Minimal invasions: is wrist arthroscopy supported by evidence? A systematic review and meta-analysis
Venla-Linnea KARJALAINEN 1, Ian A HARRIS 2, Mikko RÄISÄNEN 3, and Teemu KARJALAINEN 4
1 Central Finland Health Care District; 2 Ingham Institute for Applied Medical Research, South West-ern Sydney Clinical School, UNSW Sydney, Liverpool, NSW, Australia; 3 Department of Orthopae-dics and Hand Surgery, Kuopio University Hospital, Kuopio, Finland; 4 Department of Surgery, Hospital Nova of Central Finland, Jyvaskyla, Finland and Monash Department of Clinical Epidemiology, Cabrini Institute and Department of Epidemiology and Preventive Medicine, School of Public Health & Preventive Medicine, Monash University, Malvern, Australia
Background and purpose — Wrist arthroscopy is used increasingly, but its benefits and harms are unclear. This systematic review aimed to identify all published randomized controlled trials on wrist arthroscopy and synthesize the evidence of the benefits and harms of wrist arthroscopic procedures.
Methods — We searched CENTRAL, MEDLINE, and Embase for randomized controlled trials comparing wrist-arthroscopic surgery with corresponding open surgery, placebo surgery, a non-surgical treatment, or no treatment. We estimated the treatment effect with a random effect meta-analysis using patient reported outcome measure (PROM) as primary outcome where several studies assessed the same intervention.
Results — Of 7 included studies, none compared wrist arthroscopic procedures with no treatment or placebo surgery. 3 trials compared arthroscopically assisted reduction with fluoroscopic reduction of intra-articular distal radius fractures. The certainty of evidence was low to very low for all comparisons. The benefit of arthroscopy was clinically unimportant (smaller than what patients may consider meaningful) at all time points. 2 studies compared arthroscopic and open resection of wrist ganglia, finding no significant difference in recurrence rates. 1 study estimated the benefit of arthroscopic joint debridement and irrigation in intra-articular distal radius fractures, showing no clinically relevant benefit. 1 study compared arthroscopic triangular fibrocartilage complex repair with splinting in distal radioulnar joint instability in people with distal radius fractures, finding no evidence of benefits for repair at the long-term follow-up but the study was unblinded, and the estimates imprecise.
Conclusion — The current limited evidence from RCTs does not support benefits of wrist arthroscopy compared with open or non-surgical interventions.
Citation: Acta Orthopaedica 2023; 94: 200–206. DOI https://doi.org/10.2340/17453674.2023.11957.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-19. Accepted: 2023-03-16. Published: 2023-04-27.
Correspondence: teemu.karjalainen@ksshp.fi
TK and VLK conceived the study, extracted the data, assessed the certainty of the evidence, and wrote the initial draft. MR and VLK assessed the risk of bias. VLK performed the data analysis. IAH and MR gave critical comments on and edited the draft. All authors discussed and contributed to the final manuscript.
The authors would like to thank Trevor Corson, who assisted with and provided insights on the language and writing of this article.
Handling co-editor: Taco Gosens
Acta thanksGerald Kraan, Yrjänä Nietosvaara, and Maria Wilcke for help with peer review of this study.
Surgeons increasingly use wrist arthroscopy to diagnose and treat a wide variety of intra-articular wrist conditions (1). The rationale for arthroscopy is that it enables accurate diagnosis and definitive treatment in the same setting with less injury to soft tissue compared with open surgery. Furthermore, better visualization can improve the precision of the procedure, such as when reducing joint surface fragments in an intra-articular distal radius fracture (2-6). Surgical indications for wrist arthroscopy are increasing as new instruments allow more intricate procedures, such as removal of carpal bones, partial arthrodesis, or ligament reconstructions, to be performed arthroscopically (7,8). However, prolonged operative duration and special instrumentation required for arthroscopic surgery increase the costs of the procedure.
Due to the increased costs, arthroscopic surgery should provide corresponding, patient-important benefits over open surgery, nonoperative care, or no treatment. To investigate whether wrist arthroscopy provides such benefits, we conducted a systematic review of evidence from RCTs assessing the effects of wrist arthroscopic procedures. The specific aims of this systematic review were to (i) map the empirical evidence estimating effects of wrist arthroscopic procedures, and (ii) assess whether wrist arthroscopic procedures provide superior benefits to patients compared with open procedures or no procedures (nonoperative treatment, placebo treatment, or no treatment).
