The natural history of acetabular dysplasia and later total hip arthroplasty in late-detected DDH: 48 patients with closed reduction followed to a mean age of 62 years
Terje TERJESEN
Section of Children’s Orthopaedics and Reconstructive Surgery, Division of Orthopaedic Surgery, Oslo University Hospital, Rikshospitalet, and University of Oslo, Oslo, Norway
Background and purpose — The long-term prognosis of acetabular dysplasia without subluxation in developmental dislocation of the hip (DDH) is uncertain. The aim of this study was to assess the consequence of having acetabular dysplasia at skeletal maturity on the need for having a total hip arthroplasty (THA) up to the age of 60 years.
Patients and methods — Inclusion criteria were age at diagnosis 0.5–3.0 years, initial treatment with skin traction to obtain closed reduction during 1958–1962, and no acetabular procedures to improve femoral head coverage. 48 patients (57 hips) met these criteria, 41 girls and 7 boys. Hip dysplasia was defined as a center–edge (CE) angle at skeletal maturity of 10–19°, and hips with CE angles in the range 20–25° were termed borderline dysplastic.
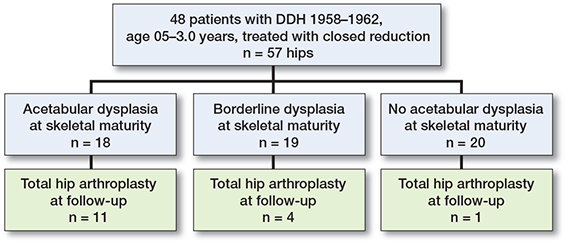
Results — At skeletal maturity, 18 hips had acetabular dysplasia with a mean CE angle of 15.8° (10–19), whereas 19 hips were borderline with CE angles 20–25°, and 20 hips were normal (CE angles ≥ 26°). During the follow-up period 16 hips had undergone THA, 11 of 18 hips with dysplasia, 4 of 19 with borderline dysplasia, and 1 of 20 hips without dysplasia (p < 0.001). Hip survival in the 18 dysplastic hips, with THA as the endpoint, was 100% up to patient age 40 years; thereafter survival fell to 83% at 50 years and 39% at 60 years. There was no significant correlation between CE angle at skeletal maturity and age at THA (p = 0.2). The mean age at the last follow-up in patients without THA was 62 years (60–64).
Conclusion — Acetabular dysplasia without subluxation was a risk factor for THA, but less than one-fifth of the hips had undergone THA up to patient age 50 years.
Citation: Acta Orthopaedica 2023; 94: 152–157. DOI https://doi.org/10.2340/17453674.2023.11664.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-02. Accepted: 2023-03-02. Published: 2023-04-13.
Correspondence: terje.terjesen@rikshospitalet.no
TT planned the study, analyzed the data, and wrote the manuscript.
The author would like to thank the photographer Øystein Horgmo for help with the illustrations.
Handling co-editors: Ilkka Helenius and Robin Christensen
Acta thanks Federico Canavese and Carl Johan Tiderius for help with peer review of this study.
The initial treatment of late-detected dislocation of the hip (DDH) is open or closed hip reduction, with or without preliminary traction. Successful outcome means that the hip should last a lifetime, with avoidance of osteoarthritis (OA) and total hip arthroplasty (THA). In cases of persistent hip dysplasia with reduced femoral head coverage during childhood and adolescence, additional surgery such as pelvic osteotomy or hip shelf operation may be indicated to improve the outcome at skeletal maturity and later (1-3). There is, however, no agreement regarding the need for these operations.
A prerequisite when defining indications for pelvic surgery is knowledge of the natural history of patients with acetabular dysplasia with or without subluxation. Such a study based on patients from our hospital was published some years ago (4) and showed that hip subluxation at skeletal maturity was a risk factor for development of OA during the follow-up period of 44 years, which confirmed previous studies (5,6). The association between acetabular dysplasia without subluxation and later OA was weaker, which calls for further studies.
