Long-term effects of retrograde approach on the knee after motorized femoral limb lengthening
Andreas H KRIEG 1, Chao DONG 1, Marc P SCHMID 2, Bernhard M SPETH 1, Dorothee HARDER 3, and Ricardo DONNERS 3
1 Pediatric Orthopedic Department, University Children’s Hospital Basel (UKBB), Basel; 2 University of Basel, Basel; 3 Department of Radiology, University Hospital Basel (USB), Basel, Switzerland
Background and purpose — The retrograde femoral approach is an established technique for implantation of nails for leg lengthening and correction and in cases of distal femoral fractures. The purpose of this study was to determine the 10-year outcome of this technique by analyzing the clinical long-term effects and radiological status of the knee after leg lengthening via a retrograde femoral approach.
Patients and methods — This retrospective single-center study included 13 patients (median age at surgery 17 [range 15–20] years) who underwent unilateral, retrograde, femoral lengthening with a motorized nail. Outcome measurements were graded variables of the SF-36, ISKD score, and Lysholm score. MRI of both knees was performed in all patients. MRI was evaluated for the presence of degenerative changes and compared with the healthy contralateral knee. Cartilage condition was graded according to the International Cartilage Repair Society (ICRS) scoring system.
Results — All patients were pain-free and had a full range of motion 10 (range 10.0–12.2) years after surgery. All postoperative knees showed fibrosis of Hoffa’s fat pad and moderate to severe cartilage defects (ICRS Grade 2–4) of the trochlear groove (nail entry site). 6 out of 13 operated knees exhibited retropatellar cartilage defects.
Conclusion — Our study showed that patients were pain-free, but cartilage defects at the entry point and arthrofibrosis at Hoffa’s fat pad were observed without causing clinical impairment.
Citation: Acta Orthopaedica 2023; 94: 128–134. DOI https://doi.org/10.2340/17453674.2023.10323.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-10-03. Accepted: 2023-01-28. Published: 2023-03-22.
Correspondence: andreas.krieg@ukbb.ch
AHK performed all surgeries and designed the work. DH and RD organized all MRIs and analyzed them. CD and MPS collected the data, CD and BMS performed data analysis. AHK and RD wrote the manuscript. BMS, DH, and CD critically reviewed the manuscript. BMS, AHK, and RD finalized the manuscript.
Handling co-editor: Ivan Hvid
Acta thanks Franck Accadbled and Jan Rölfing for help with peer review of this study.
The correction of congenital and post-traumatic femoral deformities is a common indication in orthopedic surgery. Femoral bone lengthening with external fixators has proved to be associated with a high-risk profile (1,2). In contrast, the use of the recently introduced motorized femoral intramedullary nail has allowed a significant reduction in intervention-related complications while maintaining the advantages of a retrograde approach (3-6). A major advantage of the retrograde over an anterograde technique is the greater potential for correction of limb deformities (3). In addition, the retrograde femoral approach has been described as beneficial for the treatment of distal diaphyseal and metaphyseal fractures in obese patients (7,8). Although retrograde nailing is a promising technique, there are several steps and features specific to this method that must be followed to minimize complications. For example, the use of drill sleeves is essential to avoid contaminating the knee joint with bone marrow and to protect the patella and quadriceps tendon (5,6,9). Contemporary literature revealed superior patient outcomes after lower extremity valgus correction with a retrograde intramedullary femoral nail (IMFN) versus a less invasive stabilization system (LISS) procedure. IMFN patients displayed better limb function, patient comfort, and healing parameters 2 years after surgery. Radiological comparison showed no significant differences in the knee joint findings between the IMFN and LISS patients (10).
Overall, the current literature suggests good patient safety and outcomes within a 12–24-month follow-up period after retrograde femoral nailing (11,12). However, studies with longer follow-up are lacking. These are of interest, though, as the retrograde approach could be associated with accelerated knee joint degeneration, which may become evident only many years after surgery in this usually young patient cohort. Therefore, the question remains whether retrograde femoral nailing in the long term leads to accelerated degeneration of the knee joint and patient discomfort. Consequently, the purpose of this study was to assess radiologically and clinically the knee joints of patients 10 years after retrograde motorized femoral nailing surgery.