Methods
We followed the PRISMA guidelines throughout the study (9).
Identification of studies
We included all randomized or quasi-randomized controlled trials that compared any wrist arthroscopic treatment with corresponding open surgery, placebo treatment (including diagnostic wrist arthroscopy), or a non-surgical treatment (including, for example, waiting list control) in participants with any wrist condition. We performed searches in MEDLINE, Embase, and CENTRAL databases on November 8, 2021.
Study selection
Two authors (VLK, TK) screened the titles and abstracts and reviewed the full texts of potentially eligible studies. Disagreements were settled through discussion.
Outcome measures
The following outcome measures were considered in this review: wrist or upper extremity specific patient reported outcome measure (PROM; primary outcome), pain, global improvement, grip strength, and adverse events. When several functional outcomes were reported in the same trial, we prioritized the Disabilities of Shoulder, Arm, and Hand (DASH) score for the PROM as it was reported by most of the studies. The DASH questionnaire is an upper-extremity-specific PROM yielding a total score ranging from 0 points (no disability) to 100 points (worst possible disability) (10).
Secondary outcomes were pain measured with a visual analog scale (VAS), global improvement (dichotomous), grip strength (percentage compared with healthy side), and the proportion of participants with adverse events. Ganglion recurrence was not in our protocol, but we collected it as it was the only outcome measured in ganglion trials.
The predefined time points were short term (< 3 months), medium term (3–6 months, longer time point was extracted when both were reported), and long term (> 6 months, longest available time point was extracted).
Data collection and handling
We extracted all data to a pre-tested pro forma. The extracted data included the name of the first author, year of publication, number of participants, the condition being treated, the intervention and control treatments, and the outcomes at each time point. The number of adverse events was collected at the latest available follow-up. We preferred data from the intention-to-treat analysis but, if not reported, we used per protocol or astreated data.
For continuous outcomes, we extracted the mean and SD values. If the mean was not available, we used median as an approximation of the mean. When SD was not available, we calculated it based on 95% confidence intervals (CIs) or based on interquartile range when CIs were not reported.
Measurement of treatment effect and data synthesis
All meta-analyses were stratified by condition and intervention. We used inverse variance weighting with a random effects model in all meta-analyses. When several different measures were used for one outcome domain, we used the standardized mean difference (SMD) for pooling and then back-translated the SMD to the original scale using typical SD (median SD at the baseline). We used 0.05 as the level of statistical significance but estimated whether the benefit was patient-important based on the CI of the estimate and the minimal clinically important difference (MCID) value of the corresponding outcome measure (11). Before pooling, we assessed clinical diversity by examining the inclusion and exclusion criteria, diagnostic criteria, and details of the intervention. We determined heterogeneity of the meta-analysis with visual inspection of the forest plots and I2 statistics. When substantial unexplained heterogeneity was present, we downgraded the certainty of evidence as suggested by the GRADEpro handbook (12).
For binary outcomes, we extracted events and the total number of participants at each time point. When total numbers were not available, we used the number of participants randomized to each group. We expressed the treatment effect as relative risk (RR) with 95% confidence intervals.
We used the packages meta and metafor in R (4.0.0) with the software RStudio (1.2.5042) R Foundation for Statistical Computing, Vienna, Austria) for the meta-analyses (13-16).
Risk of bias and certainty of evidence (see Appendix)
Two authors (VLK, MR) independently assessed the risk of bias based on the Cochrane risk of bias tool 1.0 (17). Disagreements were settled by discussion and deferral to a third author when necessary. We assessed the certainty of evidence using the GRADEPRO tool (18). We downgraded the certainty (reflecting our confidence in the pooled treatment effect) based on (i) risk of bias (downgraded when included studies were at high or unclear risk of bias) (ii) inconsistency (certainty was downgraded if the studies in the meta-analyses were inconsistent without apparent explanation); (iii) imprecision of the estimates (the treatment estimates were considered precise when the 95% confidence intervals excluded or supported patient-important benefits); (iv) indirectness of the evidence (indirectness was present when surrogate outcomes were used). For grip strength, we did not assess certainty as it is not a patient-reported outcome and the relevance of differences is unclear. However, we included this outcome because it was measured in most studies and may reflect pain and function to some degree. We did not assess publication bias because of the low number of studies available for each meta-analysis.