OA after late-detected DDH increases with the length of follow-up, but the rates of OA and THA vary (7-10). Survival analysis with conversion to THA as the endpoint requires long follow-up. Thomas et al. (8) reported on late-detected DDH treated with open reduction and Salter-type pelvic osteotomy and found that the survival rate decreased markedly (from 86% to 54%) between 40 and 45 years’ follow-up. Such a rapid deterioration was not confirmed in another study on patients treated with preliminary traction and closed reduction (4). Thus, the pattern of hip survival after various treatment strategies needs more studies with longer follow-up.
The present study among children treated for late-detected DDH before the age of 3 years has longer follow-up than previous studies and includes only patients without late pelvic surgery to correct acetabular dysplasia. The primary aim was to compare the consequence of having acetabular dysplasia without subluxation at skeletal maturity, relative to those without, on the need for a THA up to the age of 60 years.
Patients and methods
Patients in this retrospective study were recruited from the period 1958–1962 through a search of the diagnosis card index for DDH at Sophies Minde Orthopaedic Hospital (now a division of Oslo University Hospital). The inclusion criteria were no associated anomaly, no neuromuscular disorder, no previous treatment in other hospitals, age at diagnosis 0.5–3.0 years, initial treatment with skin traction to obtain closed hip reduction, and no concurrent or later pelvic procedures (osteotomy or shelf operation) to improve femoral head coverage. 48 patients (57 hips) met these criteria, 41 girls and 7 boys with a mean age of 1.4 years (0.5–2.8) at diagnosis. DDH was unilateral in 39 patients and bilateral in 9. The left side was affected more often than the right side (37 vs 20). 45 hips had total dislocation and 12 had subluxation with femoral head coverage < 50%.
The patients were initially treated with bilateral longitudinal skin traction to obtain gradual closed reduction, as previously described (11). The average time in traction was 33 days (16–65). The mean age at spica cast application was 1.6 years (0.7–3.1). 27 hips were reduced at patient age < 1.5 years and 30 hips at age ≥ 1.5 years. Hip spica was used for a mean period of 9.3 months (6–15). The spica was changed every 3 months. Because of femoral valgus or increased femoral anteversion, later proximal femoral osteotomy (with varus and/or derotation) was performed in 10 hips at a mean patient age of 13 years (6–19).
The study is reported according to STROBE guidelines.
Radiographic evaluation (Figure 1)
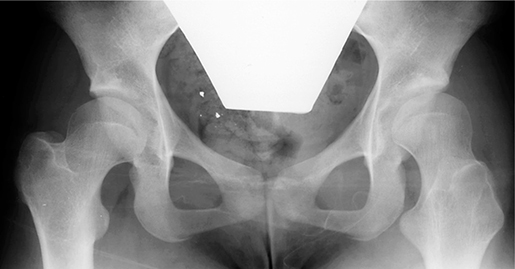
Conventional anteroposterior radiographs of the pelvis at skeletal maturity or later were available in all except 1 patient (who was 11.2 years at the last radiographic follow-up). Skeletal maturity was defined as patient age ≥ 15 years, when the physes of the proximal femur and acetabulum were closed. The mean patient age (except the patient mentioned above) was 26 years (15–56). A radiograph showing the pelvis and both hips was taken with the patient in the supine position, and care was taken to position the patient with the legs parallel and to avoid rotation of the pelvis and hips. The old radiographs (from diagnosis of DDH until 2002 when PACS was introduced at our hospital) were digitized for the current analysis. The radiographic assessment was performed by the author, who has long experience in evaluation of radiographs of hips in children and adults. The center–edge (CE) angle was measured as described by Wiberg (5), using the most lateral point of the acetabular roof as landmark (Figure 1). Femoral head coverage was also assessed by the migration percentage (MP) according to Reimers (12) using the same acetabular landmark as for the CE angle (Figure 1). The hip is located if the MP is < 33%, subluxated if it is 33–89%, and dislocated if MP is ≥ 90%. Avascular necrosis of the femoral head (AVN) was assessed according to Kalamchi and MacEwen (13). The radiographic outcome at skeletal maturity was evaluated using the classification of Wiberg (5). CE angle < 20° means acetabular dysplasia, CE angle 20–25° means borderline dysplasia, whereas normal hips have a CE angle > 25°. Subluxation was for the present study defined as a CE angle < 10º and a broken Shenton line. A case with follow-up is presented in Figure 2.

