Study protocol for discharge on day of surgery after hip and knee arthroplasty from the Center for Fast-track Hip and Knee Replacement
Martin LINDBERG-LARSEN 1,2, Claus VARNUM 1,3, Thomas JAKOBSEN 1,4, Mikkel Rathsach ANDERSEN 1,5, Kim SPERLING 1,6, Søren OVERGAARD 1,7, Torben Bæk HANSEN 1,8, Christoffer Calov JØRGENSEN 1,9, Henrik KEHLET 1,10, and Kirill GROMOV 1,11
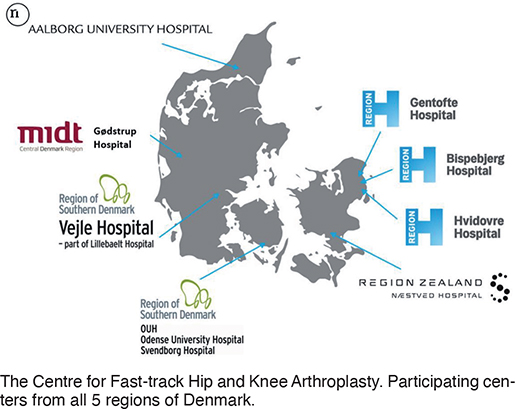
1 Center for Fast-track Hip and Knee Replacement; 2 Department of Orthopaedic Surgery and traumatology, Odense University Hospital and Svendborg; 3 Department of Orthopaedic Surgery, Lillebaelt Hospital—Vejle; 4 Department of Orthopaedic Surgery, Aalborg University Hospital; 5 Department of Orthopaedic Surgery, Copenhagen University Hospital, Herlev-Gentofte; 6 Department of Orthopaedic Surgery, Næstved, Slagelse and Ringsted Hospitals; 7 Department of Orthopaedic Surgery and Traumatology, Copenhagen University Hospital, Bispebjerg; 8 University Clinic for Hand, Hip and Knee Surgery, Hospital Unit West Jutland and Aarhus University; 9 Department of Anaesthesia, Hospital of Northern Zeeland, Hillerød; 10 Section of Surgical Pathophysiology, Copenhagen University Hospital, Rigshospitalet; 11 Department of Orthopaedic Surgery, Hvidovre University Hospital, Denmark
Background and purpose — Limited data exists on the implementation process and safety of discharge on the day of surgery after primary hip and knee arthroplasty in a multicenter setting. We report our study protocol on the investigation of the feasibility, safety, and socioeconomic aspects following discharge on day of surgery after hip and knee arthroplasty across 8 fast-track centers.
Patients and methods — This is a study protocol for a prospective cohort study on discharge on day of surgery from the Center for Fast-track Hip and Knee Replacement. The collaboration includes 8 centers covering 40% of the primary hip and knee arthroplasty procedures undertaken in Denmark. All patients scheduled for surgery are screened for eligibility using well-defined inclusion and exclusion criteria. Eligible patients fulfilling discharge criteria will be discharged on day of surgery. We expect to screen 9,000 patients annually.
Duration and outcome — Patients will be enrolled over a 3-year period from September 2022 and reporting of results will run continuously until December 2025. We shall report the proportion of eligible patients and patients discharged on day of surgery as well as limiting factors. Readmissions and complications within 30 days are recorded with real-time follow-up by research staff. Furthermore, patient-reported information on willingness to repeat discharge on day of surgery, contacts with the healthcare system, complications, and workability is registered 30 days postoperatively. EQ-5D, Oxford Knee Score, and Oxford Hip Score are completed preoperatively and after 3 months and 1 year. Finally, outcome data will be used in the development of a prediction model for successful discharge on the day of surgery.
Citation: Acta Orthopaedica 2023; 94: 121–127. DOI: https://doi.org/10.2340/17453674.2023.11636.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-25. Accepted: 2023-03-04. Published: 2023-03-20.
Correspondence: martin.lindberg-larsen@rsyd.dk
All authors are members of the Center for Fast-track Hip and Knee Replacement steering committee. The study protocol and guideline were planned at steering committee meetings. MLL, CV, and KG wrote the primary draft of the manuscript and led the discharge on day of surgery project within the collaboration. All authors reviewed the manuscript. MLL, KG, CV, SO, KS, MRA, TBH, and TJ are representatives from each of the 8 participating centers.