Registration, funding, and disclosures
This systematic review was prospectively registered in the PROSPERO database. The study received no funding. Teemu Karjalainen has received funding from Academy of Finland. Other authors declare no conflict of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.11957
Results
Literature search and study selection
The search yielded 271 records of which 259 were excluded in the initial screening process. After reading 12 full texts, we included 7 eligible studies (Figure 1). Additionally, 3 potentially eligible ongoing studies were registered in ClinicalTrials.gov registry: NCT02911610, NCT04755127, and NCT04576169.
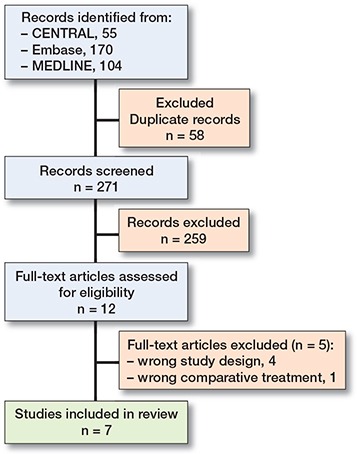
Figure 1. PRISMA flow diagram of included articles.
The studies were conducted between 1999 and 2020 in Greece, Italy, Japan, Korea, the Netherlands, and the USA and are summarized in the Table. 3 studies compared arthroscopically assisted reduction with fluoroscopic reduction of distal intra-articular radius fractures (19-21); 2 studies compared arthroscopic removal of wrist ganglion with open removal (22,23); 1 study assessed the effect of debridement and irrigation of the radiocarpal joint in intra-articular distal radius fractures (24); and 1 study compared triangular fibrocartilage complex (TFCC) repair with supination cast in distal radioulnar joint (DRUJ) instability identified during operation for unstable distal radius fractures (25).
| Trial | Country | Participants women/total | Mean age | Arthroscopic intervention | Control | Analyzed outcomes | Follow-up, months mean (range) |
| Arthroscopically assisted reduction vs. open/fluoroscopic reduction for intra-articular fractures of the distal radius | |||||||
| Doi 1999 (19) | Japan | 47/82 | 54 | Arthroscopically assisted reduction and external fixation | Fluoroscopic reduction and internal fixation | Modified system of Green and O’Brien; adverse events | 31 (24–47) |
| Varitimidis 2008 (20) | Greece | 23/40 | 46 | Arthroscopically and fluoro-scopically assisted reduction and external fixation plus percutaneous pinning | Fluoroscopic reduction and external fixation plus percutaneous pinning | DASH score; grip strength; adverse events | 24 |
| Yamazaki 2015 (21) | Japan | 54/74 | 64 | Arthroscopically assisted reduction and fixation with a volar locking plate | Fluoroscopic reduction and fixation with a volar locking plate | DASH score; grip strength; adverse events | 11 |
| Arthroscopic excision vs. open excision for wrist ganglia | |||||||
| Kang 2008 (22) | USA | 48/72 | 35 | Arthroscopic excision | Open excision | Ganglion recurrence; adverse events | 12 |
| Rocchi 2008 (23) | Italy | 34/50 | 37 | Arthroscopic resection through 2 or 3 dorsal ports | Open excision through a longitudinal volar skin incision | Adverse events (including ganglion recurrence) | 26 (12–39) |
| Open reduction with arthroscopic debridement vs. open reduction alone for intra-articular fractures of the distal radius | |||||||
| Selles 2020 (24) | Netherlands | 33/50 | 59 | Open reduction and internal fixation with arthro-scopic debridement | Open reduction and internal fixation alone | DASH score; postop. pain (VAS); grip strength; adverse events | 12 |
| Arthroscopic TFCC repair vs. supination splint for DRUJ instability with distal radius fracture | |||||||
| Lee 2016 (25) | Korea | 9/12 a | 46 | Arthroscopic TFCC repair | Supination sugar-tong splint | DASH score; grip strength; adverse events | 17 (13–24) |
| a 158 in entire study, 12 allocated to included treatments. | |||||||
Arthroscopically assisted reduction vs. open/fluoroscopic reduction for intra-articular fractures of the distal radius
PROM
The benefits of arthroscopic reduction may be smaller than the minimal clinically important difference (MCID of 10.8 points in DASH) (11). The evidence was downgraded to low certainty due to risk of bias (lack of blinding) and imprecision (the confidence intervals did not exclude patient-important benefits) at short and long term, and very low at medium term (third step for inconsistency).
