Total joint arthroplasty versus resection-interposition arthroplasty for thumb carpometacarpal arthritis: a randomized controlled trial
Sebastian M KLIM 1,a, Reingard GLEHR 2,a, Armin GRAEF 1, Florian AMERSTORFER 1, Andreas LEITHNER 1, and Mathias GLEHR 1
1 Department for Orthopaedics and Trauma, Medical University of Graz, Graz; 2 Institute of General Practice and Evidence-based Health Services Research, Medical University of Graz, Austria
a Shared first authorship
Background and purpose — Thumb carpometacarpal (TCMC) osteoarthritis is a common condition that causes pain and functional limitations. We compared the outcomes of 2 surgical procedures for TCMC osteoarthritis, the Epping resection-suspension arthroplasty and the double-mobility TCMC prosthesis, and focused on pain relief, functional outcomes, and patient quality of life.
Patients and methods — Over a 7-year period a randomized controlled trial including 183 cases of TCMC osteoarthritis was conducted comparing a double mobility TCMC prosthesis (Moovis, Stryker, Kalamazoo, MI, USA) with the Epping resection-suspension arthroplasty. Pre- and postoperative examinations included the range of motion (ROM), SFMcGill score, visual analogue scale (VAS), the disabilities of the arm, shoulder and hand questionnaire (DASH), and the hospital anxiety and depression scale (HADS).
Results — At the 6-week postoperative follow-up, significant differences were found in VAS: Epping median 4.0 (interquartile range [IQR] 2.0–5.0) vs. TCMC prosthesis 2.0 (IQR 0.25–4.0), p = 0.03, effect size (area under the curve [AUC]) 0.64 (95% confidence interval [CI] 0.55–0.73), in DASH score: Epping 61 (IQR 43–75) vs. TCMC prosthesis 45 (IQR 29–57), p < 0.001, AUC 0.69 (CI 0.61– 0.78), and in radial abduction: Epping 55 (IQR 50–60) vs. TCMC prosthesis 62 (IQR 60–70), p = 0.001, AUC 0.70 (CI 0.61–0.79). No significant group differences were found at the 6- and 12-months follow-up. During the follow-up period, 3 of 82 prostheses had to be revised but there was no revision in the Epping group.
Conclusion — The double mobility TCMC prosthesis had superior outcomes compared with the Epping procedure at 6 weeks; however, there were no significant differences in outcomes at 6 months and 1 year postoperatively. The implant survival rate of 96% after 12 months was acceptable.
Citation: Acta Orthopaedica 2023; 94: 224–229. DOI: https://doi.org/10.2340/17453674.2023.11919.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-08-31. Accepted: 2023-03-13. Published: 2023-05-03.
Correspondence: sebastian.klim@medunigraz.at
RG: critical review of the manuscript, data interpretation. SMK: writing of the manuscript, data interpretation. AG: data acquisition, statistical analysis. FA: data acquisition, design of the work. AL: approval of the final version, data acquisition, interpretation. MG: PI of this project, design of the work; data acquisition, revision of the draft.
Handling co-editors: Peter Frandsen and Philippe Wagner
Acta thanks Michel Boeckstyns and Teemu Karjalainen for help with peer review of this study.
For patients nonresponsive to conservative treatment for thumb carpometacarpal (TCMC) osteoarthritis, a variety of different surgical options are available. The procedures include trapeziectomy with or without tendon interposition, ligament reconstruction, and various prosthetic implants. The Epping resection-suspension arthroplasty procedure was described in 1983 to address the proximal migration of the first ray while providing pain-free grip strength without any implants (1). It is performed via a trapeziectomy followed by a flexor carpi radialis suspension-/interposition at the base of the first metacarpal bone. Despite good functional outcome and pain relief in general, weakness of thumb opposition and patient-reported postoperative persistent restriction in daily activities are described (2). Concerning grip and pinch strength compared with the contralateral side, persistent reduction initially postoperatively (2), improvement after 12 months (3), and no significant difference between the 2 sides in objective long-term examination (4) is reported in the literature. Studies comparing trapeziectomy and trapeziectomy with tendon interposition recommend trapeziectomy due to the simple technique and comparable outcome if there is no special strength requirement (5).