Handling co-editors: Bart Swierstra and Philippe Wagner
Acta thanks Justine Naylor and Annette W-Dahl for help with peer review of this study.
Fast-track hip and knee arthroplasty is becoming the standard of care worldwide for selected patients. Studies have shown a reduction in perioperative morbidity and mortality (1), with a concomitant reduction in length of stay (2) and a reduction in costs (3) as functional discharge criteria are achieved earlier. Discharge on day of surgery can be seen as the ultimate goal of fast-track arthroplasty and has gained interest in an increasingly competitive financial environment (4,5). The COVID-19 pandemic has further fueled interest in discharge on day of surgery, as the number of beds available for elective surgery has been reduced, but the demands for hip and knee surgery were unchanged. This motivated shorter stay in hospital. Additionally, the need for optimal utilization of healthcare resources is evident (6,7).
Despite multiple studies showing that discharge on day of surgery after total hip arthroplasty (THA), total knee arthroplasty (TKA), and unicompartmental knee arthroplasty (UKA) may be both feasible and safe in selected patients (8-12), utilization of discharge on day of surgery remains low. Only 0.5% in the United Kingdom (13) and about 5% in Denmark (14) are discharged on the day of surgery after THA and TKA. Discharge on day of surgery after UKA is higher, at 5% in the United Kingdom (13) and 19% in Denmark (15).
There is a need for more detailed multicenter studies regarding selection criteria and patient safety (16). Thus, it is important to investigate whether discharge on day of surgery is possible without compromising patient satisfaction, functional outcome, and risk of complications. Likewise, it is important to investigate whether discharge on day of surgery is possible on a larger scale without increasing costs for the patient or the healthcare system. Previous studies have been performed in dedicated centers, but protocols that standardize or prescribe criteria for patients for whom day of surgery discharge may be relevant and may help broader and safe adoption of this practice.
Aim
The proposed research project will determine the feasibility, safety, and socioeconomic aspects following discharge on day of surgery after primary hip and knee arthroplasty across 8 well-established fast-track centers in a socialized healthcare system in Denmark. The ambition is to increase the discharge on day of surgery after uniform multicenter introduction without compromising patient safety, satisfaction, and costs. In this perspective, we also present our current guideline for discharge on day of surgery.
Study protocol
Study design and organization
This is a study protocol for a prospective cohort study on discharge on day of surgery from the Center for Fast-track Hip and Knee Replacement, a multicenter collaboration consisting of 8 arthroplasty centers (17), covering approximately 40% of the annual hip and knee arthroplasty production in Denmark (Figure) (2). All centers follow the same guideline for discharge on day of surgery as described in this protocol. Prior to this project, only 3 (Odense University Hospital Svendborg, Lillebaelt Hospital—Vejle, Hvidovre University Hospital) of the 8 centers offered discharge on day of surgery, with up to 15% of all primary THA and TKA patients being discharged on day of surgery (10).
Center and staff education
An educational program was introduced for the 5 centers that had not implemented outpatient hip and knee arthroplasty surgery prior to study initiation. The program was cross-sectional and included education of all involved healthcare professionals at the centers and a written professional instruction. Instructions and teaching resources were available from the 3 centers with an already established outpatient program and education also included multidisciplinary visits to these centers.
Study period and number of participants
Outpatient surgery according to this protocol is implemented at the 8 participating centers from September 1, 2022. Inclusion of patients and reporting of results will run continuously until the end of 2025. We expect to screen approximately 9,000 patients and schedule about 3,000 patients for discharge on day of surgery annually.
Study participants and eligibility criteria
Patients scheduled for hip and knee arthroplasty at the 8 participating centers will be included in a database after informed consent. Inclusion and exclusion criteria for planned discharge on day of surgery are presented in Table 1. The chosen criteria were based on previous data from outpatient surgery (10,18) as well as our previous multicenter data on risk of complications after fast-track hip and knee arthroplasty (2).
Outpatient visit and preoperative phase
All patients scheduled for primary unilateral THA, TKA, or UKA at participating centers are screened for potential discharge on day of surgery according to the inclusion and exclusion criteria (Table 1). Patients fulfilling inclusion criteria will be informed about potential discharge on day of surgery. Preoperative blood samples including hemoglobin, C-reactive protein, creatinine, and electrolytes are taken, as well as blood glucose and HbA1c in diabetic patients.
Operation scheduling
If possible, patients eligible for discharge on day of surgery are scheduled for surgery as the first patients on the operation program with intended start of surgery before 1 p.m.