At the short-term follow-up, any PROM for function was reported by only 1 of the 3 studies (20); the mean DASH score was 28 with open reduction and was 3.0 points better (CI 5.2 worse to 11 better; 1 study; 70 participants) with arthroscopic reduction.
2 studies measured PROM at the medium-term follow-up (20,21); the mean DASH score was 14.5 with open and was 4.7 better (CI 12 worse to 21 better; 2 studies; 110 participants; I2 = 97%) with arthroscopic reduction.
At the long-term follow-up, all 3 studies reported PROM but 1 (19) used a different measure. The pooled standardized mean difference (SMD) was –0.41 (CI –1.0 to 0.19; 3 studies; 192 participants; I2 = 75%) favoring arthroscopic reduction. This translates to an improvement of 4.3 points (CI 2.0 worse to 10.5 better) in the DASH score with arthroscopic reduction. (Figure 2)
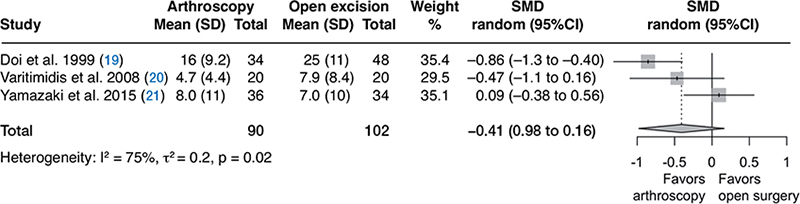
Figure 2. Forest plot of PROM at the long-term follow up in the comparison of arthroscopically assisted reduction with open/fluoroscopic reduction for intra-articular fractures of the distal radius.
Adverse events
There were 13/90 adverse events in the arthroscopic treatment group and 12/102 in the open treatment group. These included, e.g., infection, severe stiffness of finger joints, reflex sympathetic dystrophy, carpal tunnel syndrome. The pooled risk ratio was 1.15 (CI 0.07 to 19.5, 3 studies, 192 participants, I2 = 46%). The certainty of evidence was very low due to very serious imprecision and risk of bias.
Grip strength
At short and medium term, grip strength as the percentage compared with the healthy contralateral wrist was measured in 1 of the 3 studies (70 participants) (21). At the short-term follow-up point, the mean grip was 48% of the contralateral side in the open reduction group and 5.0% worse (CI 15.3% worse to 5.3% better) in the arthroscopic group. At the medium-term follow-up, the mean grip in the open treatment group was 84% of the contralateral side and was 2.0% worse (CI 10% worse to 6.3% better) in the arthroscopic group.
At the long-term follow-up point, 2 studies (152 participants) measured grip strength (19,21). The mean grip strength in the control group was 83% and was 5.2% worse (CI 15% worse to 4.6% better , I2 = 66%) in the arthroscopic reduction group.
Arthroscopic excision vs. open excision for wrist ganglia
In this comparison, we identified 2 trials (22,23). Kang et al. studied dorsal ganglia whereas Rocchi et al. studied volar ganglia. Neither study measured patient-reported outcomes such as pain or PROMs. The evidence regarding ganglion recurrence and adverse events was downgraded as very low due to risk of bias (lack of blinding) and very serious imprecision (CI include large differences in both directions for both outcomes).
Ganglion recurrence
For dorsal ganglia, there were 3/28 recurrences in the arthroscopic group and 2/23 in the open group. There were 3/20 recurrences in the arthroscopic group and 1/20 in the open group for volar ganglia. The pooled risk ratio was 1.7 (CI 0.45 to 6.6, 2 studies, 91 participants, I2 = 0%) (Figure 3).