Figure 1. CE (center–edge) angle is the angle between 2 lines through the center of the femoral head (right hip): the perpendicular to the inter-teardrop line and the line from the center to the lateral acetabular rim. MP (migration percentage, left hip); it is the percentage of the femoral head lateral to Perkins’ line (a/b x 100).
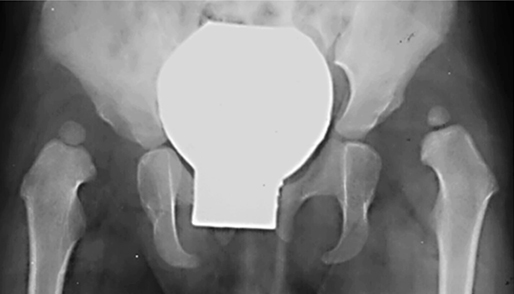
Figure 2. A. A 20-month-old girl with bilateral hip dislocation. She was initially treated with skin traction (30 days) to obtain closed reduction and thereafter hip spica cast for 12 months (the spica cast was changed every 3 months).
B. The same patient at skeletal maturity (age 15 years) with acetabular dysplasia in both hips, with CE angles 18° in the right hip and 17° in the left. A few days after this radiograph, a femoral inter-trochanteric osteotomy (derotation and varization) was performed in the left hip.

C. The patient at age 52 years. The dysplasia is unchanged compared with that in Figure 2 B. There is no sign of osteoarthritis and the patient had no hip complaints. No THA had been performed at the age of 61 years.
Information regarding THA was provided by the Norwegian Arthroplasty Register (NAR), which started registration of THA in Norway in 1988. NAR has a registration completeness of 97% (14). The data was received in June 2022 with information on whether or not the patients had undergone THA and the date at the time of THA.
Statistics
SPSS (version 28) was used for statistical analysis (IBM Corp, Armonk, NY, USA). Categorical data were analyzed with the Pearson chi-square test. Continuous variables were analyzed using the t-test for independent samples. For correlation between parameters, Pearson’s correlation coefficient (r) was used. All tests were 2-sided. Differences were considered significant when the p-value was < 0.05. Kaplan–Meier survival analysis with conversion to THA as endpoint was used to assess the long-term prognosis.
Ethics and disclosures
The study was approved by the Regional Committee of Medical Research Ethics (ref. 2012/1761b) and our institutional review board, and informed consent was received from all the patients. There are no conflicts of interests. A completed disclosure form for this article following the ICMJE template is available on the article page, doi: 10.2340/17453674.2023.11664.
Results
20 hips were normal at skeletal maturity, with a mean CE angle of 30° (26–36) and a mean MP of 18% (6–23). 19 hips had borderline acetabular dysplasia, with a mean CE angle of 22° (20–25) and a mean MP of 24% (10–30). 18 hips had acetabular dysplasia, with a mean CE angle of 16° (10–19) and a mean MP of 31% (22–37). The correlation coefficient between CE angle and MP was –0.82 (p < 0.001), indicating a very good correlation between the methods in assessing the femoral head coverage.
16 hips had undergone THA (Figure 3). Significant risk factors for THA were acetabular dysplasia at skeletal maturity and avascular necrosis (AVN) of the femoral head (Table 1). The mean CE angle at skeletal maturity was 18° (SD 4.0) in hips with later THA and 25° (SD 5.6) in hips without THA (p < 0.001). THA had been performed in 1 out of 20 normal hips, in 4 of 19 hips with borderline dysplasia, and in 11 of 18 hips with hip dysplasia. The difference between the dysplastic hips and the other groups was significant (p < 0.001). Although the percentage of THA was greater in the borderline hips than in the normal hips (Table 1), the numbers of hips were too small for meaningful statistical analysis. In the 18 dysplastic hips, there was no significant difference in CE angle at skeletal maturity between the 11 hips that had undergone THA and the 7 hips without THA (p = 0.7).