Surgery and anesthesia
All patients receive high-dose glucocorticoids preoperatively (24 mg dexamethasone or 125 mg methylprednisolone) except insulin-dependent diabetic patients (19-22). 1 gram of tranexamic acid is administered intravenously during surgery in all patients and may be repeated 3–4 hours postoperatively (23,24). Patients are operated on according to a standard protocol of the individual center. Local anesthesia with minimum 150 mL ropivacaine 2 mg/mL is used in knee arthroplasties but not in hip arthroplasties (25). Both general anesthesia and spinal anesthesia may be used (26). For spinal anesthesia a relatively short-acting blockade with, e.g., ropivacaine 5 mg/mL, 3–4 mL or Marcaine 5 mg/mL 2–2.5 mL is recommended to facilitate early mobilization within 2 hours postoperatively. Peripheral nerve blocks are not used routinely (27).
Postoperative pain management and other medication
Multimodal opioid-sparing postoperative analgesics including paracetamol (1 g x 4), nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (400 mg x 3/4), or COX-2 inhibitors such as celecoxib (200 mg x 2) will be used except in cases where contraindicated. Opioids of any kind are used only as rescue treatment and opioids with depository effect are not used routinely. Medication with paracetamol and NSAIDs is initiated 1–2 hours preoperatively as premedication (28,29). Furthermore, antiemetics and laxative treatment are provided postoperatively for rescue use.
Antibiotic prophylaxis
Antibiotic prophylaxis is administered 30–60 minutes preoperatively at all sites with either cloxacillin 2 g IV or cefuroxime 1.5 g IV according to local microbiological guidelines. For knee surgery, 1 additional dose (1 g cloxacillin or 1.5 g cefuroxime) is administered within 6 hours postoperatively before discharge. For hips, a protocol for a national randomized controlled trial (ProHipQ-OA, NCT05530551) is followed comparing only preoperative prophylaxis with preoperative prophylaxis plus repeated doses 6, 12, and 18 hours postoperatively (first postoperative dose IV and the remaining doses as tablets).
Postoperative thromboprophylaxis
Postoperative thromboprophylaxis is administered once 6 to 10 hours after surgery using rivaroxaban (Xarelto 10 mg, Bayer Pharma, Berlin, Germany) or apixaban (Eliquis 5 mg, Bristol-Myers Squibb, Princeton, NJ, USA) (30).
Postoperative mobilization and discharge
All patients are intended to be mobilized < 3 hours following end of surgery with full weightbearing.
Patients fulfilling discharge criteria will be discharged to their own home. Discharge criteria are presented in detail in Table 2. All patients receive instruction in rehabilitation exercises before discharge.
| Discharge criteria |
Activity level
|
Postoperative nausea and vomiting (PONV)
|
Pain
|
Postoperative bleeding
|
| a EWS = national implemented Early Warning Score systems based on NEWS2 from the Royal College of Physicians (36). |
Knee arthroplasty patients receive supervised rehabilitation 1–2 times a week for 2–3 months postoperatively in their local municipality, except for 1 center where it is only offered to selected knee patients. Hip arthroplasty patients do not routinely receive supervised rehabilitation postoperatively after discharge. The use of postoperative consultations in the outpatient clinic varies among centers.
Database
All data is collected in a REDCap database in collaboration with the Open Patient data Explorative Network (OPEN) in Odense University Hospital. Data includes patient-reported data from questionnaires filled in online or on paper according to preference. Furthermore, additional detailed data from patient files on patient comorbidities, medications, and blood samples is registered by dedicated research staff (nurses and physiotherapists) with physician back-up if necessary.
Preoperative data
Detailed patient-reported data on patient characteristics including Clinical Frailty Score, medical comorbidities, social status, workability, and living conditions is registered by the patients preoperatively with help from research staff if necessary. Furthermore, patient-reported outcomes (joint specific and generic) as well as a Pain Catastrophizing Scale are achieved through questionnaires filled in by the patients preoperatively. Preoperative medication is registered from medical charts and categorized according to indications by research staff. Data on preoperative blood samples including hemoglobin, creatinine, glomerular filtration rate, and C-reactive protein is registered by research staff. Preoperative blood samples are taken, and data is registered in the database as close to surgery as possible and maximum 2 months before.