Endoprosthesis of the TCMC joint represents a different treatment strategy aiming at an exact reconstruction of the joint geometry. Studies report good functional outcomes and pain relief (6). Few RCTs compared the total joint arthroplasty with the interposition arthroplasty, showing similar results in both groups (7,8) or better results for the prosthesis groups (9-11). However, there are some prosthesis designs (cemented and uncemented) with high rates of loosening, luxation, and poor subjective results (12,13). To address these issues, a prosthesis was designed combining a cylindric, double-mobility cup and a hydroxyapatite-covered stem available in different sizes. The aim of our study was to compare this new prosthesis design with the Epping arthroplasty as the current standard in our institution regarding the subjective and objective functional outcome, pain relief, and patient quality of life (QOL).
Patients and methods
From November 2014 to June 2022, a prospective, randomized controlled study was conducted at our tertiary referral center for orthopedic surgery. Eligibility criteria were symptomatic rhizarthrosis grade 2 and 3 according to Eaton`s classification, failed conservative treatment prior to surgery and written informed consent to the study. Exclusion criteria were scaphotrapezotrapezoidal (STT) arthrosis and former TCMC joint surgery. Patients were provided with information on the study and were given the opportunity to express their interest in participating during the evaluation of surgical indication and collection of baseline data. Prior to surgery we employed centralized computer randomization using a webbased randomization tool that was developed and maintained by an independent statistician who was not involved in the trial (“Randomizer for Clinical Trials” tool [Medical University of Graz, Graz, Austria]) (14). The allocation sequence was kept strictly confidential and accessible only to the independent statistician and the senior author. One group received the Epping resection-suspension arthroplasty procedure, and the other group received a double-mobility TCMC joint prosthesis (Moovis, Stryker, Kalamazoo, MI, USA) without blinding. The study is reported according to CONSORT guidelines.
Outcomes
Follow-up examinations were performed 1 day, 2 weeks, 6 weeks, and 3, 6, and 12 months postoperatively by an unblinded study nurse. The primary outcome was the visual analogue scale (VAS, range 0 [no pain] to 10 [worst pain]) at 6 weeks postoperatively (15). The secondary outcomes consisted of the Disabilities of the Arm, Shoulder and Hand questionnaire (DASH, 0 [best] to 100 [worst]) as well as the measurement of thumb opposition (scale from 1 to 10) and retropulsion (scale from 1 to 3) range according to Kapandji and the maximal palmar and radial abduction using a goniometer (16,17). Further, the tip-to-tip force (between thumb and index finger) was measured in Newtons (N) using a handheld dynamometer (Cit Technics, Haren, the Netherlands). Native radiographs (anteroposterior, lateral, oblique) were performed after 6 weeks and at every consecutive follow-up examination to evaluate signs of loosening and dislocation in all patients. To record pain, we used the SF-McGill Pain questionnaire (0–55) in addition to the VAS (18). To capture quality of life (QOL) the Hospital Anxiety and Depression Scale (HADS, 0–42) was completed (19). At the 3-, 6-, and 12-month follow-up examination, patients were asked about their satisfaction concerning the success of treatment. The possible range was from “very satisfied,” “satisfied,” “not very satisfied,” and “dissatisfied.” Furthermore, the patients were asked whether they would undergo this surgical treatment again.
Surgical technique
All operations were performed by the senior author using a dorsoradial approach. During implantation of the prosthesis the TCMC joint is opened, and 3 mm of the metacarpal base and osteophytes is resected. Following the release of the trapezium the first metacarpal and the trapezium are prepared for the prosthesis by broaching and drilling. After the test implants have shown satisfying joint tension and anatomic conditions, the HA-coated stem and cup are pressfit inserted using the appropriate size, followed by the modular head. All operations were performed as described using the standard pressfit stem and cup. Depending on the surgeon’s preference, the stem is available in a standard and an anatomic design and the cup in a screw, pressfit, and cemented version. During the Epping resection-suspension arthroplasty the trapeziectomy is performed, the flexor carpi radialis tendon is divided into two parts and one of these is stripped and cut proximally. To create a suspension of the first ray, this tendon strip is pulled through a drill hole in the base of the 1st metacarpal from ulnar palmar to radial dorsal. The rest of the tendon strip is sutured to a roll replacing the os trapezium. The first ray was immobilized using an orthosis for 6 weeks postoperatively in both study groups followed by 8 weeks of physical therapy.