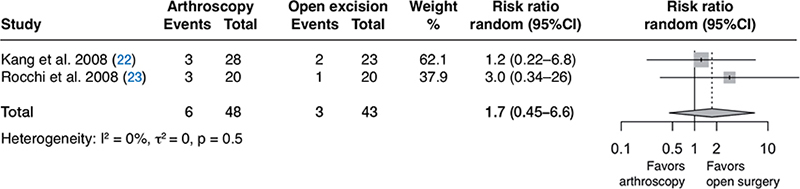
Figure 3. Forest plot of ganglion recurrence in the comparison of arthroscopic excision with open excision for wrist ganglia.
Adverse events
There were 3/48 adverse events in the arthroscopic treatment group and 7/43 in the open treatment group. The pooled risk ratio was 0.49 (CI 0.08 to 3.0, 2 studies, 91 participants, I2 = 27%).
Open reduction with arthroscopic debridement vs. open reduction alone for intra-articular fractures of the distal radius
In this comparison we identified only 1 study, and thus we did not perform a meta-analysis (24). We report the results as medians. To assess the uncertainty of the estimates, we calculated treatment effect using median value as an approximation of the mean and IQR to estimate SD. The evidence was downgraded to low due to risk of bias (lack of blinding) and imprecision.
PROM
Arthroscopic debridement probably does not provide patient-important benefits compared with no debridement (moderate certainty, downgraded for bias).
At the short-term follow-up, the median DASH score (0 to 100, higher is worse) in the open group was 23 and was 4.0 points worse (CI 13 points worse to 5.1 points better) in the arthroscopic group.
At the medium-term follow-up point, the median DASH score in the open group was 8.0 and was 2.0 points better (CI 4.2 points worse to 8.2 points better) in the arthroscopic group.
At the long-term follow-up, the median DASH score in the open group was 6.0 and was 2.0 points worse (CI 9.9 points worse to 5.9 points better) in the arthroscopic group.
The authors also measured Patient-Rated Wrist Evaluation score, showing similar treatment effect estimates.
Pain
Low certainty evidence (downgraded for bias and imprecision) indicates that the pain may not differ between the groups.
At the short-term follow-up, the median VAS score (0 to 10, higher is worse) in the open group was 2.0 points and was 1.0 point better (CI 0.2 worse to 2.2 better) in the arthroscopic group.
At the medium-term follow-up point, the median VAS score in the open group was 2.0 points and was 2.0 points better in the arthroscopic group (CI 1.2 better to 2.8 better).
Adverse events
There were 6/25 adverse events in the arthroscopic treatment group and 5/25 in the open treatment group. This corresponds with an RR of 1.2 (CI 0.42 to 3.4); very low certainty evidence due to risk of bias and very serious imprecision (confidence intervals are compatible with large benefits in either direction).
Grip strength
Grip strength was measured but only partially reported. The mean grip strength was 15 kg in the arthroscopic group and 18 kg in the open treatment group. Selles et al. reported a statistically significant p value of 0.003 for this difference (24).
Arthroscopic TFCC repair vs. supination splint for DRUJ instability with distal radius fracture
In this comparison, we identified 1 study and thus did not conduct a meta-analysis (25).
PROM
Low certainty evidence indicates that surgery may not provide benefits compared with splinting alone (downgraded for bias and imprecision). At the long-term follow-up, the mean DASH score was 14 with supination splint and 1.0 point better (CI 11 points worse to 13 better) with arthroscopic TFCC repair (1 study; 12 participants).
Adverse events
There were no adverse events reported in either group.
Discussion
Wrist arthroscopy is a promising technique with several purported advantages, but the benefits of this minimally invasive technique over open procedures or no surgery were not clearly established in this review. Patient-important benefits should be established before wide implementation because of the risks and costs associated with surgery. Furthermore, compared with open procedures, operating times can be substantially longer in arthroscopic procedures and they often require special instrumentation, thus increasing the costs (26-29). However, when used for diagnostic purposes, or if surgery is not unduly extended or additional specialized and expensive instrumentation used, non-inferiority may justify arthroscopic procedures over open procedures.