Outcomes
Postoperative outcomes will also be registered in the database using a combination of chart review, by research staff, using the electronic healthcare records and a patient-reported questionnaire sent out 30 days postoperatively. Specific reasons for not being discharged on day of surgery are registered in patients not discharged on day of surgery despite being scheduled for it. Registration of severity of postoperative complications leading to a primary admission > 2 days or readmissions to hospital within 30 days after surgery is done using the Clavien–Dindo and Comprehensive Complication Index (31). Outcomes are listed in Table 3.
Dissemination plan
The reporting of results is planned to be divided into 4 parts:
1. Implementation of discharge on day of surgery after hip and knee arthroplasty
Main aim: to investigate the implementation process and feasibility of outpatient THA, TKA, and UKA in centers with well-established fast-track pathways in a public healthcare system.
Primary outcome: percentage of patients discharged on the day of surgery 6 months after implementation (March 1, 2023) in total and in each center, compared with baseline.
Secondary outcome: to describe barriers in the implementation process in total and on center level.
2. Safety of discharge on day of surgery after hip and knee arthroplasty in a multicenter setting
Main aim: to investigate complications and readmissions within 30 days in patients eligible for outpatient surgery discharged on day of surgery, compared with eligible patients not discharged on day of surgery in the same period, as well as baseline controls.
Primary outcome: readmission risk within 30 days after surgery.
Secondary outcomes: all postoperative complications (scored using Clavien–Dindo and Comprehensive Complication Index) and all other contacts with healthcare system including general practitioner and outpatient visits within 30 days.
3. Prediction of successful discharge on day of surgery
Main aim: development of a prediction tool for discharge on the day of surgery.
Outcomes: risk factors for unsuccessful discharge on day of surgery despite fulfilling inclusion criteria.
4. Socioeconomic analysis of discharge on day of surgery
Aim: to investigate impact on the costs per patient of implementation of discharge on day of surgery after hip and knee arthroplasty on a national level.
Estimation of costs per patient will include the costs related to the following outcomes:
- all contacts with the healthcare system within 30 days postoperatively;
- use of home nurses from the municipalities and other community health services;
- duration of sick leave related to the surgical procedure;
- patient-reported outcome (function and health status);
- patient-reported willingness to repeat discharge on day of surgery;
- changes in workflow and potential reduction in use of hospital beds.
Statistical analysis plan
In this large-scale prospective cohort study, we address multiple outcomes. For most outcomes an observational before–after research design will be used to assess the impact of discharge on day of surgery. Baseline data from the Danish National Patient Registry (32) at the participating centers from 2019 and 2020 (pre-COVID status), will be used as a baseline control in most sub-studies. Furthermore, eligible patients not discharged on day of surgery and patients not eligible for discharge on day of surgery will be used as control groups where appropriate according to outcome. Most outcomes will be presented as proportions with 95% confidence intervals. In the analysis of risk factors for unsuccessful discharge on day of surgery, a multivariable logistic regression model will be used. Furthermore, we will use machine learning on preoperative data to develop a tool for future selection of patients best suited for discharge on day of surgery (33).
To ensure the feasibility of the study within the planned study period, preliminary power calculations for the main aims of the overall study have been performed. For discharge on day surgery, a conservative estimate is a 10-percentage point increase (from 5% to 15%). To detect this, a sample size of 266 patients in each group is needed using 90% power and 5% alpha. For risk of readmission ≤ 30 days after discharge on day of surgery, 1,411 patients are needed in the study group as well as the control group to be able to detect a potential difference of 3 percentage points (from 5% to 8%) using 90% power and 5% alpha. With the expected inclusion rate, the study is very feasible and reporting on all outcomes is possible within the study period.
Patient involvement
Patients and relatives are involved in the whole research process. The posed research questions have been prepared in collaboration with the patients and relatives council at the Orthopaedic Research Unit, Odense University Hospital. The patient-reported parts (questionnaires) of the fast-track database have been tested by patients and relatives and modified. Reporting of results and status of the research project will be continuously reported on our website and accessible to participants in the study and patients in general. Finally, we have planned annual workshops with patients and relatives from different centers in order to receive their input.
Ethics, registration, funding, and disclosures
Consecutive patients are included in the database after informed consent. Ethical approval was not necessary because treatment of eligible patients using discharge on day of surgery is standard of care at the participating centers according to the described guideline. This trial is registered in Region of Southern Denmark and data processing is approved (Journal No 22/39454). The study is also registered on ClinicalTrials. gov (NCT05613439).