Statistics
The primary endpoint (VAS pain at 6 weeks after the operation) was analyzed using the Mann–Whitney U-test. Secondary endpoints were analyzed with all other parameters as an exploratory analysis. The analysis specifies the exact number of joints per patient (1 or 2). Appropriate methods were applied to account for dependence when 2 joints were used. P-values were adjusted where necessary using the Holm–Bonferroni method. This adjustment was done for each variable separately to account for measurements at different time points but not on a global level as the analysis was exploratory. To account for the longitudinal nature of the data, linear mixed-effect models were employed where appropriate. Ordinal variables and variables measured with limited precision were analyzed using nonparametric tests, without assuming normality. To provide information on the relevance of the observed effects, treatment effects were calculated including confidence intervals (CI) of group differences in mixed-effect models (where applicable) and area under the curve (AUC) for ordinal variables. Boxplots were employed to visually represent longitudinal results. As all patients were treated according to their original randomization, there was no difference between the intention-to-treat and per protocol analysis. While there were some missing values in the follow-up data of our study, we made a conscious decision to include all patients due to their significant value to the study. We have taken steps to mitigate the impact of the missing data and used appropriate statistical methods to account for the uncertainty. The samples size was based on pilot study data. The statistical significance level was set at p < 0.05. Statistical analyses were performed using R (version 4.2.1; R Foundation for Statistical Computing, Vienna, Austria).
Ethics, registration, data sharing, funding, and disclosures
This study was conducted at the Medical University of Graz (Austria) and approved by the institutional review board (26-543 ex 13/14). Source data is available on reasonable request. The study is registered on clinicaltrials.gov (NCT05267964). Informed consent was obtained from all individual participants included in the study. This study was supported by a study nurse grant from Stryker Corp. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.11919
Results
There were 183 consecutive cases of TCMC osteoarthritis in 169 patients (in 14 patients, surgery was performed on both TCMC joints; Figure 1). During the study, 3 joints in the TCMC prosthesis group had to be revised. This was due to a polyethylene inlay dislocation 10 months postoperatively, cup loosening caused by osteonecrosis of the trapezium after 7 months, and due to a head dislocation on the second postoperative day. In 1 case, a clinically inconspicuous decentration of the prosthesis head was detected (no revision necessary). 2 cases of a tenovaginitis de Quervain occurred after implantation of the prosthesis, which was treated surgically by splitting the first extensor tendon compartment (3 and 7 months following index surgery). Preoperative baseline patient characteristics, score and measurement results regarding functional outcome, strength, level of pain, and QOL of both groups are described in Table 1.
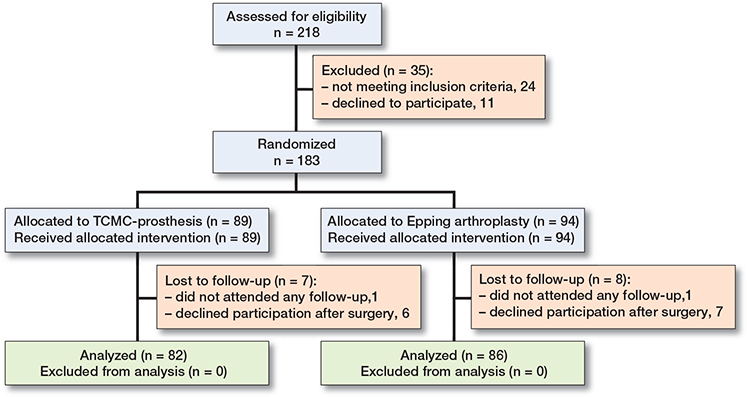
Figure 1. Flowchart depicting patient inclusion, randomization, and loss-to-follow-up.