Patients and methods
Study design, setting, and participants
This is a retrospective single-center study reported according to STROBE guidelines. Between January 2006 and December 2009, 20 patients with leg-length discrepancy had undergone leg lengthening with a motorized nail (FITBONE, Telescope Active Actuator nail [TAA]; WITTENSTEIN intens GmbH, Igersheim, Germany) via the retrograde femoral approach at our institution. At the time of initial surgery, all patients had closed physes.
Patient inclusion criteria were intramedullary lengthening surgery performed at our institution, using a retrograde approach, during the given inclusion interval from 2006 to 2009. Cases in whom MRI examinations could not be performed safely were excluded from the study (e.g., pacemakers, cochlear implants, neurostimulators, other MRI-incompatible devices, claustrophobic patients requiring sedation, and pregnant patients) or when injury or surgery of the contralateral knee was reported (4 patients). 3 patients were lost to follow-up. Eventually, 13 patients (4 females, 9 males) were recruited (Figure 1). Median time between study enrollment and surgery was 10.0 (range 10.0–12.2) years and median patient age at the time of surgery 17 (range 15–20) years. Patient details are summarized in Table 1.
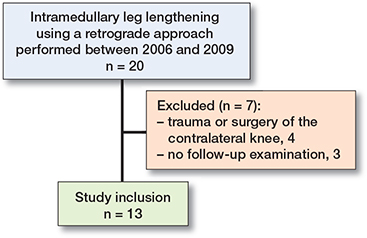
Figure 1. Flowchart of study inclusion.
Surgical procedure
Surgery was performed by a senior orthopedic surgeon with 20 years of experience (AK). Prior to surgery, leg length discrepancy, preoperative mechanical axis alignment, and joint alignment were assessed on plain radiographs (long-leg standing radiographs). These measurements were performed under conditions similar to the standard preoperative protocol for retrograde correction planning as described by Baumgart (13). The femoral FITBONE TAA is straight, unlike conventional trauma nails, which must be considered during preoperative planning. It is essential to plan for supracondylar femoral displacement and/or angulation osteotomies prior to surgery to achieve a corrected mechanical axis, thus avoiding early osteoarthritis after limb and joint malalignment.
The femoral nail was inserted through a small longitudinal incision of the patellar tendon, 1 centimeter below the patella via an opening in the trochlea with a diameter of 12.5 mm, which was prepared with continuous drilling from 8 mm to 12.5 mm. The bone was opened with special drill sleeves that prevented contamination of the knee joint with bone chips (Figure 2) and iatrogenic harm to the knee. The osteotomy was performed with a drill and chisel. The lengthening process was initiated 5 to 7 days after surgery by induction voltage. The impulses were applied 3 times a day.
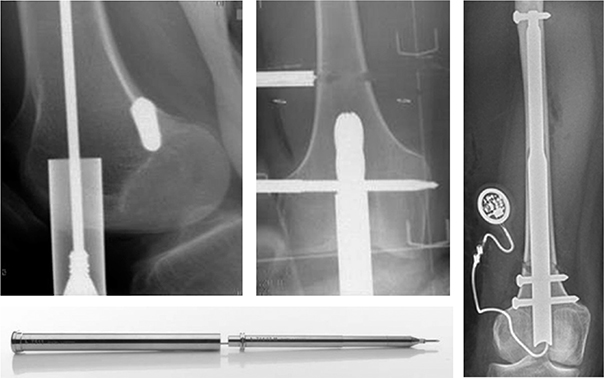
Figure 2. A 3-mm K-wire is used to define the optimal insertion point of the trochlea and a cone is inserted over the Kirschner wire to bluntly drain the patellar tendon and patella to the side. If the cone is correctly positioned, the protective sleeve (inner diameter 13 mm) is inserted retrograde with a tube sinker. Reaming (final reamer with 12.5 mm diameter) is performed from retrograde through the sleeve to the planned osteotomy line and a drill hole osteotomy is performed through a percutaneous incision. Right image shows the final result with the implanted nail.