One reason that the benefits were not evident in trials could be because open procedures of the wrist can be performed through small incisions and often require, relatively speaking, little dissection. For example, a wrist ganglion can be removed from a short incision while an arthroscopic procedure requires four small incisions, and the resection in the joint capsule is likely equally extensive. Unfortunately, none of the studies comparing arthroscopy with open resection of ganglion measured patient-important benefits.
As for the possible benefits of wrist arthroscopy over no surgery, these are largely based on observational studies (30-37). For example, a systematic review assessing arthroscopic debridement for TFCC injuries identified 18 observational studies showing a mean 21-point improvement in DASH score and a 4-point decrease in pain (0 to 10 scale) after surgery (38). However, none of the studies had a control group, so we do not know if the observed improvements would have occurred without surgery. This is typical of musculoskeletal complaints (39); several high-quality RCTs that have tested the efficacy of arthroscopic surgery in other joints have shown the procedures to be no better than placebo surgery or nonsurgical alternatives (40,41). People improve also without surgery. The lack of high-quality evidence supporting the use of wrist arthroscopy leaves open whether, for many indications, the procedure is providing any benefits over nonoperative treatments.
We identified no previous reviews assessing the effect of wrist arthroscopic surgery based on randomized controlled trials. The strengths of this study are that we used a sensitive search algorithm to identify relevant studies and used no language restrictions. We also searched trial registries for unpublished trials. Thus, it is unlikely that we missed any trials, but, due to the small number of included studies, we were unable to assess the presence of publication bias. We assessed the certainty of the evidence using the GRADE approach and expressed the degree of our confidence in the presented estimates to reflect the uncertainty regarding our findings. The lack of rigorous trials limits the conclusions of this review concerning the treatment effects, and the true effects may differ substantially from the presented ones. However, this simply points to the urgent need for the kind of high-quality trials on wrist arthroscopy that have been conducted on arthroscopic procedures for other joints.
Conclusion
The current limited evidence from RCTs does not support benefits of wrist arthroscopy compared with open or non-surgical interventions. The development of arthroscopic instrumentation and implants has significantly advanced in recent years. This has allowed more complex procedures to be performed arthroscopically. These technical successes have lured many into adopting new technologies, perhaps partly out of the fear of missing out. However, this increase in uptake has not been accompanied by experimental evidence supporting the assumed benefits. Understandably, surgeons wish to adopt the most promising new techniques, and with incremental technical advancements, wrist arthroscopy might ultimately result in patient-important benefits. However, any future benefits would require evidence-based support from high-quality, low-bias, randomized controlled trials. Until such evidence arises, surgeons should acknowledge the uncertainty regarding patient benefits when recommending wrist arthroscopic procedures.
Supplementary data
The search strategy is available as supplementary data on the article home page, doi:10.2340/17453674.2023.11957
- Karelson M C, Jokihaara J, Launonen A P, Huttunen T, Mattila V M. Lower nationwide rates of arthroscopic procedures in 2016 compared with 1997 (634925 total arthroscopic procedures): has the tide turned? Br J Sports Med 2021; 55(18): 1018-23. doi: 10.1136/bjsports-2019-101844.
- Cooney W P. Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg Am 1993; 18(5): 815-22. doi: 10.1016/0363-5023(93)90047-7.
- Chloros G D, Wiesler E R, Poehling G G. Current concepts in wrist arthroscopy. Arthroscopy 2008; 24(3): 343-54. doi: 10.1016/j.arthro.2007.10.006.
- Bawale R, Singh B. A review of wrist arthroscopy of wrist surgery: an experience at a district general hospital. Orthopaedic Proceedings 2013; 95-B(SUPP_19): 32. doi: 10.1302/1358-992X.95BSUPP_19.IOSUK2011-032.
- Chloros G D, Shen J, Mahirogullari M, Wiesler E R. Wrist arthroscopy. J Surg Orthop Adv 2007; 16(2): 49-61.
- Nakamura T, Cheong Ho P, Atzei A, Corella F, Haugstvedt J R. Revolutions in arthroscopic wrist surgeries. J Hand Surg (European Volume) 2021; 47(1): 52-64. doi: 10.1177/17531934211030861.