Primary and secondary outcomes
The confirmatory analysis of the primary endpoint (VAS at 6 weeks postoperatively) including 1 joint per patient showed a significantly worse result for the Epping group compared with the TCMC prosthesis group (p = 0.005). Postoperative score results of both groups were as described in Table 2. Significant secondary outcome differences were observed at 6 weeks and 3 months postoperatively (SF-McGill, DASH score) as depicted in Figure 2. The study revealed 2 notable differences in terms of function between the 2 groups. The radial abduction was found to be better in the TCMC prosthesis group than in the Epping group at 6 weeks (Epping 55° [IQR 50–60] vs. TCMC prosthesis 62° [IQR 60–70]; p = 0.001; effect size [AUC] 0.70 [CI 0.61–0.79]) and at 3 months (Epping 60° [IQR 60–70] vs. TCMC prosthesis 70° [IQR 65–70]; p = 0.009; effect size [AUC] 0.67 [CI 0.58–0.75]). At 3 months, there was significantly better thumb retropulsion in the TCMC prosthesis group than in the Epping group: Epping (scale 0 = 4 [5.8%], 1 = 18 [26%], 2 = 27 [39%], 3 = 20 [29%]) versus TCMC prosthesis (scale 0 = 1 [1.4%], 1 = 11 [15%], 2 = 18 [25%], 3 = 41 [58%]); p = 0.02; effect size (AUC) 0.65 (CI 0.56–0.74). There were no other significant differences between the groups in the follow-up examinations. Most participants were either “very satisfied” (Epping 49% vs. TCMC prosthesis 69%) or “satisfied” (Epping 42% vs. TCMC prosthesis 21%) regarding the course and outcome of the surgical treatment. At 12 months, 81% of the Epping group and 92% of the TCMC prosthesis group would opt again for surgical treatment. There were no significant group differences regarding these questionnaires.
| Characteristic | Epping arthroplasty, n = 86 | TCMC prosthesis, n = 82 | p-value a | Effect size AUC (95% CI) |
||||
| Missing, n | median (IQR) | [range] | Missing, n | median (IQR) | [range] | |||
| VAS pain | ||||||||
| 1 day | 9 | 3.0 (2.0–7.0) | [0.0–10] | 6 | 3.0 (1.0–5.0) | [0.0–10] | 0.8 | 0.51 (0.41–0.61) |
| 2 weeks | 10 | 2.0 (1.0–4.0) | [0.0–10] | 10 | 1.0 (0.0–3.0) | [0.0–8.0] | 0.1 | 0.62 (0.53–0.71) |
| 6 weeks | 14 | 4.0 (2.0–5.0) | [0.0–10] | 8 | 2.0 (0.25–4.0) | [0.0–10] | 0.03 | 0.64 (0.55–0.73) |
| 3 months | 7 | 2.0 (1.0–4.0) | [0.0–10] | 5 | 1.0 (0.0–3.0) | [0.0–8.0] | 0.2 | 0.59 (0.50–0.69) |
| 6 months | 10 | 1.5 (0.75–3.0) | [0.0–10] | 8 | 1.0 (0.0–2.8) | [0.0–8.0] | 0.3 | 0.58 (0.49–0.68) |
| 12 months | 12 | 1.0 (0.0–3.0) | [0.0–8.0] | 3 | 0.0 (0.0–2.0) | [0.0–7.0] | 0.4 | 0.57 (0.48–0.66) |
| SF-McGill | ||||||||
| 1 day | 3 | 16 (6–24) | [0–42] | 2 | 10 (5–19) | [0–44] | 0.3 | 0.58 (0.48–0.67) |
| 2 weeks | 3 | 8 (4–17) | [0–52] | 3 | 5 (1–9) | [0–42] | 0.05 | 0.62 (0.53–0.71) |
| 6 weeks | 3 | 10 (5–20) | [0–39] | 2 | 7 (3–11) | [0–32] | 0.01 | 0.65 (0.56–0.74) |
| 3 months | 2 | 9 (4–16) | [0–41] | 1 | 7 (1–13) | [0–35] | 0.03 | 0.63 (0.54–0.72) |
| 6 months | 2 | 5 (2–11) | [0–35] | 3 | 3 (0–8) | [0–39] | 0.3 | 0.57 (0.48–0.66) |
| 12 months | 2 | 3 (0–9) | [0–41] | 1 | 2 (0–8) | [0–34] | 0.4 | 0.54 (0.45–0.63) |
| HADS-D | ||||||||
| 3 months | 7 | 8 (4–14) | [0–30] | 9 | 5 (1–12) | [0–30] | 0.2 | 0.60 (0.50–0.69) |
| 6 months | 11 | 8 (3–14) | [0–29] | 11 | 5 (1–10) | [0–29] | 0.2 | 0.59 (0.49–0.69) |
| 12 months | 10 | 8 (2–16) | [0–29] | 5 | 5 (1–12) | [0–37] | 0.2 | 0.58 (0.48–0.67) |
| DASH | ||||||||