In 2021, the collaboration received funding from the NOVO Nordisk foundation (Grant number: NNF21SA0073760) to support the organizational setup for the entire fast-track project including dedicated research staff at all centers, data monitoring and follow-up on complications. The “discharge on day of surgery project” is part of the entire fast-track project.
The authors are members of the steering committee of the Centre of Fast-track Hip and Knee Arthroplasty and report no conflicts of interest regarding this project. HK and KG are members of the Zimmer Biomet advisory board on rapid recovery. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.11636
Discussion
Clinical impact
Some 22,000 patients are treated with a primary hip or knee arthroplasty annually in Denmark. Mean length of hospital stay after these procedures is 1–2 days, but less than 5% are discharged on the day of surgery (14). It may be possible to increase the proportion of patients discharged on day of surgery to about 30% with continued high patient satisfaction and high patient safety. However, this requires an evidence based high-quality protocol, a well-established multicenter collaboration, and publication of the entire research process.
The planned studies on this project are clinically relevant and necessary as previous studies on the feasibility of outpatient hip and knee arthroplasty are based on data and experiences from a few dedicated centers (9-12,34). Previous largescale register-based studies show that the use of outpatient surgery may be safe, but the use of the concept varies between centers and safety was analyzed based on procedure and diagnosis codes and not on prospectively collected data (13,15). Hence, prospective multicenter consecutive cohort studies from a public socialized healthcare system including detailed standardized information on preoperative patient characteristics and postoperative complications, costs, and patient satisfaction are needed in order to evaluate generalizability and safety of discharge on day of surgery.
Strengths and limitations
This is a pragmatic study reflecting clinical practice as it is countrywide in both university and regional hospitals, thus increasing the generalizability of the findings. There is a short distance from research to actual clinical implementation, as shown before in the center collaboration. Hence, the study should be very feasible. Finally, the standardization of postoperative complications requiring hospitalization by using the Clavien–Dindo and Comprehensive Complication Index will provide an easily comparable measure reflecting both clinician and patient perspectives on severity.
A limitation of a multicenter study may be slight differences in logistics between centers. Furthermore, adherence to study protocol and guideline may vary among centers as many individuals are involved in patient treatment at 8 centers.
Future perspective
This study will show to what extent discharge on day of surgery after hip and knee arthroplasty can be implemented across multiple centers in a socialized healthcare setting. The safety and patient-related aspects of such an implementation will be investigated and disseminated. This study will allow for improvement of patient selection for discharge on day of surgery, as patients not fulfilling the criteria for discharge on day of surgery will be identified and analyzed. The findings from the study will lead to an updated guideline for discharge on day of surgery. Importantly, if it is possible to increase the frequency of patient discharge on day of surgery without compromising patient outcome using a well-defined guideline, this could be replicated and adapted worldwide and potentially in other parts of the healthcare system. In this way, the increasingly limited hospital resources can be used for the patients needing them most.
- Kehlet H. Fast-track hip and knee arthroplasty. Lancet 2013; 381(9878): 1600-2. doi: 10.1016/S0140-6736(13)61003-X.
- Petersen P B, Kehlet H, Jorgensen C C, Lundbeck Foundation Centre for Fast-track H, Knee Replacement Collaborative G. Improvement in fast-track hip and knee arthroplasty: a prospective multicentre study of 36,935 procedures from 2010 to 2017. Sci Rep 2020; 10(1): 21233. doi: 10.1038/s41598-020-77127-6.
- Andreasen S E, Holm H B, Jorgensen M, Gromov K, Kjaersgaard-Andersen P, Husted H. Time-driven activity-based cost of fast-track total hip and knee arthroplasty. J Arthroplasty 2017; 32(6): 1747-55. doi: 10.1016/j.arth.2016.12.040.
- Argenson J N, Husted H, Lombardi A Jr, Booth R E, Thienpont E. Global Forum: An international perspective on outpatient surgical procedures for adult hip and knee reconstruction. J Bone Joint Surg Am 2016; 98(13): e55. doi: 10.2106/JBJS.15.00998.
- Vehmeijer S B W, Husted H, Kehlet H. Outpatient total hip and knee arthroplasty. Acta Orthop 2018; 89(2): 141-4. doi: 10.1080/17453674.2017.1410958.
- Meneghini R M. Introduction: Optimizing hip and knee arthroplasty in the COVID era. J Arthroplasty 2021; 36(7S): S45. doi: 10.1016/j.arth.2021.03.011.