Outcome assessment
The surgery side and the contralateral side were evaluated clinically and radiologically, with the latter serving as a control in this study.
Clinical assessment
The patient’s general health and both knees were clinically assessed, and health-related quality of life was measured with the Short Form (SF)-36 questionnaire—a generic 36-item questionnaire that measures 8 multi-item dimensions of health (14). The International Knee Documentation Committee (IKDC) score, which uses a subjective scale, was used to evaluate overall function. It contains 3 items: knee symptoms, sports activity, and knee function (15). Finally, the Lysholm Score, a 100-point scoring system that addresses knee function and limitation, was applied to evaluate the presence of limping, weight-bearing tolerance, locking, instability, pain, and swelling of the knee, as well as locomotion problems such as climbing stairs and squatting. The score is graded as excellent (95–100), good (84–94), fair (65–83), or poor (> 65) (16,17). The difference in scoring between the patient’s 2 knees was recorded.
Leg lengths were measured, pelvic equality was checked (posterior, superior, iliac, spines), gait was assessed (limping yes/no), and thigh circumferences were measured 15 cm above the upper patellar rim (CD, MS).
Radiological assessment
Plain radiographs obtained during the 10-year follow-up period were evaluated for consolidation. This was defined as corticalization of at least 3 sides of the callus on the biplane radiographs, followed by transition to full weight-bearing. Each individual lengthening period (distraction, maturation, consolidation) and the corresponding indices were calculated and evaluated. The last radiographic examination was performed after the removal of metal in all patients after successful distraction.
3.0T MRI (Siemens Prisma, Siemens Healthineers, Erlangen, Germany) of both knees was performed consecutively for each patient after study inclusion at the 10-year follow-up appointment. Images were evaluated by a board-certified radiologist with 5 years of experience in dedicated musculoskeletal radiology and a musculoskeletal imaging fellow.
Knee joint MRI images were morphologically assessed for marrow edematous changes, cartilage status, defects and tears of internal ligamentous structures and menisci, degenerative changes, capsule alterations, fibrosis, inflammatory changes such as synovitis, muscle atrophy, and fatty degeneration. The diameter of the distal quadriceps muscle 5 cm above the patella was compared with the contralateral knee. Cartilage condition was graded according to the International Cartilage Repair Society (ICRS) scoring system (18) in all compartments, with special attention paid to trochlear and retropatellar facets.
Statistics
Analyses were performed with commercially available software (SPSS Statistics Version 25, IBM Corp, Armonk, NY, USA) for calculation of mean and median, as well as 95% confidence intervals (CI) of the measurements.
Ethics, funding, and disclosures
This study has been approved by the local ethics committee (Ethikkomission Nordwest- und Zentralschweiz EKNZ 2018/01857). There are no conflicts of interest concerning the contents of this manuscript. AK was a paid consultant for ORTHOFIX S.R.L. The remaining authors declare no conflict of interest. This research was supported in part by the Kämpf Bötschi Foundation, Basel, Switzerland. The sponsors neither had an influence on study design, the collection, analysis, and interpretation of data, the preparation of the manuscript, nor on the decision to submit the article for publication. The views expressed in this manuscript are exclusively those of the authors. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.10323
Results
Distraction was started a median 6 (range 4–10) days postoperatively, with a median distraction index of 1.0 (range 0.8–1.7) mm/day. The median hospital stay was 14 (range 9–22) days. At the time, the retrograde femoral leg lengthening was a novel procedure in these young patients. Consequently, patients were kept under active surveillance in the hospital for a relatively long time to ensure patient recovery and comfort. The median femoral maturation index was 22 days/cm (range 16–30). The median consolidation index was 35 (range 27–44) days/cm for the femur.