| 6 weeks | 11 | 61 (43–75) | [5–100] | 7 | 45 (29–57) | [0–91] | < 0.001 | 0.69 (0.61–0.78) |
| 3 months | 5 | 38 (22–55) | [3–88] | 5 | 24 (12–41) | [0–99] | 0.001 | 0.68 (0.59–0.76) |
| 6 months | 8 | 26 (12–47) | [0–80] | 8 | 16 (8–29) | [0–75] | 0.07 | 0.60 (0.51–0.70) |
| 12 months | 9 | 18 (6–34) | [0–84] | 5 | 10 (4–26) | [0–68] | 0.09 | 0.58 (0.49–0.68) |
| a Mann–Whitney U-test with Holm–Bonferroni correction and AUC calculated for first intervention per patient. | ||||||||
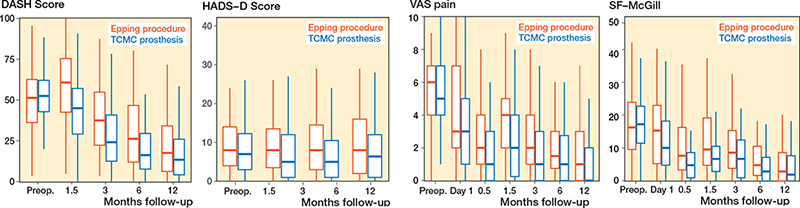
Figure 2. Display of the longitudinal course of the DASH, HADS-D, VAS pain and SF-McGill scores over the study period. Horizontal lines are median, box are IQR, and whiskers are 1.5 x IQR.
Linear mixed-effect models
The linear mixed-effect models were calculated including all operated joints. The effect of the TCMC prosthesis compared with the Epping on the DASH score, adjusted for the preoperative value, was evaluated with pointwise 95% CIs. The simultaneous CIs (adjusted for multiple comparisons using Bonferroni correction) did not cover zero at 6 weeks (CI –22 to –8.1) and 3 months (CI –18 to –3.6), indicating significant differences between the groups. At 6 months and 12 months, the CIs covered zero, indicating no significant differences between the groups. The effect of the TCMC prosthesis compared with the Epping on the SF-McGill score was assessed accordingly. The simultaneous CIs did not cover zero at 2 weeks (CI –8.7 to –1.9), 6 weeks (CI –7.6 to –2.1), and 3 months (CI –6.1 to –0.50), indicating significant differences between the groups.
Discussion
The present study compared QOL and functional outcomes of the Epping arthroplasty and TCMC prosthesis and found a significantly better outcome in terms of pain (VAS), disability (DASH score), and quality of life (SF-McGill score) for the TCMC prosthesis group at 6 weeks and 3 months after surgery. The study also showed a significantly better outcome for the TCMC prosthesis group in terms of radial abduction and thumb retropulsion. However, no significant differences could be found 1 year postoperatively. Most participants in both groups were satisfied with the outcome of the surgery and would opt to redo the procedure.
Our results are partly consistent with former comparisons of total joint and interposition arthroplasty, providing better pain relief (9,10), a better QuickDASH score (9) and higher patient satisfaction (9,10). Cebrian-Gomez et al. and Ulrich-Vinther et al. show a faster convalescence too (9,10), Ulrich-Vinther et al. (10) and Jurca et al. (11) additionally report stronger grip functions, and an improved range of motion, which is consistent with our findings of better range of thumb retropulsion in the prosthesis group. However, our data show these significant differences only in the short-term follow-up examination after 6 weeks and 3 months. A difference after 6 months and 1 year could not be found. Robles-Molina et al. (7) show better pinch strength and range of motion in the prosthesis group, but no difference in pain relief and functional improvement. In a long-term survey by Vandenberghe et al. (8), no difference in pain or function was found between the 2 groups, which were rather unequally selected as the authors confirm. We could not find any other comparison of total joint and interposition arthroplasty using the Moovis system.
