast-paced walk test, Timed up and go test, 6-minute walk test, or Stair climb test (26).
Reporting bias assessment
Risk of bias in trials, including a weighted summary plot of the risk of bias, was reported for each outcome and time point (low risk, some concerns, or high risk) of RCT and NRS (low risk, moderate risk, serious risk, or no information).
Certainty assessment
All reviewers rated the certainty in the evidence for each outcome using the GRADE approach (domains assessed were risk of bias, inconsistency, indirectness, imprecision, and publication bias) (27). Certainty was categorized as high, moderate, low, or very low.
Statistics
Effect measures and synthesis methods
All eligible trials were included in the summary of the evidence, and trials with outcome data were included in the meta-analyses, stratified by study design. We calculated effect size as a standardized mean difference (SMD) and summarized using inverse variance and Mantel–Haenszel random effects meta-analysis (i.e., the average of the intervention effects across all studies). As post hoc sensitivity analyses, fixed effects meta-analyses were performed and are reported in Supplementary data. Cochrane’s rule of thumb (< 0.4 = small effect, 0.4–0.7 = moderate effect, > 0.7 = large effect) was used to re-express SMD in the summary of findings (28). We estimated a weighted mean difference (WMD) for continuous outcomes on a particular scale. If necessary, binary outcome data was transformed to an SMD, and standard deviation (SD) was estimated from the odds ratio (29). For binary outcomes, we estimated the risk ratio (RR) with 95% confidence intervals (CI) and the absolute risk increase or reduction per 1,000. The number needed to treat (NNT) for an additional harmful event was reported for early hip dislocations for RCTs (30). Cochrane’s rule of thumb (RR < 0.75 or > 1.25) was used to assess minimal important differences (MID) in risk (harm or benefit). For all statistical analyses, we considered an α level of 0.05 to be statistically significant. Review Manager 5 (version 5.4.1, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) was used for all analyses, and Robvis (31) was used for risk of bias visualizations. The summary of findings table was produced in GradePro (GRADEpro Guideline Development Tool, McMaster University, and Evidence Prime, Canada).
Subgroup analyses and analyses of heterogeneity
The presence of publication bias was assessed by interpretation of funnel plot (32), and heterogeneity of results was assessed using the Cochrane Q test quantified as I2 values and the between-study variance τ2, with an I2 value > 50% considered as substantial heterogeneity (33). We did not protocolize any subgroup or sensitivity analyses. Thus the subgroup analysis (of the content of control intervention [i.e., some or no precautions] for the critical outcome, early hip dislocations) was considered post hoc and can be found in Supplementary data.
Ethics, registration, data sharing plan, funding, and disclosures
A protocol for this work was registered on the Danish Health Authority Website (16). Support for this study was partly provided by the Danish Ministry of Health based on the Danish Finance Act in 2017, and the work was approved and overseen by the Danish Health Authority. Members of the project group (CBK, LRM, ST, KB, MLM, and JFR) received salaries from the Danish Health Authority. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Data will be available upon reasonable request. CBK, JFR, EP, JSL, ST, MLM, TJ, PMH, KB, and SO declare no conflict of interest. LRM and IM declare no financial conflicts of interest. LRM and IM have authored a study (34) included in this review. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.11958
Results
Study selection
1 NRS was included from the 2016 review (34). The updated searches identified 1,860 unique references, of which 67 were screened in full text. Of these, 59 were excluded, leaving 4 new RCTs (35-38) and 4 new NRSs (39-42) for inclusion (Figure 1).
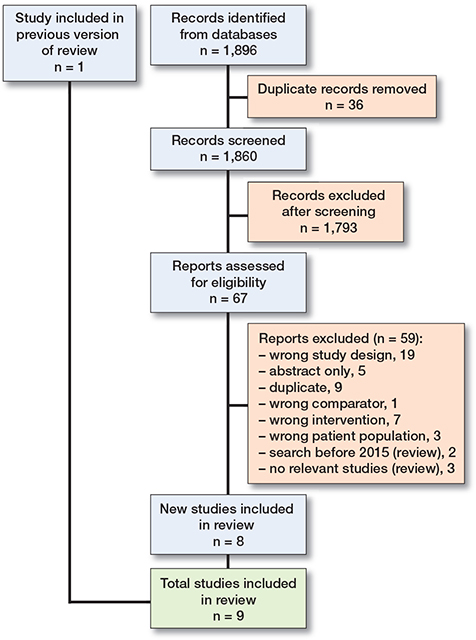
Figure 1. PRISMA flow diagram illustrating selection of studies.
Study characteristics
In the 4 single-center RCTs, 1,616 patients were randomized to either hip precautions or no or minimal precautions for 6 (35,36,38) or 8 (37) weeks. In the intervention groups, all patients were at least instructed to avoid hip flexion beyond 90°, adduction beyond the midline, and internal rotation, with Peters et al. limiting patients to supine sleeping (37). Assistive devices were not routinely prescribed in the 4 RCTs. Patients in the control groups were not instructed to follow any precautions in 3 trials (35,36,38). In Peters et al., patients were advised to avoid the combination of hip flexion beyond 90°, adduction beyond the midline, and internal rotation (37) (Table 1, see Appendix).
The 5 single-center NRSs included 7,219 patients using a non-randomized comparison before and after a procedure change from movement precautions to no or minimal precautions for 6 (34,39,41,42) or 12 (40) weeks (Table 1, see Appendix).
Results and certainty in the evidence
The following includes a summary of findings, an effect size interpretation, risk of bias assessments, and grading of the certainty of evidence (Table 2, see Appendix). Risk of bias assessments for each outcome, forest plots of all primary meta-analyses, and sensitivity analysis are available in Supplementary data.