Questionnaires and clinical evaluation
The median SF-36 score was 87. All patients could perform at least moderately strenuous activities without limitations, and 9 of 13 could perform very strenuous activities such as soccer, running, or lifting heavy objects without limitations. None of the patients had difficulties performing their work or other daily activities. 9 of 13 patients had not experienced pain during the past 4 weeks. The remaining patients reported mild discomfort.
A median IKDC score of 94% was obtained. 12 patients scored within the norm of their age group (age between 25 and 34 for male subjects: 89 (SD 16), for female subjects: 86 (SD 19) points) (19). The test showed no relevant clinical differences between the operated and nonoperated knees.
On the knee-specific Lysholm score, a median score of 93% was achieved. 12 patients achieved an excellent or good score (each n = 6). All patients were able to bear their full body-weight on one leg. 2 patients reported an occasional feeling of entrapment, but no locking sensation, and 1 patient reported occasional locking. 3 of 13 patients felt somewhat impaired when climbing stairs. Pelvic equality was achieved and maintained 10 years after surgery in 12 patients. 1 patient had a 1 cm deviation from pelvic equality, which was attributed to pre-existing pes equinus of 15°.
In all patients, the distraction goal was achieved and maintained after 10 years. The femur was lengthened by 3.4 cm (range 2.4–4.5 cm).
7 patients had a smaller thigh circumference on the operated side compared with the nonoperated side. Overall, the median circumference of the operated side was 2.6% or 1.3 (SD 0.5) cm smaller than the nonoperated side.
All patients showed a normal gait pattern without limping on the clinical examination. Painless anterior crepitation was evident in 8 out of 13 patients (Table 2).
| Patient ID | Leg circumference (cm) | Crepitation | Pelvic inequality | IKDC | Lysholm | SF36 | ||
| Operated side | nonoperated side | difference | ||||||
| 1 | 43 | 48.0 | –5.0 | + | – | 92 | 98 | 89 |
| 2 | 52.5 | 52.5 | 0 | – | – | 96 | 100 | 82 |
| 3 | 49 | 49.0 | 0 | + | – | 76 | 69 | 63 |
| 4 | 51.0 | 52.5 | –1.5 | + | – | 70 | 91 | 84 |
| 5 | 52.0 | 52.0 | 0 | – | – | 99 | 99 | 96 |
| 6 | 47.0 | 47.0 | 0 | – | – | 94 | 93 | 95 |
| 7 | 48.0 | 48.0 | 0 | + | – | 95 | 90 | 90 |
| 8 | 56.5 | 59.5 | –3.0 | + | + a | 82 | 88 | 79 |
| 9 | 44.0 | 45.0 | –1.0 | – | – | 81 | 91 | 79 |
| 10 | 49.0 | 50.0 | –1.0 | + | – | 100 | 100 | 87 |
| 11 | 45.0 | 49.0 | –4.0 | + | – | 84 | 88 | 89 |
| 12 | 49.5 | 51.5 | –2.0 | – | – | 95 | 98 | 87 |
| 13 | 50.5 | 50.0 | 0.5 | + | – | 98 | 95 | 89 |
| Median | 49.0 | 50.0 | –1.0 | 94 | 93 | 87 | ||
| CI | 48.0–49.5 | 48.0–51.5 | 0 to –2.0 | 84–95 | 91–95 | 84–89 | ||
| a (–1 cm) | ||||||||
Radiological evaluation
The results of the radiological assessment are summarized in Tables 3 and 4. Trochlear cartilage defects with an average ICRS score of 3.4 were found in all post-surgical knees, whereas no contralateral knee had an ICRS score larger than 1. ICRS grade was 4 in 8, grade 3 in 2, and grade 2 in 3 of 13 patients (Figure 3). In contrast, all contralateral nonoperated knees achieved ICRS grades 0 or 1. For the patellar cartilage, 3 of 13 knees showed ICRS grade 4, 2 grade 2, and 8 grades 0 or 1 on the operated side (Figure 4). 1 knee achieved grade 4 and the other 12 grades 0 or 1 on the nonoperated side.