During the 12-month follow-up period, 3 joints (4%) in the TCMC prosthesis group had to be revised due to 1 cup loosening and 2 cases of dislocation (polyethylene and head). A large systematic review including 32 articles concerning 19 different implants identified the same causes (loosening and dislocation) to be the most frequent complications in total TCMC joint arthroplasty. Failure rates varied between zero and 44% depending on the prosthesis design (20). Authors have described various reasons for aseptic loosening with prosthesis malposition and patient selection being among the most frequent (21). The choice of implant fixation, cemented or pressfit, does not seem to have a major influence on loosening rates. Studies report low as well as high failure rates for both fixation methods, mainly depending on the prosthesis type (6,8,22-25).
Strengths and limitations
2 major advantages of the present study should be highlighted. On the one hand, this study was planned and conducted as a randomized controlled trial with the operations being performed by a single surgeon. On the other hand, we included a total of 183 cases with a loss to follow-up rate of 8%, which makes this trial one of the largest of its kind (20). These facts contribute significantly to the validity and value of the reported results.
However, we also want to acknowledge the following limitations to this work. The follow-up time of 12 months does not allow a conclusion on mid- and long-term stability of the TCMC joints (aseptic loosening, dislocation). Because this is one of the major problems of past and current TCMC prosthesis designs, a long-term follow-up evaluation needs to be awaited. The Moovis implant survival rate was 96% at 12 months’ follow-up. While missing data can introduce bias into study results, we believe that including all patients is more valuable than excluding those with missing data. Our statistical methods were selected to account for the uncertainty introduced by missing data, and we believe they have helped to mitigate the impact of missing data on our results. We believe that our efforts to address missing data have improved the quality of our study and increased its reliability. Nevertheless, we acknowledge that missing data is a limitation of our study that cannot be fully eliminated.
Further we have encountered a considerable age difference between the 2 study groups despite the randomization as described in Table 1. For the authors, the only conclusive explanation for this is the final group size of 168 patients, which could not ensure a completely identical cohort allocation, and therefore the age difference is due to chance. Another limitation of this study is the lack of blinding of the participants and the study nurse who conducted the follow-up examinations, as this was not possible in the framework of our outpatient department.
Conclusion
We found superior outcomes at 6 weeks and 3 months after surgery for the double mobility TCMC prosthesis compared with interposition arthroplasty in terms of pain and function. However, there were no significant differences in outcomes after 6 months and 1 year. The implant survival rate of 96% after 12 months is considered acceptable, and both methods showed favorable results.
- Epping W, Noack G. (Surgical treatment of the saddle joint arthrosis). Handchir Mikrochir Plast Chir 1983; 15(3): 168.
- Wittemann M, Demir E, Sauerbier M, Germann G. (The Epping resection-suspension arthroplasty procedure: a standard procedure in the operative treatment of trapeziometacarpal osteoarthrosis?). Handchir Mikrochir Plast Chir 2002; 34(1): 49. doi: 10.1055/s-2002-22108.
- Krein R, Richter M, Brüser P. (Does Epping resection arthroplasty lead to loss of hand strength? A prospective study). Handchir Mikrochir Plast Chir 2001; 33(3): 171. doi: 10.1055/s-2001-15125.
- Klein S M, Wachter K, Koller M, Vykoukal J, Geis S, Dolderer J H, et al. Long-term results after modified Epping procedure for trapeziometacarpal osteoarthritis. Arch Orthop Trauma Surg 2015; 135(10): 1475. doi: 10.1007/s00402-015-2307-6.
- Liu Q, Xu B, Lyu H, Lee J H. Differences between simple trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition for the treatment of trapeziometacarpal osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg 2022; 142(6): 987. doi 10.1007/s00402-020-03707-w
- Lemoine S, Wavreille G, Alnot J Y, Fontaine C, Chantelot C. Second generation GUEPAR total arthroplasty of the thumb basal joint: 50 months follow-up in 84 cases. Orthop Traumatol Surg Res 2009; 95(1): 63. doi: 10.1016/j.otsr.2008.06.001.