| Parameters | THA | |||
| n | No | Yes | p-value a | |
| Grade of DDH | 0.8 | |||
| Complete dislocation | 45 | 32 | 13 | |
| Subluxation | 12 | 9 | 3 | |
| Laterality of DDH | 0.5 | |||
| Unilateral | 39 | 29 | 10 | |
| Bilateral | 18 | 12 | 6 | |
| Age at hip reduction | 0.1 | |||
| < 1.5 years | 27 | 22 | 5 | |
| ≥ 1.5 years | 30 | 19 | 11 | |
| AVN | 0.004 | |||
| No | 54 | 41 | 13 | |
| Yes | 3 | 0 | 3 | |
| CE angle b | < 0.001 | |||
| < 20° | 18 | 7 | 11 | |
| 20°–25° | 19 | 15 | 4 | |
| > 25° | 20 | 19 | 1 | |
| aChi-square test. | ||||
| bCenter–edge angle at skeletal maturity-DDH = developmental dislocation of the hip AVN = avascular necrosis of the femoral head | ||||
The mean patient age at THA was 53 years (41–61), 52 years in hips with acetabular dysplasia, 55 years in hips with borderline dysplasia, and 56 years in the 1 normal hip. The correlation between CE angle at skeletal maturity and age at THA was not statistically significant (r = 0.35; p = 0.2).
The mean age at the last follow-up in patients who had not undergone THA was 62 years (60–64). Kaplan–Meier survival analyses with conversion to THA as endpoint are presented in Table 2 and Figure 4. Survival was 100% until patient age 40 years and then decreased slightly to 95% at 50 years. Then, a more pronounced decrease was seen, ending with a survival rate of 74% at patient age 60 years. In order to assess the significance of increasing age at hip reduction, survival analysis was separately performed in the 30 patients who were ≥ 1.5 years (range 1.5–3.1) at reduction. This group had similar hip survival rate to the total material until age 40 years. Thereafter, survival was 5% lower at age 50 years and 7% lower at age 60 years (Table 2).
| Patient age a | Total material 57 hips | Age b ≥ 1.5 years | CE angle < 20° 18 hips | CE angle 20–25° 19 hips | CE angle > 25° 20 hips |
| 40 | 100 | 100 | 100 | 100 | 100 |
| 45 | 97 (92–100) | 93 (84–100) | 89 (74–100) | 100 | 100 |
| 50 | 95 (89–100) | 90 (79–100) | 83 (65–100) | 95 (85–100) | 100 |
| 55 | 86 (77–95) | 80 (66–94) | 67 (45–89) | 90 (77–100) | 95 (85–100) |
| 60 | 74 (63–85) | 67 (50–84) | 39 (16–62) | 80 (62–98) | 95 (85–100) |
| aPatient age at follow-up. | |||||
| bPatient age at hip reduction. | |||||
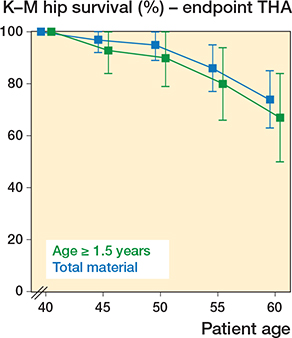
Figure 4. Kaplan–Meier survival analysis (with 95% confidence intervals) with total hip arthroplasty as the endpoint in all 57 hips and in the 30 hips of patients ≥ 1.5 years at the time of hip reduction.
The lowest hip survival rates occurred in the 18 hips with CE angle < 20°at skeletal maturity (Table 2; Figure 5). Survival decreased from 100% at patient age 40 years, to 83% at 50 years, and 39% at 60 years. In the hips with borderline dysplasia, survival rates were high: 95% at patient age 50 years and 80% at age 60 years.
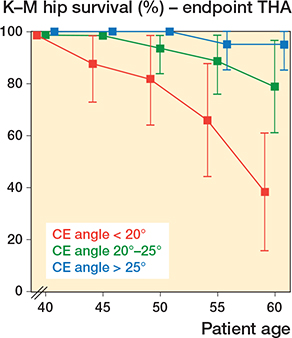
Figure 5. Kaplan–Meier survival analysis with THA as the endpoint according to 3 categories of CE angles at skeletal maturity: dysplastic hips with CE angle < 20°, borderline hips with CE angle 20–25°, and normal hips with CE angle > 25°.