| Patient ID | ICRS score a | Hoffa fibrosis b | Vastus atrophy | |
| trochlea | patella | |||
| 1 | 4 | 0 | 2 | + |
| 2 | 2 | 0 | 2 | – |
| 3 | 3 | 4 | 1 | + |
| 4 | 2 | 4 | 2 | + |
| 5 | 4 | 0 | 1 | + |
| 6 | 4 | 0 | 1 | + |
| 7 | 4 | 2 | 1 | + |
| 8 | 2 | 0 | 1 | + |
| 9 | 3 | 1 | 2 | + |
| 10 | 4 | 4 | 1 | – |
| 11 | 4 | 0 | 2 | + |
| 12 | 4 | 1 | 1 | + |
| 13 | 4 | 2 | 1 | – |
| a ICRS score: 0 = normal, 1 = nearly normal (superficial lesions), 2 = abnormal (lesions extending down < 50% of cartilage depth), 3 = severely abnormal (lesions extending down > 50% of cartilage depth as well as down to the calcified level or the subchondral bone but not through the subchondral bone), 4 = severely abnormal (like 3 but with extension to the subchondral bone).
b 0 = none, 1 = mild, 2 = extensive. |
||||
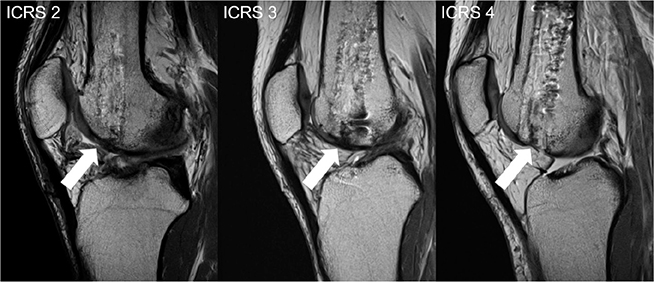
Figure 3. Cartilage damage of the trochlea—representative PD-weighted, sagittal images, showing the cartilage defects of the trochlea at the nail entry site (arrows), with the majority of patients (8/13) having high-grade defects with no residual cartilage coverage (ICRS 4); the minimum score was ICRS 2.
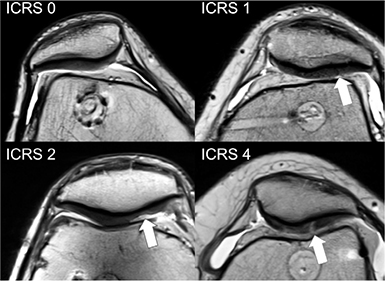
Figure 4. Retropatellar cartilage damage—representative PD-weighted axial images showing the scope of cartilage findings following a retrograde nail implantation (arrows), most commonly (6/13) no cartilage damage was found (ICRS 0).
Hoffa’s fibrosis was found in the MRI of all operated knees (Figure 5). Musculus vastus medialis femoris atrophy was noted in 10 out of 13 operated knees and in none of the contralateral controls (Figure 6).
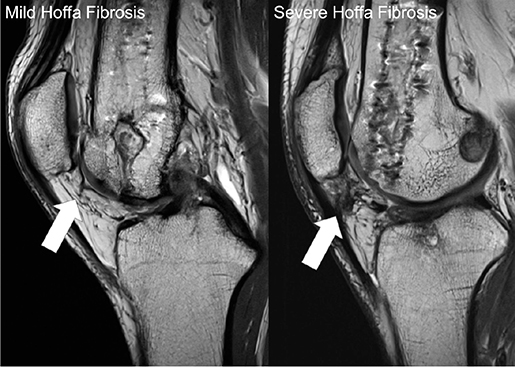
Figure 5. Hoffa fibrosis—representative, PD-weighted, sagittal images showing an example of mild fibrosis found in 8 patients and severe fibrosis found in 5 (arrows).