- Ho P C, Tse W L, Wong C W yee, Hung L K. Advances in arthroscopic surgery of the wrist: from resection to reconstruction. Medicina Fluminensis 2015; 51(1): 52-89.
- Burnier M, Herzberg G, Luchetti R, Del Piñal F, Kakar S. Dry wrist arthroscopy for ulnar-sided wrist disorders. J Hand Surg Am 2021; 46(2): 133-41. doi: 10.1016/j.jhsa.2020.08.011.
- Page M J, McKenzie J E, Bossuyt P M, Boutron I, Hoffmann T C, Mulrow C D, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021 Mar 29; 372:n71. doi: 10.1136/bmj.n71
- Hudak P L, Amadio P C, Bombardier C, Beaton D, Cole D, Davis A, et al. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head). Am J Ind Med 1996; 29(6): 602-8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AIDAJIM4>3.0.CO;2-L.
- Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the Disabilities of the Arm, Shoulder and Hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther 2014; 44(1): 30-9. doi: 10.2519/jospt.2014.4893.
- Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations. GRADE Working Group; 2013, https://www.gradeworkinggroup.org/.
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010; 36(3): 1-48. doi: 10.18637/jss.v036.i03.
- Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019; 22(4): 153-60. doi: 10.1136/ebmental-2019-300117.
- R Core Team. R: A Language and environment for statistical computing. Vienna, Austria R Foundation for Statistical Computing; 2020.
- RStudio Team. RStudio: Integrated development environment for R. Boston, MA: RStudio Team; 2020.
- Higgins J P T, Altman D G, Sterne J A C. Assessing risk of bias in included studies. In: Cochrane Handbook for Systematic Reviews of Interventions Version 510; 2011. Chapter 8.
- GRADE Working Group. GRADEpro guideline development tool [software]. Hamilton, Ontario: McMaster University and Evidence Prime; 2021.
- Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am 1999; 81(8): 1093-110. doi: 10.2106/00004623-199908000-00005.
- Varitimidis S E, Basdekis G K, Dailiana Z H, Hantes M E, Bargiotas K, Malizos K. Treatment of intra-articular fractures of the distal radius. J Bone Joint Surg Br 2008; 90(6): 778-85. doi: 10.1302/0301620X.90B6.19809.
- Yamazaki H, Uchiyama S, Komatsu M, Hashimoto S, Kobayashi Y, Sakurai T, et al. Arthroscopic assistance does not improve the functional or radiographic outcome of unstable intra-articular distal radial fractures treated with a volar locking plate: a randomised controlled trial. Bone Joint J 2015; 97-B(7): 957-62. doi: 10.1302/0301-620X.97B7.35354.
- Kang L, Akelman E, Weiss A P C. Arthroscopic versus open dorsal ganglion excision: a prospective, randomized comparison of rates of recurrence and of residual pain. J Hand Surg Am 2008; 33(4): 471-5. doi: 10.1016/j.jhsa.2008.01.009.
- Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scand J Plast Reconstr Surg Hand Surg 2008; 42(5): 253-9. doi: 10.1080/02844310802210897.
- Selles C A, Mulders M A M, Colaris J W, van Heijl M, Cleffken B I, Schep N W L. Arthroscopic debridement does not enhance surgical treatment of intra-articular distal radius fractures: a randomized controlled trial. J Hand Surg Eur 2020; 45(4): 327-32. doi: 10.1177/1753193419866128.
- Lee S K, Kim K J, Cha Y H, Choy W S. Conservative treatment is sufficient for acute distal radioulnar joint instability with distal radius fracture. Ann Plast Surg 2016; 77(3): 297-304. doi: 10.1097/SAP.0000000000000663.
- del Piñal F, Klausmeyer M, Thams C, Moraleda E, Galindo C. Early experience with (dry) arthroscopic 4-corner arthrodesis: from a 4-hour operation to a tourniquet time. J Hand Surg Am 2012; 37(11): 2389-99. doi: 10.1016/j.jhsa.2012.08.026.
- Del Piñal F, Clune J. Arthroscopic management of intra-articular malunion in fractures of the distal radius. Hand Clin 2017; 33(4): 669-75. doi: 10.1016/j.hcl.2017.07.004.