- Wainwright T W. Enhanced recovery after surgery (ERAS) for hip and knee replacement: why and how it should be implemented following the COVID-19 pandemic. Medicina (Kaunas) 2021; 57(1). doi: 10.3390/medicina57010081.
- Bemelmans Y F L, Keulen M H F, Heymans M, van Haaren E H, Boonen B, Schotanus M G M. Safety and efficacy of outpatient hip and knee arthroplasty: a systematic review with meta-analysis. Arch Orthop Trauma Surg 2022; 142(8): 1775-91. doi: 10.1007/s00402-021-03811-5.
- Dey S, Gadde R, Sobti A, Macdonald N, Jacob J, Unnithan A. The safety and efficacy of day-case total joint arthroplasty. Ann R Coll Surg Engl 2021; 103(9): 638-44. doi: 10.1308/rcsann.2021.0066.
- Gromov K, Kjaersgaard-Andersen P, Revald P, Kehlet H, Husted H. Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop 2017; 88(5): 516-21. doi: 10.1080/17453674.2017.1314158.
- Rozell J C, Ast M P, Jiranek W A, Kim R H, Della Valle C J. Outpatient total joint arthroplasty: the new reality. J Arthroplasty 2021; 36(7S): S33-9. doi: 10.1016/j.arth.2021.02.030.
- Schmidt A M, Garval M, Gromov K, Holm C, Larsen J R, Runge C, et al. Feasibility, safety, and patient-reported outcomes 90 days after same-day total knee arthroplasty: a matched cohort study. Acta Orthop 2022; 93: 509-18. doi: 10.2340/17453674.2022.2807.
- Wainwright T W. The current status of daycase hip and knee arthroplasty within the English National Health Service: a retrospective analysis of hospital episode statistics data. Ann R Coll Surg Engl 2021; 103(5): 324-31. doi: 10.1308/rcsann.2020.7142.
- Bredgaard Jensen C, Troelsen A, Bang Foss N, Skovgaard Nielsen C, Lindberg-Larsen M, Gromov K. The 10-year evolution of day-case hip and knee arthroplasty: a nationwide registry study of 166,833 procedures from 2010–2020. Acta Orthop. Accepted March 2023.
- Arndt K B, Varnum C, Lindberg-Larsen M, Jensen C B, Rasmussen L E. Readmissions and mortality after outpatient vs inpatient unicompartmental knee arthroplasty in Denmark: a propensity score matched study of 5,384 procedures. Knee 2022; 38: 50-5. doi: 10.1016/j.knee.2022.07.008.
- Wainwright T W, Memtsoudis S G, Kehlet H. Fast-track hip and knee arthroplasty … how fast? Br J Anaesth 2021; 126(2): 348-9. doi: 10.1016/j.bja.2020.09.038.
- Artz N, Elvers K T, Lowe C M, Sackley C, Jepson P, Beswick A D. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord 2015; 16: 15. doi: 10.1186/s12891-015-0469-6.
- Berend K R, Lombardi A V Jr, Berend M E, Adams J B, Morris M J. The outpatient total hip arthroplasty: a paradigm change. Bone Joint J 2018; 100-B(1 Supple A): 31-5. doi: 10.1302/0301-620X.100B1.BJJ-2017-0514.R1.
- Gasbjerg K S, Hagi-Pedersen D, Lunn T H, Laursen C C, Holmqvist M, Vinstrup L O, et al. Effect of dexamethasone as an analgesic adjuvant to multimodal pain treatment after total knee arthroplasty: randomised clinical trial. BMJ 2022; 376: e067325. doi: 10.1136/bmj-2021-067325.
- Nielsen N I, Kehlet H, Gromov K, Troelsen A, Husted H, Varnum C, et al. High-dose steroids in high pain responders undergoing total knee arthroplasty: a randomised double-blind trial. Br J Anaesth 2022; 128(1): 150-8. doi: 10.1016/j.bja.2021.10.001.
- Jorgensen C C, Pitter F T, Kehlet H, Lundbeck Foundation Center for Fast-track H, Knee Replacement Collaborative G. Safety aspects of preoperative high-dose glucocorticoid in primary total knee replacement. Br J Anaesth 2017; 119(2): 267-75. doi: 10.1093/bja/aex190.