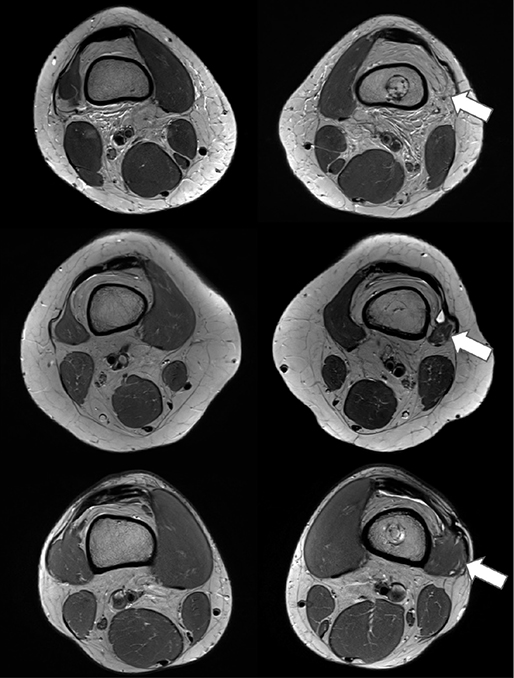
Figure 6. Quadriceps atrophy—representative PD-weighted axial images showing atrophy of the side of surgery (right column) compared with the nonoperated side (left column). More severe atrophy, especially of the M. vastus lateralis (arrows), is shown in the top row, less severe in the middle row, and no atrophy between sides in the bottom row.
There was no significant difference regarding the presence of joint effusion when comparing the operated with the contralateral knees. There was minimal joint effusion on both sides in 6 out of 13 knees, and 2 patients displayed this on the operated side only. The remaining 5 patients had no joint effusion at all.
Discussion
This study compared the operated with the nonoperated knee in patients with status post-femoral lengthening via the retrograde approach with an intramedullary nail over 10 years after surgery. The study showed that patients were pain-free with good limb function, but high-grade cartilage defects of the trochlea and Hoffa’s fat pad fibrosis were common MRI findings.
All patients had good clinical outcome 10 years following surgery with a retrograde approach. Accordingly, clinical examinations showed no relevant differences between joint function of the operated compared with the nonoperated knees except for anterior, painless crepitation in 8 patients. This was thought to be related to fibrosis of the Hoffa body. Regarding the predictive power of the questionnaires, the question arises as to how accurately the patient answers reflect reality. It may be that the patients have become so accustomed to the physical circumstances over the past 10 years that they consider their current conditions to be normal, when in fact they are not. At present, however, the results reflect a reality of no relevant impairment of the operated side.
MRI showed atrophy of the quadriceps muscle on the operated side in 10 of 13 cases, which could be the reason for the difference in strength. On the one hand, the atrophy could be pre-existing due to the congenital deformity with altered biomechanics because of the shortened bone in our patients (8 of 13 patients) (20). On the other hand, a previous biomechanical study showed a weakening effect of intramedullary lengthening on muscle strength. In this study, in the first 2 years after the procedure a significant difference remained for the maximum isokinetic torque of the extensors (22% lower in the lengthened leg, preoperatively this difference was already 15%) (21). This may be inferred from the response of the muscle to the distraction procedure itself, in terms of higher stiffness, less immediate displacement, and inconsistent force relaxation properties. It was therefore considered that physiotherapy after limb lengthening should focus primarily on the extensor muscles to compensate for strength losses (21). In both the present and the above-mentioned study, the loss of strength was not evident in the clinical parameters or in the gait pattern.
We consider a further study after another 10 years to be useful, to further evaluate the potential predictive value of the MRI findings. Tan et al. (22) reported knee stiffness and patellar tendon ossification after the retrograde femoral approach for fracture treatment with an intramedullary nail. Court-Brown et al. (23) reported the same complications in tibial fracture repair with an intramedullary nail. Our patients showed neither ossification of the patellar tendon nor knee stiffness. However, our patient population had a different elective indication and no previous knee trauma.