Critical outcome
Early hip dislocations (Figure 2)
The median early dislocation rate in the 4 RCTs was 0.8% (range 0.5–1.5) (35-38). The meta-analysis showed an RR of 1.8 (CI 0.6–5.2) based on 10 dislocations in 810 patients (1.2%) in the precaution groups and 5 dislocations in 806 patients (0.6%) in the control groups. The absolute risk difference was 5 more per 1,000 (CI –2 to +26) in the precaution groups. The NNT for an additional early hip dislocation in the precaution groups was 164 (CI 65–313). The certainty in the evidence was low and downgraded due to high risk of bias (i.e., deviations from intended interventions, missing outcome data) and serious imprecision (i.e., few events and the confidence interval included a lower and higher threshold for MID in risk) (Table 2, see Appendix, Table 3).
| Study | Risk of b ias do mains | |||||
| 1 | 2 | 3 | 4 | 5 | Total | |
| Tetreault 2020 (35) |  |
 |
 |
 |
 |
 |
| Dietz 2019 (36) |  |
 |
 |
 |
 |
 |
| Peters 2019 (37) |  |
 |
 |
 |
 |
 |
| Mounts 2022 (38) |  |
 |
 |
 |
 |
 |
Judgements:  = high, = high,  = some concerns, = some concerns,  = low. = low. |
||||||
| Domains: 1 = Bias arising from the randomization process. 2 = Bias due to deviations from intended intervention. 3 = Bias due to missing outcome data. 4 = Bias in measurement of the outcome. 5 = Bias in selection of the reported results. |
||||||
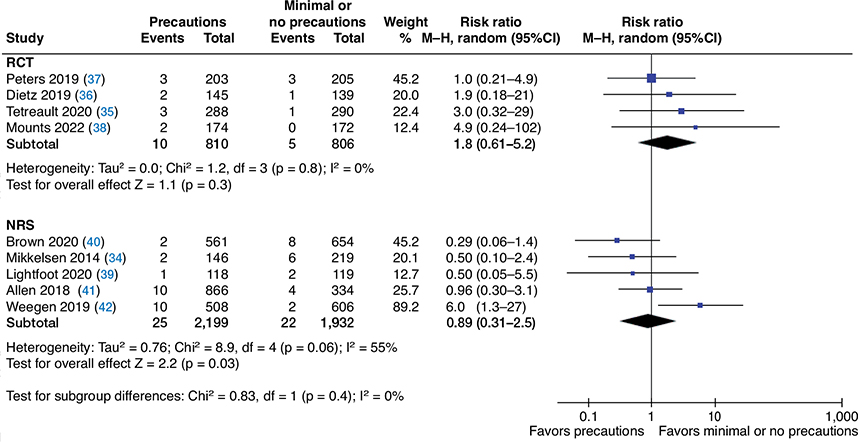
Figure 2. Random-effects meta-analysis on the effect of precautions on the risk of early dislocations after total hip arthroplasty. Abbreviations: M-H = Mantel-Haenszel, CI = confidence interval, RCT = randomized controlled trial NRS = non-randomized study.
The meta-analysis, including 5 NRSs, showed a RR of 0.9 (CI 0.3–2.5) based on 25 dislocations in 2,199 patients (1.1%) in precaution groups and 22 dislocations in 1,932 patients (1.1%) in control groups (34,39–42). There was considerable heterogeneity (I 2 55%). The absolute risk difference was 1 fewer per 1,000 (CI –8 to +17). The certainty in the evidence was very low and was downgraded due to serious risk of bias (i.e., selection bias, missing data, selective outcome reporting) and serious imprecision (i.e., few events and the confidence interval included a higher threshold for an MID) (Table 4). Visual inspection of the funnel plot with RCTs and NRSs did not indicate the presence of publication bias (see Supplementary data). Evidence from RCTs and NRSs suggests that hip precautions may have negligible or no difference in risk of early dislocations compared with minimal or no precautions.
| Study | Risk of bias domains | |||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Overall | |
| Allen 2018 (41) |  |
 |
 |
 |
 |
 |
 |
 |
| Lightfoot 2020 (39) |  |
 |
 |
 |
 |
 |
 |
 |
| Mikkelsen 2014 (34) |  |
 |
 |
 |
 |
 |
 |
 |
| Weegen 2019 (42) |  |
 |
 |
 |
 |
 |
 |
 |
| Brown 2019 (40) |  |
 |
 |
 |
 |
 |
 |
 |
Judgements: = serious, = serious,  = moderate, = moderate,  = low, = low,  = no information = no informationDomains: 1 = Bias due to confounding 2 = Bias due to selection of participants. 3 = Bias in classification of interventions. 4 = Bias due to deviations from intended interventions. 5 = Bias due to missing data. 6 = Bias in measurement of the outcome. 7 = Bias in selection of the reported results. |
||||||||
Important outcomes
Late hip dislocations
The meta-analysis, including 2 RCTs (35,38), showed an RR of 1 (CI 0.1–9.6) based on 1 late dislocation in 462 patients in both groups (0.2%). The absolute risk difference was 0 fewer per 1,000 (CI –2 to +19). The meta-analysis, including 2 NRSs, showed a RR of 0.9 (CI 0.1–6.2) based on 7 patients with dislocations of 3,112 (0.2%) in precaution groups and 3 dislocations in 1,327 patients (0.2%) in control groups (40,41). The absolute risk difference was 0 fewer per 1,000 (CI –2 to +12). Evidence from RCTs and NRSs suggests that precautions may have negligible or no difference in risk of late dis-locations compared with minimal or no precautions, but the evidence is very uncertain (see reasons for downgrading in Table 2 in Appendix).
Patient-reported function
3 RCTs found no difference in HOOS total score (0–100, higher better) at 6 weeks (35-37) when using a minimal clinical important difference (MCID) of 9 points (43). Tetreault et al. reported that 37% (98/288) of patients in the precaution group and 21% (64/290) in the control (p = 0.01) found daily activities difficult (35). The meta-analysis, including the 4 RCTs and 1,616 patients, showed an SMD of –0.2 (CI –0.2 to –0.1), which translates to a WMD on the HOOS of –1.3 (CI –2.2 to –0.3) points in favor of minimal or no precautions. The certainty in the evidence was moderate. At 1-year follow-up, the meta-analysis, including 2 RCTs and 620 patients, showed an WMD of –2.2 (CI –5 to 0.6) points on the HOOS in favor of minimal or no precautions (36,38). There was considerable heterogeneity (I2 62%). The certainty in the evidence was moderate. Evidence suggests precautions likely result in negligible or no difference in patient-reported function at the end of treatment and after 1 year compared with minimal or no precautions.