Discussion
The characteristics of the present study were initial skin traction to obtain gradual closed reduction, no pelvic operations to correct acetabular dysplasia, and available radiographs at skeletal maturity or later. With follow-up to patient age ≥ 60 years, the study probably represents the longest follow-up of DDH to date. The main results were that 1/5 with dysplasia and 1/20 with borderline dysplasia received a THA. The overall hip survival (with THA as the endpoint) was very good (≥ 90%) until patient age 50 years, and acetabular dysplasia without subluxation was a risk factor for THA.
Acetabular dysplasia with or without subluxation is not uncommon after treatment of late-detected DDH (6,9). Previous studies, where no corrective pelvic surgery had been performed, have shown that subluxation is a clear risk factor for later OA (5,7,15). There is also an association, although weaker, between less severe abnormalities (acetabular dysplasia without subluxation) and later OA. Wiberg (5) reported on 17 patients with dysplasia and found a linear relationship between the CE angle and the age at OA onset. 7 hips were subluxated (mean CE angle 2°) and all of these developed OA at a mean age of 42 years. The remaining 10 hips that were not subluxated developed OA at a mean age of 57 years. This pattern of OA was not confirmed by Cooperman et al. (15), who studied 32 hips with acetabular dysplasia, but without subluxation (“an essentially intact Shenton’s line”). They found that almost all patients developed OA, but there was no linear relationship between the CE angle and the age at which OA developed. Our results were in accordance with those of Cooperman et al. (15). With a follow-up to patient age > 60 years, the rate of THA was high (61%), but there was no significant relationship between the CE angle and the age at THA.
Survival rates with THA as the endpoint vary considerably, probably because of differences in age at diagnosis of DDH, initial treatment policy, later additional surgical procedures, and follow-up time. Thomas et al. (8) studied patients who were > 1.5 years of age at the time of open reduction and simultaneous Salter type pelvic osteotomy. The survival rate fell from 99% at patient age 33 years to 54% at 48 years. The reduction in survival was no less than 32% between the age of 43 and 48 years. Such a large reduction in the same age span has not been confirmed in other studies of pelvic osteotomies (9,16).
The long-term hip survival rates in the present dysplastic hips were compared with those after periacetabular osteotomy (PAO) (Table 3). Between patient age 40 and 50 years, hip survival decreased by approximately 27% after PAO and 17% without PAO. The greatest decrease of survival in the hips with no PAO (present study) was 44% between the ages of 50 and 60 years. In this age span, a decrease of 32% after PAO was found (9). The long-term studies featured in Table 3 indicate that the survival rate is good (86–100%) up to age 40 years and thereafter a pronounced deterioration occurs, no matter whether or not late pelvic osteotomies have been performed. Thus, to study the true outcome of different treatment concepts, a follow-up to patient age 60 years is desirable.
This study has several limitations. First, it was retrospective and there was no control group. Second, the number of patients was rather limited, especially in the subgroups, which could affect the reliability of the statistical analyses. Third, the diagnosis of hip dysplasia was based on the CE angle, but recent studies have emphasized that dysplasia should not be based on this parameter alone (17). 3-dimensional CT showed that although lateral acetabular deficiency was present in all the patients, several other radiographic features of dysplasia were also found (18). Fourth, the age at measurement of CE angles varied considerably. However, as a previous study showed that the CE angle in hips without subluxation did not change significantly after the age of 15–20 years (4), the CE angles in the oldest patients were probably representative for those at a younger adult age. Finally, because NAR started its registration of THAs in 1988 and reports a registration completeness of 97% (14) some THAs might have been lost to our registration. However, the patients had been examined clinically for a previous study (11), which ensured that no THAs had been performed before NAR was active. The strengths of the study are the long follow-up time and that data on acetabular dysplasia at skeletal maturity and whether or not THA had been performed were available in all patients.
In conclusion, what are the clinical implications of this study? First, it provides important knowledge to patients and caregivers regarding what long-term outcome can be expected after late-detected DDH when no pelvic osteotomies have been performed. Second, the results are relevant for the discussion of the indications and timing of treatment, which remains a controversial topic (19-22). The survival curves with THA as the endpoint are well suited for comparison with those of more modern treatment concepts including pelvic osteotomies, although the latter patients have preoperative hip pain, whereas pain had not been systematically recorded in the case reports of the present patients. PAO was initially recommended for patients with more pronounced degrees of hip dysplasia (9), but the procedure has in recent years also been used for symptomatic patients with mild dysplasia. In patients ≤ 21 years with CE angles 18–25°, Swarup et al. (21) reported good clinical and radiographic outcomes, but the follow-up time was short (minimum 1 year). Future studies with longer follow-up would be suitable for comparison with the present results.