Overall, contrary to some previous authors (24), we believe surgery with an intramedullary nail for leg lengthening using a retrograde approach may be a good option. Lee et al. (24) discourage surgery with the ISKD nail as patients experienced many complications and severe pain. Our group of patients received a motorized nail with specific instruments, and we do not confirm that study’s concerns. Our patient cohort did not show relevant clinical impairment in daily activities 10 years after surgery. However, radiologically visible defects are still evident not only after 2 years (19) but also after 10 years. Hammouda et al. (25) found no major risks with the antegrade femoral approach. This is also true for the retrograde approach (26).
Strengths and limitations
A unique feature of this study is the control group in the form of the opposite side in the same individual. Also, the examinations and clinical tests were performed by trained personnel, who had no direct interests in the study outcome or involvement in the treatment of the patients. However, this study has limitation. First and foremost, a small number of patients was reported. Due to this being a relatively new surgical technique in Switzerland, there are not many patients yet in whom this operation was performed more than 10 years ago. Second, we did not include a control group that received leg lengthening with a different surgical approach, thus not allowing for comparison between techniques. Third, 10 years is a long time interval. Consequently, other patient lifestyle-related factors can contribute to general and joint health. Finally, a diagnostic MRI protocol was used. Advanced, quantitative MRI sequences may be able to provide further insight into cartilage status and facilitate comparisons.
Conclusion
Our study showed cartilage defects at the entry point, Hoffa’s arthrofibrosis, and mild atrophy of the quadriceps femoris muscle. However, after 10 years’ follow-up these changes did not cause any clinically relevant impairment.
- Dahl M T, Gulli B, Berg T. Complications of limb lengthening: a learning curve. Clin Orthop Relat Res 1994; (301): 10-18. doi: 10.1097/00003086-199404000-00003.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 1990; 250: 81-104. doi: 10.5005/jp/books/12869_156.
- Lenze U, Krieg A H. Intramedullary lengthening nails: can we also correct deformities? J Child Orthop 2016; 10(6): 511-16. doi: 10.1007/s11832-016-0782-0.
- Krieg A H, Speth B M, Foster B K. Leg lengthening with a motorized nail in adolescents. Clin Orthop Relat Res 2008: 466(1): 189-97. doi: 10.1007/s11999-007-0040-3.
- Calder P R, McKay J E, Timms A J, Roskrow T, Fugazzotto S, Edel P, et al. Femoral lengthening using the Precice intramedullary limb-lengthening system: outcome comparison following antegrade and retrograde nails. Bone Joint J 2019; 101(9): 1168-76. doi: 10.1302/0301-620x.101b9.bjj-2018-1271.r1.
- Fragomen A T, Rozbruch S R. Lengthening of the femur with a remote-controlled magnetic intramedullary nail: retrograde technique. JBJS Essent Surg Tech 2016; 6(2): e20. doi: 10.2106/jbjs.st.15.00069.
- Herscovici Jr D, Whiteman K. Retrograde nailing of the femur using an intercondylar approach. Clin Orthop Relat Res 1996; (332): 98. doi: 10.1097/00003086-199611000-00013.
- Ostrum R F, DiCicco J, Lakatos R, Poka A. Retrograde intramedullary nailing of femoral diaphyseal fractures. J Orthop Trauma 1998; 12(7): 464-8. doi: 10.1097/00005131-199809000-00006.
- Accadbled F, Pailhé R, Cavaignac E, Sales de Gauzy J. Bone lengthening using the Fitbone® motorized intramedullary nail: the first experience in France. Orthop Traumatol Surg Res 2016; 102(2): 217-22. doi: 10.1016/j.otsr.2015.10.011.
- Oezcan Ç, Sökücü S, Beng K, Çetinkaya E, Demir B, Kabukçuoğlu Y S. Prospective comparative study of two methods for fixation after distal femur corrective osteotomy for valgus deformity; retrograde intramedullary nailing versus less invasive stabilization system plating. Int Orthop 2016; 40(10): 2121-6. doi: 10.1007/s00264-016-3190-7.