- Del Piñal F. Arthroscopic volar capsuloligamentous repair. J Wrist Surg 2013; 2(2): 126-8. doi: 10.1055/s-0033-1343016.
- Tse W L, Lau S W, Wong W Y, Cheng H S, Chow C S, Ho P C, et al. Arthroscopic reconstruction of triangular fibrocartilage complex (TFCC) with tendon graft for chronic DRUJ instability. Injury 2013; 44(3): 386-90. doi: 10.1016/j.injury.2013.01.009.
- Edwards S G, Johansen J A. Prospective outcomes and associations of wrist ganglion cysts resected arthroscopically. J Hand Surgery 2009; 34(3): 395-400. doi: 10.1016/j.jhsa.2008.11.025.
- Fernandes C H, Meirelles L M, Raduan Neto J, Fernandes M, Dos Santos J B G, Faloppa F. Arthroscopic resection of dorsal wrist ganglion: results and rate of recurrence over a minimum follow-up of 4 years. Hand (N Y) 2019; 14(2): 236-41. doi: 10.1177/1558944717743601.
- Fernandes C H, Miranda C D O, dos Santos J B G, Faloppa F. A systematic review of complications and recurrence rate of arthroscopic resection of volar wrist ganglion. Hand Surg 2014; 19(03): 475-80. doi: 10.1142/S0218810414300046.
- Gallego S, Mathoulin C. Arthroscopic resection of dorsal wrist ganglia: 114 cases with minimum follow-up of 2 years. Arthroscopy 2010; 26(12): 1675-82. doi: 10.1016/j.arthro.2010.05.008.
- Mathoulin C, Hoyos A, Pelaez J. Arthroscopic resection of wrist ganglia. Hand Surg 2004; 9(2): 159-64. doi: 10.1142/s0218810404002169.
- Mathoulin C, Gras M. Arthroscopic management of dorsal and volar wrist ganglion. Hand Clin 2017; 33(4): 769-77. doi: 10.1016/j.hcl.2017.07.012.
- Rizzo M, Berger R A, Steinmann S P, Bishop A T. Arthroscopic resection in the management of dorsal wrist ganglions: results with a minimum 2-year follow-up period. J Hand Surg Am 2004; 29(1): 59-62. doi: 10.1016/j.jhsa.2003.10.018.
- Shkolnikova J, Harvey J. Wrist arthroscopy in the management of distal radius fractures. Ann Jt 2018; 3. doi: 10.21037/aoj.2018.08.06.
- Saito T, Malay S, Chung K C. A systematic review of outcomes after arthroscopic debridement for triangular fibrocartilage complex tear. Plast Reconstr Surg 2017; 140(5): 697e-708e. doi: https://dx.doi.org/10.1097/PRS.0000000000003750.
- Wartolowska K A, Gerry S, Feakins B G, Collins G S, Cook J, Judge A, et al. A meta-analysis of temporal changes of response in the placebo arm of surgical randomized controlled trials: an update. Trials 2017; 18(1): 323. doi: 10.1186/s13063-017-2070-9.
- Brignardello-Petersen R, Guyatt G H, Buchbinder R, Poolman R W, Schandelmaier S, Chang Y, et al. Knee arthroscopy versus conservative management in patients with degenerative knee disease: a systematic review. BMJ Open 2017; 7(5): e016114. doi: 10.1136/bmjopen-2017-016114.
- Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, et al. Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Ann Rheum Dis 2018; 77(2): 188 LP-195. doi: 10.1136/annrheumdis-2017-211172.
Appendix
| Author | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
| Doi et al. 1999 (19) | High | High | High | High | Unclear | Unclear | High |
| Kang et al. 2008 (22) | High | High | High | High | High | Unclear | Low |
| Lee et al. 2016 (25) | Low | Unclear | High | High | Unclear | Unclear | High |
| Rocchi et al. 2008 (23) | Low | Low | High | High | Low | Unclear | Low |
| Selles et al. 2020 (24) | Low | Low | High | High | Low | Low | Low |
| Varitimidis et al. 2008 (20) | Low | Low | High | High | Low | Unclear | Unclear |
| Yamazaki et al. 2015 (21) | Low | Low | High | Low | Low | Unclear | Low |