Performance-based assessment of function
1 NRS, Mikkelsen et al. (34) had blinded assessors to evaluate patients’ stair-climbing ability 3 weeks after the 6 weeks’ intervention. In the precaution group, 33% (40/122) of patients were capable of stair climbing versus 51% (103/201) in the control group (RR 0.6, CI 0.5–0.9) in favor of minimal or no precautions. The absolute risk difference was 184 fewer per 1,000 (CI –266 to –77) whom could stair climb in the precaution group. Evidence suggests that precautions may reduce the performance-based assessment of function slightly, at the end of treatment, compared with minimal or no precautions, but the evidence is very uncertain.
Hip-related pain
The meta-analysis, including 2 RCTs and 692 patients, showed an SMD of 0 (CI –0.2 to 0.2), which translates to a WMD on the VAS scale (0–100) of 0 (CI –1.5 to 1.5) points (36,37). The certainty in the evidence was moderate. Evidence suggests precautions likely result in negligible or no difference in hip-related pain at the end of treatment, compared with minimal or no precautions.
Health-related quality of life
The meta-analysis, including 2 RCTs and 692 patients, showed an SMD of –0.1 (CI –0.3 to 0), which translates to a WMD on the EQ-5D total score (0–1) of –0.01 (CI –0.02 to 0) points (36,37). The certainty in the evidence was moderate. Evidence suggests precautions likely result in negligible or no difference in patient-reported quality of life, at the end of treatment, compared with minimal or no precautions.
Return to work
1 RCT by Tetreault et al. (35) reported a mean difference of 2.1 days (CI –0.3 to 4.5) after surgery until work commencement. The certainty in the evidence was low. Evidence suggests that precautions may result in negligible or no difference in time to return to work, compared with minimal or no precautions.
Reoperation
The meta-analysis, including 2 RCTs (37,38), showed an absolute risk difference of 0 fewer per 1,000 (CI –10 to +10) based on 1 late dislocation in 377 patients in precaution groups (0.3%) and 0 of 377 patients in the controls. The certainty in the evidence was very low. The meta-analysis, including 2 NRSs, showed an RR of 1.2 (CI 0.5–3) based on 11 patients with revision THA of 1,663 (0.7%) in the precaution groups and 9 revision THAs in 1,703 patients (0.5%) in the control groups (40,42). The absolute risk difference was 1 more per 1,000 (CI –3 to +10) in patients with hip precautions. The certainty in the evidence was very low. Evidence from RCTs and NRSs suggests that precautions may have negligible or no difference in risk of reoperation after 1 year, compared with minimal or no precautions, but the evidence is very uncertain.
Discussion
Our findings suggest that precautions after THA have limited influence on recovery compared with fewer or no precautions. This review is an important update to the most recent published review. The most recent review from 2020 on hip dislocations following THA surgery included a narrative summary of the outcomes of dislocations, patient-reported function, and quality of life (11). However, 2 additional RCTs (35,38) and 2 NRSs (39,40) have been published since then. Despite the growing evidence base, there was still low or very low certainty in the evidence for most outcomes. This uncertainty is likely related to the challenges of answering the research question in a randomized study design (e.g., recruiting, monitoring patient adherence, and contamination bias), ultimately increasing the risk of bias. First, the included studies report low hip dislocation rates (median 0.8%) compared with a recent register study (3.5%) (1), suggesting that included patients were from a low-risk population. High-risk patients (older age, frailty, and serious multimorbidity) possibly declined to participate or were excluded. This hypothesis is supported by Dietz et al. and Peters et al., excluding patients with severe hip OA (36,37) and Mounts et al., including only patients with intra-articular stability (38). Second, recruitment to RCTs is a challenge. 3 studies reported rates between 19% and 59% declining to participate among all eligible patients (36-38,44). Despite removing only sleeping restrictions, 183 (79%) of the 232 patients declined to participate in Peters et al. because they were too anxious (37).
This review focused on the effect of being allocated to hip precautions or not and thus used the ITT analyses from the included studies. To investigate the effect of adherence to hip precautions, per protocol data could have been used in the analysis if reported in the included studies. 3 studies reported that 22–28% of patients did not comply with the precaution recommendations in their group (36,37,45), which are similar to previously reported adherence rates (44). Besides adherence, it will also be necessary to assess how dislocations occur and are reported. None of the included studies reported how patients dislocated their hip (e.g., excessive bending over, crossing the legs, falling when sleeping, or unexpected movement) (46). However, this was reported in the NRS by Gromov et al., and they did not find the removal of restrictions leading to an increased risk of dislocation or reduction of reoperations (47). In addition, they found that most dislocations (86%) were considered unavoidable (47).
Imprecision was another source of uncertainty when interpreting the differences in risks and wide confidence intervals, primarily owing to few events. Despite a relative risk increase of 80% in the precaution group for early dislocations, the estimate was insignificant, and the absolute difference was too small to be considered an MID. Using Cochrane’s rule of thumb of at least 300 events and the dislocation rate from the included RCT studies (0.8%) would require more than 38,000 or 8,600 patients using a rate of 3.5% (1).
Strengths and limitations
This is the first published systematic review, including meta-analyses, using the GRADE methodology on the influence of hip precautions on the risk of hip dislocations and recommended patient-important outcomes following THA surgery for patients with hip OA (24). We used methods recommended by the Cochrane Collaboration, including methods to reduce the risk of bias in the process, such as searches performed by a research librarian, duplicate inclusion of studies, duplicate data extraction using a data collection form, and duplicate risk of bias assessment. Also, we included both randomized and observational study designs to reflect the heterogeneous clinical practice and the limited evidence base.