- Hierholzer C, von Rüden C, Pötzel T, Woltmann A, Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: a retrospective analysis. Indian J Orthop 2011; 45(3): 243-50. doi: 10.4103/0019-5413.80043.
- Kim J-W, Oh C-W, Oh J-K, Park K-H, Kim H-J, Kim T-S, et al. Treatment of infra-isthmal femoral fracture with an intramedullary nail: is retrograde nailing a better option than antegrade nailing? Arch Orthop Trauma Surg 2018; 138(9): 1241-7. doi: 10.1007/s00402-018-2961-6.
- Baumgart R. The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction. Oper Orthop Traumatol 2009; 21(2): 221-33. doi: 10.1007/s00064-009-1709-4.
- Ware J, Bierman A, Gandek B, Sinclair S, Lawrence W. Comparison of SF-36 summary and preference-based utility scores across groups differing in disease severity: results from the Medicare health outcomes survey. Value in Health 2003; 6(3): 304. doi: 10.1016/s1098-3015(10)64112-5.
- Higgins L D, Taylor M K, Park D, Ghodadra N, Marchant M, Pietrobon R, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) subjective knee form. Joint Bone Spine 2007; 74(6): 594-9. doi: 10.1016/j.jbspin.2007.01.036.
- Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982; 10(3): 150-4. doi: 10.1177/036354658201000306.
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985; (198): 43-9. doi: 10.1097/00003086-198509000-00007.
- Dipaola J D, Nelson D W, Colville M R. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 1991; 7(1): 101-4. doi: 10.1016/0749-8063(91)90087-e.
- Anderson A F, Irrgang J J, Kocher M S, Mann B J, Harrast J J. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med 2006; 34(1): 128-35. doi: 10.1177/0363546505280214.
- Pirani S, Beauchamp R D, Li D, Sawatzky B. Soft tissue anatomy of proximal femoral focal deficiency. J Pediatr Orthop 1991; 11(5): 563-70. doi: 10.1097/01241398-199109000-00001.
- Krieg A H, Gehmert S, Neeser O L, Kaelin X, Speth B M. Gain of length-loss of strength? Alteration in muscle strength after femoral leg lengthening in young patients: a prospective longitudinal observational study. J Pediatr Orthop B 2018; 27(5): 399-403. doi: 10.1097/bpb.0000000000000479.
- Tan L, Wang T, Li Y-H, Yang T, Hao B, Zhu D, et al. Patellar tendon ossification after retrograde intramedullary nailing for distal femoral shaft fracture: a case report and review of the literature. Medicine (Baltimore) 2017; 96(47): e8875. doi: 10.1097/md.0000000000008875.
- Court-Brown C M, Will E, Christie J, McQueen M M. Reamed or unreamed nailing for closed tibial fractures: a prospective study in Tscherne C1 fractures. J Bone Joint Surg Br 1996; 78(4): 580-3. doi: 10.1302/0301-620x.78b4.0780580.
- Lee D H, Ryu K J, Song H R, Han S-H. Complications of the Intramedullary Skeletal Kinetic Distractor (ISKD) in distraction osteogenesis. Clin Orthop Relat Res 2014; 472(12): 3852-9. doi: 10.1007/s11999-014-3547-4.
- Hammouda A I, Jauregui J J, Gesheff M G, Standard S C, Herzenberg J E. Trochanteric entry for femoral lengthening nails in children: is it safe? J Pediatr Orthop 2017; 37(4): 258-64. doi: 10.1097/bpo.0000000000000636.
- Krieg A H, Lenze U, Speth B M, Hasler C C. Intramedullary leg lengthening with a motorized nail: indications, challenges, and outcome in 32 patients. Acta Orthop 2011; 82(3): 344-50. doi: 10.3109/17453674.2011.584209.