- Lex J R, Edwards T C, Packer T W, Jones G G, Ravi B. Perioperative systemic dexamethasone reduces length of stay in total joint arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty 2021; 36(3): 1168-86. doi: 10.1016/j.arth.2020.10.010.
- Sun Q, Li J, Chen J, Zheng C, Liu C, Jia Y. Comparison of intravenous, topical or combined routes of tranexamic acid administration in patients undergoing total knee and hip arthroplasty: a meta-analysis of randomised controlled trials. BMJ Open 2019; 9(1): e024350. doi: 10.1136/bmjopen-2018-024350.
- Magill P, Hill J C, Bryce L, Martin U, Dorman A, Hogg R, et al. Oral tranexamic acid for an additional 24 hours postoperatively versus a single preoperative intravenous dose for reducing blood loss in total knee arthroplasty: results of a randomized controlled trial (TRAC-24). Bone Joint J 2021; 103-B(10): 1595-603. doi: 10.1302/0301-620X.103B10.BJJ-2020-2308.R1.
- Andersen L O, Kehlet H. Analgesic efficacy of local infiltration analgesia in hip and knee arthroplasty: a systematic review. Br J Anaesth 2014; 113(3): 360-74. doi: 10.1093/bja/aeu155.
- Pu X, Sun J M. General anesthesia vs spinal anesthesia for patients undergoing total-hip arthroplasty: a meta-analysis. Medicine (Baltimore) 2019; 98(16): e14925. doi: 10.1097/MD.0000000000014925.
- Memtsoudis S G, Cozowicz C, Bekeris J, Bekere D, Liu J, Soffin E M, et al. Peripheral nerve block anesthesia/analgesia for patients undergoing primary hip and knee arthroplasty: recommendations from the International Consensus on Anesthesia-Related Outcomes after Surgery (ICAROS) group based on a systematic review and meta-analysis of current literature. Reg Anesth Pain Med 2021; 46(11): 971-85. doi: 10.1136/rapm-2021-102750.
- Anger M, Valovska T, Beloeil H, Lirk P, Joshi G P, Van de Velde M, et al. PROSPECT guideline for total hip arthroplasty: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia 2021; 76(8): 1082-97. doi: 10.1111/anae.15498.
- Lavand’homme P M, Kehlet H, Rawal N, Joshi G P, PROSPECT Working Group of the European Society of Regional Anaesthesia and Pain Therapy (ESRA). Pain management after total knee arthroplasty: PROcedure SPEcific Postoperative Pain ManagemenT recommendations. Eur J Anaesthesiol 2022; 39(9): 743-57. doi: 10.1097/EJA.0000000000001691.
- Petersen P B, Kehlet H, Jorgensen C C, Lundbeck Foundation Centre for Fast-track H, Knee Replacement Collaborative G. Safety of in-hospital only thromboprophylaxis after fast-track total hip and knee arthroplasty: a prospective follow-up study in 17,582 procedures. Thromb Haemost 2018; 118(12): 2152-61. doi: 10.1055/s-0038-1675641.
- Slankamenac K, Graf R, Barkun J, Puhan M A, Clavien P A. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 2013; 258(1): 1-7. doi: 10.1097/SLA.0b013e318296c732.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90. doi: 10.2147/CLEP.S91125.
- Gogenur I. Introducing machine learning-based prediction models in the perioperative setting. Br J Surg 2023; Jan 21: znac462. doi: 10.1093/bjs/znac462. Epub ahead of print.
- Bemelmans Y F L, Keulen M H F, Heymans M, van Haaren E H, Boonen B, Schotanus M G M. Safety and efficacy of outpatient hip and knee arthroplasty: a systematic review with meta-analysis. Arch Orthop Trauma Surg 2022; 142(8): 1775-91. doi: 10.1007/s00402-021-03811-5.
- Nissen S K, Fournaise A, Lauridsen J T, Ryg J, Nickel C H, Gudex C, et al. Cross-sectoral inter-rater reliability of the clinical frailty scale: a Danish translation and validation study. BMC Geriatr 2020; 20(1): 443. doi: 10.1186/s12877-020-01850-y.
- Physicians RCo. National Early Warning Score (NEWS) 2: standardising the assessment of acute-illness severity in the NHS. Updated report of working party 2017 [Available from: file:///C:/Users/iby8fi/AppData/Local/Temp/MicrosoftEdgeDownloads/20c21027-af83-489a-905b-0ff54dc6dff9/NEWS2%20final%20report_0_0.pdf.