- Salter R B. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br 1961; 43: 518-39.
- Ganz R, Klaue K, Vinh T S, Mast J W. A new periacetabular osteotomy for the treatment of hip dysplasia: technique and preliminary results. Clin Orthop Relat Res 1988; 232: 26-36.
- Holm A G V, Reikerås O, Terjesen T. Long-term results of a modified Spitzy shelf operation for residual hip dysplasia and subluxation: a fifty year follow-up study of fifty-six children and young adults. Int Orthop 2017; 41: 415-21.
- Terjesen T. Residual hip dysplasia as a risk factor for osteoarthritis in 45 years follow-up of late-detected hip dislocation. J Child Orthop 2011; 5: 425-31. 2011.
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand (Suppl. 58) 1939; 83: 7-135.
- Albinana J, Dolan L A, Spratt K F, Morcuende J, Meyer M D, Weinstein S L. Acetabular dysplasia after treatment for developmental dysplasia of the hip: implications for secondary procedures. J Bone Joint Surg Br 2004; 86-B: 876-86.
- Malvitz T A, Weinstein S L. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am 1994; 76: 1777-92.
- Thomas S R, Wedge J H, Salter R B. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am 2007; 89: 2341-50.
- Lerck D, Steppacher S D, Liechti F, Tannast M, Siebenrock K A. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Rel Res 2017; 475: 1154-68.
- Wells J, Millis M, Kim Y-J, Bulat E, Miller P, Matheney T. Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res 2017; 475: 396-405.
- Terjesen T, Horn J, Gunderson R B. Fifty-year follow-up of latedetected hip dislocation. Clinical and radiographic outcomes for seventyone patients treated with traction to obtain gradual closed reduction. J Bone Joint Surg Am 2014; 96: e28(1-9).
- Reimers J. The stability of the hip in children. Acta Orthop Scand 1980 (Suppl. 184); 51: 4-91.
- Kalamchi A, MacEwen G D. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am 1980; 62: 876-88.
- Espehaug B, Furnes O, Havelin L I, Engesæter L B, Vollset S E, Kindseth O. Registration completeness in the Norwegian Arthroplasty Register. Acta Orthop 2006; 77: 49-56.
- Cooperman D R, Wallensteen R, Stulberg S D. Acetabular dysplasia in the adult. Clin Orthop Relat Res 1983; (175): 79-85.
- Ziran N, Varcadipane J, Kadri O, Ussef N, Kanim L, Foster A, et al. Ten- and 20-year survivorship of the hip after periacetabular osteotomy for acetabular dysplasia. J Am Acad Orthop Surg 2019; 27: 247-55.
- McClincy M P, Wylie J D, Yen Y-M, Novais E N. Mild or borderline hip dysplasia: are we characterizing hips with a lateral center–edge angle between 18° and 25° appropriately? Am J Sports Med 2019; 47: 112-22.
- Nepple J J, Wells J, Ross J R, Bedi A B, Schoenecker P L, Clohisy J C. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res 2017; 475: 1037-44.
- Wenger D. Is there a role for acetabular dysplasia correction in an asymptomatic patient? J Pediatr Orthop 2013; 33: S8-S12.
- Willemsen K, Doelman C J, Sam A S Y, Seevinck P R, Sakkers R J B, Weinans H, et al. Long-term outcomes of the hip shelf arthroplasty in adolescents and adults with residual hip dysplasia: a systematic review. Acta Orthop 2020; 91: 383-9.
- Swarup I, Zaltz I, Robustelli S, Sink E. Outcomes of periacetabular osteotomy for borderline hip dysplasia in adolescent patients. J Hip Preserv Surg 2020; 7: 249-55.
- Baghdadi S, Sankar W. Residual acetabular dysplasia in the reduced hip. Indian J Orthop 2021; 55: 1480-9.