- Robles-Molina M J, Lopez-Caba F, Gomez-Sanchez R C, Cardenas-Grande E, Pajares-Lopez M, Hernandez-Cortes P. Trapeziectomy with ligament reconstruction and tendon interposition versus a trapeziometacarpal prosthesis for the treatment of thumb basal joint osteoarthritis. Orthopedics 2017; 40(4): e681. doi 10.3928/01477447-20170503-03.
- Vandenberghe L, Degreef I, Didden K, Fiews S, De Smet L. Long term outcome of trapeziectomy with ligament reconstruction/tendon interposition versus thumb basal joint prosthesis. J Hand Surg Eur 2013; 38(8): 839. doi 10.1177/1753193412469010.
- Cebrian-Gomez R, Lizaur-Utrilla A, Sebastia-Forcada E, Lopez-Prats F A. Outcomes of cementless joint prosthesis versus tendon interposition for trapeziometacarpal osteoarthritis: a prospective study. J Hand Surg Eur 2019; 44(2): 151. doi 10.1177/1753193418787151.
- Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am 2008; 33(8): 1369. doi: 10.1016/j.jhsa.2008.04.028.
- Jurča J, Němejc M, Havlas V. (Surgical treatment for advanced rhizarthrosis. comparison of results of the Burton–Pellegrini technique and trapeziometacarpal joint arthroplasty). Acta Chir Orthop Traumatol Cech 2016; 83(1): 27.
- Kaszap B, Daecke W, Jung M. High frequency failure of the Moje thumb carpometacarpal joint arthroplasty. J Hand Surg Eur 2012; 37(7): 610. doi: 10.1177/1753193412454252.
- Pérez-Ubeda M J, García-López A, Marco Martinez F, Junyent Vilanova E, Molina Martos M, López-Duran Stern L. Results of the cemented SR trapeziometacarpal prosthesis in the treatment of thumb carpometacarpal osteoarthritis. J Hand Surg Am 2003; 28(6): 917. doi: 10.1016/s0363-5023(03)00378-2.
- Medical University of Graz. Randomizer. http://www.randomizer.at/ (Accessed November 1, 2014).
- McCormack H M, Horne D J, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med 1988; 18(4): 1007. doi :10.1017/s0033291700009934.
- Kapandji A. (Clinical test of apposition and counter-apposition of the thumb). Ann Chir Main 1986; 5(1): 67. doi 10.1016/s0753-9053(86)80053-9.
- Hudak P L, Amadio P C, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) (corrected). The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996; 29(6): 602. doi: 10.1002/(sici)1097-0274(199606)29:6<602::Aid-ajim4>3.0.Co;2-l.
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1(3): 277, 1975, doi: 10.1016/0304-3959(75)90044-5
- Zigmond A S, Snaith R P. The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6): 361, 1983,
- Huang K, Hollevoet N, Giddins G. Thumb carpometacarpal joint total arthroplasty: a systematic review. J Hand Surg Eur 2015 ; 40(4): 338. doi: 10.1177/1753193414563243.
- Hess D E, Drace P, Franco M J, Chhabra A B. Failed thumb carpometacarpal arthroplasty: common etiologies and surgical options for revision. J Hand Surg Am 2018; 43(9): 844. doi: 10.1016/j.jhsa.2018.03.052.
- Wachtl S W, Guggenheim P R, Sennwald G R. Cemented and non-cemented replacements of the trapeziometacarpal joint. J Bone Joint Surg Br 1998; 80(1): 121. doi: 10.1302/0301-620x.80b1.7941.
- De Smet L, Sioen W, Spaepen D, van Ransbeeck H. Treatment of basal joint arthritis of the thumb: trapeziectomy with or without tendon interposition/ligament reconstruction. Hand Surg 2004; 9(1): 5. doi: 10.1142/s0218810404001942.
- Regnard P J. Electra trapezio metacarpal prosthesis: results of the first 100 cases. J Hand Surg Br 2007; 31: 621. doi: 10.1016/j.jhsb.2006.05.019.
- Hansen T B, Stilling M. Equally good fixation of cemented and uncemented cups in total trapeziometacarpal joint prostheses: a randomized clinical RSA study with 2-year follow-up. Acta Orthop 2013; 84(1): 98. doi: 10.3109/17453674.2013.765625.