However, some limitations should be considered when interpreting this review. The broad research question relied on us comparing evidence with differences in precautions between the restricted and unrestricted groups, with 1 RCT (37) and 2 NRSs (34,42) advising some precautions in the control groups. Including these in the meta-analysis increases the risk of a tooconservative relative risk estimate because they might influence the results towards no difference. The meta-analysis on the risk of early hip dislocation showed the same direction but a considerably larger effect when investigating differences through sensitivity analysis (see Supplementary data). For RCTs, when excluding Peters et al. (37), as the only study with precautions in the control group, the RR was 2.9 (CI 0.7–12, subgroup difference p-value: 0.3) and comparing the 2 NRSs with some precautions in the control group (34,42), showed an RR of 1.8 (CI 0.2–20) compared with RR 0.6 (CI 0.3–1.5) for the remaining 3 studies (p-value: 0.4). However, a reliable investigation of subgroup differences would require a larger number of studies and consideration of confounding. Thus, these differences should be interpreted with caution. Finally, 1 included RCT study reported a 16 percentage point difference (p = 0.01) in the number of patients who found daily activities difficult (35). Using the OR to calculate an SMD (29), we included the study in the meta-analysis of patient-reported function at the end of treatment. However, this conversion may have some limitations (e.g., the calculated standard error may not reflect the actual variance in the data and thus weigh inappropriately in the analysis). Thus, we included a meta-analysis without the study in Supplementary data. However, the results did not change the effect.
Clinical implications
Patients have distinct experiences and expectations for recovery (48,49). In certain patients, a higher risk of hip dislocation is likely (e.g., age above 75, suffering from multimorbidity, and patients with suboptimal prosthesis placement) (1). Undergoing surgery can create a feeling of vulnerability, affect patients’ self-esteem, and fear of potentially damaging their THA can overwhelm many (48,49). Some patients ultimately find that precautions provide reassurance (48). Whether to recommend movement precautions for these patients should be considered, but patients should be advised on returning to activities (48) irrespective of receiving precautions. Interviews with patients highlight that hip precautions impact patients’ physical and psychological recovery (48). First, they may limit patients’ participation in activities and be associated with an increased need for assistive devices, which has been shown to be a considerable cost for both the patient and the healthcare system (41,44,50). Second, some patients may invest time and resources in complying with precautions, sometimes even longer than intended (48). Recent studies elucidate the need to develop inpatient partnerships, and a post-surgery discharge plan to meet individual needs and preferences and to improve patient–clinician communication and patient-centered care (48,51,52).
In conclusion, based on our systematic review and meta-analyses, the current evidence does not support routinely prescribing hip precautions post-surgically for patients undergoing THA. Due to the low or very low certainty in the evidence for most outcomes, future studies could change the overall estimates. It is encouraged to investigate subgroups of patients with a higher need for postoperative hip precautions after THA.
Supplementary data
Risk of bias assessments for each outcome, forest plots of all primary meta-analyses, and sensitivity analysis are available as supplementary data in the online version of this article, doi: 10.2340/17453674.2023.11958
- Hermansen L L, Viberg B, Hansen L, Overgaard S. “True” cumulative incidence of and risk factors for hip dislocation within 2 years after primary total hip arthroplasty due to osteoarthritis: a nationwide population-based study from the Danish Hip Arthroplasty Register. J Bone Jt Surg 2021; 103(4): 295-302. doi: 10.2106/JBJS.19.01352.
- Hermansen L L, Viberg B, Overgaard S. Patient-reported outcome after dislocation of primary total hip arthroplasties: a cross-sectional study derived from the Danish Hip Arthroplasty Register. Acta Orthop 2022; 93: 29-36. doi: 10.1080/17453674.2021.1983973.
- Mechlenburg I, Knak J, Mosegaard S B, Axelsen M, Krarup Jensen N, Hansen T B, et al. Effectiveness of a bandage to prevent re-dislocation after total hip arthroplasty in patients with a previous hip dislocation: a randomized controlled trial with 12-week follow-up. Clin Rehabil 2022; 36(6): 767-75. doi: 10.1177/02692155221081462.
- Hermansen L L, Viberg B, Overgaard S. Large hospital variation in the risk of dislocation after primary total hip arthroplasty for primary osteoarthritis: 31,105 patients in 59 hospitals from the Danish Hip Arthroplasty Register. Acta Orthop 2022; 93: 503-8. doi: 10.2340/17453674.2022.2754.
- Kunutsor S K, Barrett M C, Beswick A D, Judge A, Blom A W, Wylde V, et al. Risk factors for dislocation after primary total hip replacement: a systematic review and meta-analysis of 125 studies involving approximately five million hip replacements. Lancet Rheumatol 2019; 1(2): e111-21. doi: 10.1016/S2665-9913(19)30045-1.
- Skoogh O, Tsikandylakis G, Mohaddes M, Nemes S, Odin D, Grant P, et al. Contemporary posterior surgical approach in total hip replacement: still more reoperations due to dislocation compared with direct lateral approach? An observational study of the Swedish Hip Arthroplasty Register including 156,979 hips. Acta Orthop 2019; 90(5): 411-16. doi: 10.1080/17453674.2019.1610269.
- Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S. Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop 2017; 88(3): 239-47. doi: 10.1080/17453674.2017.1291100.
- Gromov K, Troelsen A, Modaddes M, Rolfson O, Furnes O, Hallan G, et al. Varying but reduced use of postoperative mobilization restrictions after primary total hip arthroplasty in Nordic countries: a questionnaire-based study. Acta Orthop 2019; 90(2): 143-7. doi: 10.1080/17453674.2019.1572291.
- Smith T O, Sackley C M. UK survey of occupational therapist’s and physiotherapist’s experiences and attitudes towards hip replacement precautions and equipment. BMC Musculoskelet Disord 2016; 17: 228. doi: 10.1186/s12891-016-1092-x.
- Carli A V, Poitras S, Clohisy J C, Beaulé P E. Variation in use of post-operative precautions and equipment following total hip arthroplasty: a survey of the AAHKS and CAS membership. J Arthroplasty 2018; 33(10): 3201-5. doi: 10.1016/j.arth.2018.05.043.
- Crompton J, Osagie-Clouard L, Patel A. Do hip precautions after posterior-approach total hip arthroplasty affect dislocation rates? A systematic review of 7 studies with 6,900 patients. Acta Orthop 2020; 91(6): 687-92. doi: 10.1080/17453674.2020.1795598.
- van der Weegen W, Kornuijt A, Das D. Do lifestyle restrictions and precautions prevent dislocation after total hip arthroplasty? A systematic review and meta-analysis of the literature. Clin Rehabil 2016; 30(4): 329-39. doi: 10.1177/0269215515579421.
- Smith T O, Jepson P, Beswick A, Sands G, Drummond A, Davis E T, et al. Assistive devices, hip precautions, environmental modifications and training to prevent dislocation and improve function after hip arthroplasty. Cochrane Database Syst Rev 2016; 7: CD010815. doi: 10.1002/14651858.CD010815.pub2.
- Barnsley L, Barnsley L, Page R. Are hip precautions necessary post total hip arthroplasty? A systematic review. Geriatr Orthop Surg Rehabil 2015; 6(3): 230-5. doi: 10.1177/2151458515584640.
- Coole C, Edwards C, Brewin C, Drummond A. What do clinicians think about hip precautions following total hip replacement? Br J Occup Ther 2013; 76(7): 300-7. doi: 10.4276/030802213X13729279114898.
- NKR: Hofteartrose - ikke-kirurgisk behandling og genoptræning efter total hoftealloplastik [Internet]. [cited 2021, Oct 30]. Available from: https://www.sst.dk/da/udgivelser/2021/nkr-hofteartrose--ikke-kirurgiskbehandling-og-genoptraening-efter-tha.
- Alonso-Coello P, Oxman A D, Moberg J, Brignardello-Petersen R, Akl E A, Davoli M, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices 2: Clinical practice guidelines. BMJ 2016; 353: i2089. doi: 10.1136/bmj.i2089.
- Cochrane Handbook for Systematic Reviews of Interventions [Internet]. [cited 2022, Feb 10]. Available from: https://training.cochrane.org/ handbook/current.
- Page M J, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews [Internet]. MetaArXiv; 2020 Sep [cited 2021, Jan 23]. Available from: https://osf.io/preprints/metaarxiv/v7gm2/. doi: 10.31222/osf.io/v7gm2.
- Guyatt G H, Oxman A D, Kunz R, Atkins D, Brozek J, Vist G, et al. GRADE guidelines, 2: Framing the question and deciding on important outcomes. J Clin Epidemiol 2011; 64(4): 395-400. doi: 10.1016/j.jclinepi.2010.09.012.
- Cuello-Garcia C A, Santesso N, Morgan R L, Verbeek J, Thayer K, Ansari M T, et al. GRADE guidance 24: Optimizing the integration of randomized and non-randomized studies of interventions in evidence syntheses and health guidelines. J Clin Epidemiol 2022; 142:200-8. doi: 10.1016/j.jclinepi.2021.11.026.
- Sterne J A C, Savović J, Page M J, Elbers R G, Blencowe N S, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366. doi: 10.1136/bmj.l4898.
- Sterne J A, Hernán M A, Reeves B C, Savović J, Berkman N D, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919. doi: 10.1136/bmj.i4919.
- Smith T O, Hawker G A, Hunter D J, March L M, Boers M, Shea B J, et al. The OMERACT-OARSI core domain set for measurement in clinical trials of hip and/or knee osteoarthritis. J Rheumatol 2019; 46(8): 981-9 . doi: 10.3899/jrheum.181194.
- Nilsdotter A K, Lohmander L S, Klässbo M, Roos E M. Hip disability and osteoarthritis outcome score (HOOS): validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003; 4(1): 10. doi: 10.1186/1471-2474-4-10.
- Dobson F, Hinman R S, Roos E M, Abbott J H, Stratford P, Davis A M, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage 2013 Aug; 21(8): 1042-52. doi: 10.1016/j.joca.2013.05.002.
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines, 3: Rating the quality of evidence. J Clin Epidemiol 2011; 64(4): 401-6. doi: 10.1016/j.jclinepi.2010.07.015.
- Higgins J P T, Thomas J, Chandler J, Cumpston M, Li T, Page M J, Welch V A, editors. 12.6.2: Re-expressing SMDs using rules of thumb for effect sizes [Internet]. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. [cited 2022, Mar 14]. Available from: https://handbook-5-1.cochrane.org/chapter_12/12_6_2_re_expressing_smds_using_rules_of_thumb_for_effect_sizes.htm.
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 2000; 19(22): 3127-31. doi: 10.1002/1097-0258(20001130)19:22<3127::AID-SIM784>3.0.CO;2-M.
- Higgins J P T, Thomas J, Chandler J, Cumpston M, Li T, Page M J, Welch V A, editors. Chapter 15: Interpreting results and drawing conclusions [Internet]. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. [cited 2022 Oct 12]. Available from: https://training.cochrane.org/handbook/current/chapter-15.
- McGuinness L A, Higgins J P T. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods [Internet] 2020 Apr 26 [cited 2020, May 21]; n/a(n/a). Available from: https://doi.org/10.1002/jrsm.1411/.
- Sterne J A C, Harbord R M. Funnel plots in meta-analysis. Stata J 2004; 4(2): 127-41. doi: 10.1177/1536867X0400400204.
- Higgins J P T, Thompson S G. Quantifying heterogeneity in a metaanalysis. Stat Med 2002; 21(11): 1539-58. doi: 10.1002/sim.1186.
- Mikkelsen L R, Petersen M K, Søballe K, Mikkelsen S, Mechlenburg I. Does reduced movement restrictions and use of assistive devices affect rehabilitation outcome after total hip replacement? A non-randomized, controlled study. Eur J Phys Rehabil Med 2014; 50(4): 383-93.
- Tetreault M W, Akram F, Li J, Nam D, Gerlinger T L, Della Valle C J, et al. Are postoperative hip precautions necessary after primary total hip arthroplasty using a posterior approach? Preliminary results of a prospective randomized trial. J Arthroplasty 2020; 35(6S): S246-51. doi: 10.1016/j.arth.2020.02.019.
- Dietz M J, Klein A E, Lindsey B A, Duncan S T, Eicher J M, Gillig J D, et al. Posterior hip precautions do not impact early recovery in total hip arthroplasty: a multicenter, randomized, controlled study. J Arthroplasty 2019 ; 34(7, Suppl.): S221-S227.e1. doi: 10.1016/j.arth.2019.02.057.
- Peters A, Weele K ter, Manning F, Tijink M, Pakvis D, Huis in het Veld R. Less postoperative restrictions following total hip arthroplasty with use of a posterolateral approach: a prospective, randomized, non-inferiority trial. J Arthroplasty 2019; 34(10): 2415-19. doi: 10.1016/j.arth.2019.05.038.
- Mounts M R, Turner R A, Patel N B, Snelling E N, Phillips R E, Levesque D A, et al. Patients achieving 90°/45°/0° intraoperative stability do not require hip precautions following posterior approach total hip arthroplasty: a prospective randomized study. J Arthroplasty 2022; 37(8, Suppl.): S876-80. doi: 10.1016/j.arth.2022.01.028.
- Lightfoot C J, Sehat K R, Coole C, Drury G, Ablewhite J, Drummond A E R. Evaluation of hip precautions following total hip replacement: a before and after study. Disabil Rehabil 2021; 43(20): 2882-9. doi: 10.1080/09638288.2020.1721575.
- Brown M L, Ezzet K A. Relaxed hip precautions do not increase early dislocation rate following total hip arthroplasty. J Am Acad Orthop Surg 2020; 28(10): e440-7. doi: 10.5435/JAAOS-D-19-00261.
- Allen F C, Skinner D L, Harrison J, Stafford G H. The effect of precautions on early dislocations post total hip arthroplasty: a retrospective cohort study. HIP Int 2018; 28(5): 485-90. doi: 10.1177/1120700018762175.
- van der Weegen W, Kornuijt A, Das D, Vos R, Sijbesma T. It is safe to use minimal restrictions following posterior approach total hip arthroplasty: results from a large cohort study. Hip Int J Clin Exp Res Hip Pathol Ther 2019; 29(6): 572-7. doi: 10.1177/1120700018823504.
- Lyman S, Lee Y Y, McLawhorn A S, Islam W, MacLean C H. What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? Clin Orthop 2018; 476(12): 2432-41. doi: 10.1097/CORR.0000000000000456.
- Peak E L, Parvizi J, Ciminiello M, Purtill J J, Sharkey P F, Hozack W J, et al. The role of patient restrictions in reducing the prevalence of early dislocation following total hip arthroplasty: a randomized, prospective study. J Bone Joint Surg Am 2005; 87(2): 247-53. doi: 10.2106/JBJS.C.01513.
- Peters A, Manning F, Tijink M, Vollenbroek-Hutten M, Huis in ’t Veld R. Patient compliance with postoperative precautions in an unrestricted and a supine sleeping position following posterolateral total hip arthroplasty: a randomized controlled trial. Disabil Rehabil 2021; 0(0): 1-8. doi: 10.1080/09638288.2021.2012606.
- Jørgensen C C, Kehlet H, Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group. Fall-related admissions after fast-track total hip and knee arthroplasty: cause of concern or consequence of success? Clin Interv Aging 2013; 8:1569-77. doi: 10.2147/CIA.S52528.
- Gromov K, Troelsen A, Otte K S, Ørsnes T, Ladelund S, Husted H. Removal of restrictions following primary THA with posterolateral approach does not increase the risk of early dislocation. Acta Orthop 2015; 86(4): 463-8. doi: 10.3109/17453674.2015.1028009.
- Lightfoot C J, Coole C, Sehat K R, Drummond A E R. Hip precautions after total hip replacement and their discontinuation from practice: patient perceptions and experiences. Disabil Rehabil 2021; 43(20): 2890-6. doi: 10.1080/09638288.2020.1722262.
- Okafor L, Chen A F. Patient satisfaction and total hip arthroplasty: a review. Arthroplasty 2019; 1(1): 6. doi: 10.1186/s42836-019-0007-3.
- Ververeli P A, Lebby E B, Tyler C, Fouad C. Evaluation of reducing postoperative hip precautions in total hip replacement: a randomized prospective study. Orthopedics 2009; 32(12): 889. doi: 10.3928/0147744720091020-09.
- Specht K, Agerskov H, Kjaersgaard-Andersen P, Jester R, Pedersen B D. Patients’ experiences during the first 12 weeks after discharge in fast-track hip and knee arthroplasty: a qualitative study. Int J Orthop Trauma Nurs 2018; 31: 13-19. doi: 10.1016/j.ijotn.2018.08.002.
- Jansson M M, Harjumaa M, Puhto A P, Pikkarainen M. Patients’ satisfaction and experiences during elective primary fast-track total hip and knee arthroplasty journey: a qualitative study. J Clin Nurs 2020; 29(3-4): 567-82 . doi: 10.1111/jocn.15121.
Appendix
| First author (ref), country, study design | Sample size | Age | Female, n (%) | BMI | OA, n (%) | Posterior approach, n (%) | Femoral head size ≥ 32mm, n (%) | Duration |
| Allen 2018 (41), UK, NRS | ||||||||
| Intervention group: | 2,551 | 72 (64–78)a | 1,576 (62) | NA | 1,813 (71) | 866 (34) | 1,521 (60) | 6 weeks |
| Intervention: Standard hip precautions (not specified). | ||||||||
| Control group: | 673 | 71 (64–78)a | 432 (64) | NA | 634 (94) | 334 (50) | 556 (83) | 6 weeks |
| Intervention: No hip precautions. | ||||||||
| Brown 2020 (40), USA, NRS | ||||||||
| Intervention group: | 589 | 68 (11)b | 326 (55) | 28.5 (5.5)b | 520 (88) | 589 (100) | 589 (100) | 12 weeks |
| Intervention: Use of abduction pillow in hospital, avoiding hip flexion beyond 90°, adduction, and internal rotation, a pillow between their legs while sleeping, and using an elevated toilet seat. | ||||||||
| Control group: | 653 | 68 (11)b | 374 (57) 28.2 | (5.4)b | 583 (89) | 653 (100) | 653 (100) | 12 weeks |
| Intervention: Instructing patients not to cross their legs. | ||||||||
| Dietz 2019 (36), USA, RCT | ||||||||
| Intervention group: | 145 | 63 (61–64)c | 64 (44) | 30 (29–31)c | NA | 145 (100) | 35.3 d | 6 weeks |
| Intervention: No hip flexion greater than 90°, no internal rotation of the hip, and no adduction of the hip. | ||||||||
| Control group: | 139 | 63 (62–65)c | 71 (51) | 31 (30–32) c | NA | 139 (100) | 34.7e | 6 weeks |
| Intervention: No hip precautions. | ||||||||
| Lightfoot 2020 (39), UK, NRS | ||||||||
| Intervention group: | 118 | 67 (11)b | 73 (62 | 29.1 (5.4)b | 230 (97) | 82 (69) | NA | 6 weeks |
| Intervention: Avoiding hip flexion beyond 90°, adduction, and rotation, and practicing activities of daily living within these movement restrictions, such as getting on and off chairs. Use of assistive devices, including a raised toilet seat | ||||||||
| Control group: | 119 | 68 (10)b | 85 (71) | 29.1 (8.9)b | 230 (97) | 82 (69) | NA | 6 weeks |
| Intervention: Patients were allowed to move within a comfortable range of motion and as pain allowed. Assistive devices were provided to patients who required them following clinical assessment. | ||||||||
| Mounts 2022 (38), USA, RCT | ||||||||
| Intervention group: | 174 | 66 (9.9)b | 87 (50) | 29.8 (5.5)b | 159 (91) | 174 (100) | 174 (100)) | 6 weeks |
| Intervention: Avoiding hip flexion beyond 90°, adduction, and internal rotation. Use of abduction pillow. | ||||||||
| Control group: | 172 | 70 (11)b | 95 (55) | 28.9 (5.0)b | 154 (90) | 172 (100) | 172 (100) | 6 weeks |
| Intervention: Perform activities as tolerated but are advised to avoid extremes of motion based on their discretion. | ||||||||
| Mikkelsen 2014 (34), DK, NRS | ||||||||
| Intervention group: | 146 | 69 (10)b | 68 (47) | 27.2 (5.1)b | 146 (100) | 146 (100) | 141 (96) | 6 weeks |
| Intervention: Avoiding hip flexion beyond 90°, adduction, and internal rotation. Assistive devices include an elevated toilet seat, shoe-horn, bath bench, ergonomic reacher, sock aid, and wedge pillow. | ||||||||
| Control group: | 219 | 68 (9.9)b | 106 (48) | 26.5 (4.1)b | 219 (100) | 219 (100) | 210 (96) | 6 weeks |
| Intervention: Avoid-ing the combina-tion of full hip flexion, internal rotation, and adduction. Assistive devices were only distributed when needed for the patient to perform activities of daily living. | ||||||||
| Peters 2019 (37), NL, RCT | ||||||||
| Intervention group: | 205 | 64 (10)b | 124 (61) | NA | 205 (100) | 205 (100) | 205 (100) | 8 weeks |
| Intervention: Avoid activities to hip flexion beyond 90°, adduction, and internal rotation. Restricted to supine sleeping. | ||||||||
| Control group: | 203 | 64 (10)b | 109 (54) | NA | 203 (100) | 203 (100) | 203 (100) | 8 weeks |
| Intervention: Avoiding the combination of full hip flexion, internal rotation, and adduction. | ||||||||
| Tetreault 2020 (35), USA, RCT | ||||||||
| Intervention group: | 288 | 64 (9.3)b | 149 (51) | 32.9 (8.5)b | 281 (98) | 288 (100) | 281 (98) | 6 weeks |
| Intervention: Avoiding hip flexion beyond 90°, adduction, and internal rotation. | ||||||||
| Control group: | 290 | 63 (9.6)b | 135 (58) | 32.1 (8.1)b | 285 (98) | 290 (100) | 283 (98) | 6 weeks |
| Intervention: No precautions. Patients could use assistive devices if desired for comfort. | ||||||||
| Van der Weegen 2019 (42), NL, NRS | ||||||||
| Intervention group: | 1,049 | 69 (14)a | 699 (67) | NA | 1,011 (96) | 1,049 (100) | 606 (58) | 6 weeks |
| Intervention: Supine sleeping, abduction pillow, and avoid hip flexion above 90°. Assistive devices include an elevated toilet seat, elevated chair, and crutches. | ||||||||
| Control group: | 1,102 | 69 (13)a | 652 (59) | NA | 1,068 (97) | 1,102 (100) | 508 (46) | 6 weeks |
| Intervention: Avoid the combination of full hip flexion, internal rotation, and adduction. Advised patients not to cross their legs and not to bend with the operated leg moving back-ward. Assistive devices were distributed when needed for the patients to perform activities of daily living. | ||||||||
| BMI = Body Mass Index; OA = Osteoarthritis; NA = Not available; RCT = Randomized controlled trial; NRS = Non-randomized study. | ||||||||
| aMedian (interquartile range); bMean (standard deviation); cMean (95% confidence interval) dMean 35.3 (95%CI 34.9–35.7); eMean 34.7 (95%CI 34–35) | ||||||||
| Certainty assessment | Events/patients | Effect | |||||||||
| No of Study | studies design | Risk of bias | Inconsistency | Indirectness | Other considerations | Impre cision | Precautions n/N (%) | No precautionsb n/N (%) | Relative (CI) | Absolute (CI) | Certainty b |
| Early hip dislocation, within 3 months (follow-up range 6–8 weeks), critical outcome | |||||||||||
| 4 (35-38)) | RCT | seriousc | not serious | not serious | seriousd | none | 10/810 (1.2) | 5/806 (0.6) | RR 1.8 (0.6–5.2) | +5 per 105 (–2 to +26) | ⊗⊗○○ low |
| Early hip dislocation, within 3 months (follow-up range 6–12 weeks) critical outcome | |||||||||||
| 5 (34,39-42) | NRS | seriouse | not serious | not serious | seriousf | none | 25/2,199 (1.1) | 22/1,932 (1.1) | RR 0.9 (0.3–2.5) | –1 per 105 (–8 to +17) | ⊗○○○ very low |
| Late hip dislocation, longest follow-up (follow-up 29 weeks), important outcome | |||||||||||
| 2 (35,38) | RCT | seriousc | not serious | not serious | very seriousf | none | 1/462 (0.2) | 1/462 (0.2) | RR 1.0 (0.1–9.6) | 0 per 105 (–2 to +19) | very low |
| Late hip dislocation, longest follow-up (follow-up range 6–12 months), important outcome | |||||||||||
| 2 (40,41) | NRS | seriouse | not serious | seriousg | seriousf | none | 7/3112 (0.2) | 3/1327 (0.2) | RR 0.9 (0.1–6.2) | 0 per 105 (–2 to +12) | ⊗○○○ very low |
| Patient-reported function (follow-up range 6–8 weeks, assessed with HOOS, ADL questionnaire), important outcome | |||||||||||
| 4 (35-38) | RCT | serioush | not serious | not serious | not serious | none | 810 | 806 | – | SMD –0.2 (–0.2 to –0.1) | ⊗○○○ moderate |
| Patient-reported function, (follow-up 1 year, assessed with HOOS), important outcome | |||||||||||
| 2 (36,38) | RCT | serioush | not serious | not serious | not serious | none | 319 | 311 | – | MD –2.2 (–5 to +0.6) | ⊗⊗⊗○ moderate |
| Hip-related pain, end of treatment (follow-up range 6–8 weeks, assessed with Rate of pain worksheet 0–1, VAS 0–100), important outcome | |||||||||||
| 2 (36,37) | RCT | seriousi | not serious | not serious | not serious | none | 348 | 344 | – | SMD 0 (–0.2 to +0.2) | ⊗⊗⊗○ moderate |
| Health-related quality of life, end of treatment (follow-up range 6–8 weeks, assessed with EQ-5D 0–1, VAS Health State), important outcome | |||||||||||
| 2 (36,37) | RCT | seriousi | not serious | not serious | not serious | none | 348 | 344 | – | SMD –0.1 (–0.3 to +0) | ⊗⊗⊗○ moderate |
| Performance-based assessment of function, end of treatment (follow-up 9 weeks, assessed with: “Stairclimbing ability”), important outcome | |||||||||||
| 1 (34) | NRS | seriousj | not serious | not serious | seriousk | none | 40/122 (33) | 103/201 (51) | RR 0.6 (0.5–0.9) | –184 per 105 (–266 to –77) | ⊗○○○ very low |
| Return to work (days), longest follow-up, important outcome | |||||||||||
| 1 (35) | RCT | seriousl | not serious | not serious | seriousm | none | 288 | 290 | - | MD +2.1 (–0.3 to +4.5) | ⊗⊗○○ low |
| Reoperation, all causes (follow-up 8 weeks), important outcome | |||||||||||
| 2 (37,38) | RCT | seriousc | not serious | not serious | very seriousn | none | 1/377 (0.3) | 0/377 (0.0) (–0.01 to 0.01) | RD 0.00 | 0 per 105 (–10 to +10) | ⊗○○○ very low |
| Reoperation, all causes, longest follow-up (> 1 year), important outcome | |||||||||||
| 2 (40,42) | NRS | seriouso | not serious | not serious | seriousf | none | 11/1,663 (0.7) | 9/1,703 (0.5) | RR 1.2 (0.5–3) | 1 per 105 (–3 to +10) | ⊗○○○ very low |
| CI = 95% confidence interval; MD = mean difference; RR = risk ratio; RD = risk difference; NRS = Non-randomized study; RCT = Randomized controlled trial; SMD = standardized mean difference; HOOS = Hip Disability and Osteoarthritis Outcome Score; ADL = Activities of daily living; VAS = Visual analog scale; EQ-5D = EuroQol 5 dimension. | |||||||||||
| aor minimal precautions. | |||||||||||
| bGrading of Recommendations Assessment and Evaluation (GRADE) Working Group grades of evidence: high certainty (very confident that true effect lies close to estimate of effect); moderate certainty (moderately confident in the effect estimate: the true effect is likely to be close to the estimate of effect, but the possibility that it is substantially different exists); low certainty (confidence in the effect estimate is limited: true effect may be substantially different from the estimate of effect); very low certainty (very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect). | |||||||||||
| cHigh risk of bias due to deviations from intended interventions and some concerns regarding missing outcome data | |||||||||||
| dSerious imprecision owing to few events and the confidence interval included a lower and higher threshold for a minimally important difference in risk | |||||||||||
| eSerious risk of bias due to risk of selection bias, bias due to missing data, and selective outcome reporting | |||||||||||
| fSerious imprecision owing to few events and the confidence interval included a higher threshold for a minimally important difference | |||||||||||
| gSerious indirectness due to differences in surgical approach between studies. | |||||||||||
| hSome concerns regarding deviations from intended interventions and bias in the measurement of the outcome (i.e., no blinding) | |||||||||||
| iSerious risk of bias due to some concerns regarding the randomization process, deviations from intended interventions, missing data, bias in the meas-urement of the outcome | |||||||||||
| jModerate risk of bias owing to missing data and bias in selecting the reported result. | |||||||||||
| kSerious imprecision owing to data from 1 study and the confidence interval included both the lower and higher threshold for a minimally important risk difference | |||||||||||
| lHigh risk of bias due to deviations from intended interventions | |||||||||||
| mSerious imprecision owing to few included patients, only data from 1 study, and the confidence interval included a higher threshold for a minimally important risk difference | |||||||||||
| nSerious imprecision owing to few included patients and no reported events in control groups | |||||||||||
| oSerious risk of bias due to confounding (difference in femoral head size between groups) and selective outcome reporting | |||||||||||